Abstract
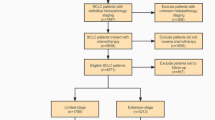
Despite the increasing incidence of combined small-cell lung cancer (C-SCLC) in recent years, there have not been many data on clinical prognostic factors predicting prognosis of C-SCLC patients. In present study, we sought pretreatment features especially basic laboratory parameters predicting survival of C-SCLC. We analyzed 613 small-cell lung cancer (SCLC) patients at our institution between January 2005 and December 2010. We identified 114 patients with C-SCLC. The pathologic and clinical characteristics of these patients were reviewed. Data of laboratory parameters obtained during regular examinations at diagnosis of these patients were examined. The Kaplan–Meier method was used to calculate the survival rate and depict the survival curves. The Cox regression model was used to analyze the independent factors affecting the overall survival (OS). These data were compared with the results obtained from our 499 pure SCLC patients who presented during the same time period. Of the 613 SCLC patients analyzed, 18.6 % of the patients presented with C-SCLC. No difference in OS was observed in patients with C-SCLC and patients with pure SCLC (P = 0.995). The Kaplan–Meier survival curves revealed that poor ECOG-PS (P < 0.001), extensive disease (P < 0.001), pathologic subtype of SC/LC (P < 0.001), not receiving surgery (P = 0.001), elevated serum lactate dehydrogenase (LDH) (P = 0.005), elevated NSE (P = 0.043), and elevated neutrophile–lymphocyte ratio (NLR) (P = 0.018) were associated with adverse prognosis of patients with C-SCLC. By multivariate analysis, OS was affected by ECOG-PS (hazard ratio 2.001, P = 0.012), disease extent (hazard ratio 3.406, P < 0.001), and NLR (hazard ratio 1.704, P = 0.030) in C-SCLC patients, while the risk factors that influenced the prognosis of the patients with pure SCLC were ECOG-PS (hazard ratio 2.132, P < 0.001), disease extent (hazard ratio 1.482, P < 0.001), and LDH (hazard ratio 1.811, P < 0.001). Patients with C-SCLC carry a similar prognosis than those with pure small-cell variety. Easily accessible pretreatment parameters such as NLR should be considered in defining the prognosis of C-SCLC patients besides disease extent and performance status.



Similar content being viewed by others
References
Govindan, R., et al. (2006). Changing epidemiology of small-cell lung cancer in the United States over the last 30 years: analysis of the surveillance, epidemiologic, and end results database. Journal of Clinical Oncology, 24(28), 4539–4544.
Osterlind, K., & Andersen, P. K. (1986). Prognostic factors in small cell lung cancer: multivariate model based on 778 patients treated with chemotherapy with or without irradiation. Cancer Research, 46(8), 4189–4194.
Maestu, I., et al. (1997). Pretreatment prognostic factors for survival in small-cell lung cancer: a new prognostic index and validation of three known prognostic indices on 341 patients. Annals of Oncology, 8(6), 547–553.
Kawahara, M., et al. (1997). Prognostic factors and prognostic staging system for small cell lung cancer. Japanese Journal of Clinical Oncology, 27(3), 158–165.
Cerny, T., et al. (1987). Pretreatment prognostic factors and scoring system in 407 small-cell lung cancer patients. International Journal of Cancer, 39(2), 146–149.
Souhami, R. L., et al. (1985). Prognostic significance of laboratory parameters measured at diagnosis in small cell carcinoma of the lung. Cancer Research, 45(6), 2878–2882.
Rawson, N. S., & Peto, J. (1990). An overview of prognostic factors in small cell lung cancer. A report from the subcommittee for the management of lung cancer of the United Kingdom coordinating committee on cancer research. British Journal of Cancer, 61(4), 597–604.
Dearing, M. P., et al. (1990). Outcome of patients with small-cell lung cancer: effect of changes in staging procedures and imaging technology on prognostic factors over 14 years. Journal of Clinical Oncology, 8(6), 1042–1049.
Paesmans, M., et al. (2000). Prognostic factors for patients with small cell lung carcinoma: analysis of a series of 763 patients included in 4 consecutive prospective trials with a minimum follow-up of 5 years. Cancer, 89(3), 523–533.
Teramukai, S., et al. (2009). Pretreatment neutrophil count as an independent prognostic factor in advanced non-small-cell lung cancer: an analysis of Japan multinational trial organisation LC00-03. European Journal of Cancer, 45(11), 1950–1958.
Sarraf, K. M., et al. (2009). Neutrophil/lymphocyte ratio and its association with survival after complete resection in non-small cell lung cancer. Journal of Thoracic and Cardiovascular Surgery, 137(2), 425–428.
Lee, S., et al. (2013). Prognostic significance of neutrophil lymphocyte ratio and platelet lymphocyte ratio in advanced gastric cancer patients treated with FOLFOX chemotherapy. BMC Cancer, 13, 350.
McMillan, D. C. (2009). Systemic inflammation, nutritional status and survival in patients with cancer. Current Opinion in Clinical Nutrition and Metabolic Care, 12(3), 223–226.
He, W., et al. (2013). Initial neutrophil lymphocyte ratio is superior to platelet lymphocyte ratio as an adverse prognostic and predictive factor in metastatic colorectal cancer. Medical Oncology, 30(1), 439.
Azab, B., et al. (2013). Pretreatment neutrophil/lymphocyte ratio is superior to platelet/lymphocyte ratio as a predictor of long-term mortality in breast cancer patients. Medical Oncology, 30(1), 432.
Lee, Y., et al. (2009). Early neutrophil-to-lymphocyte ratio reduction as a surrogate marker of prognosis in never smokers with advanced lung adenocarcinoma receiving gefitinib or standard chemotherapy as first-line therapy. Journal of Cancer Research and Clinical Oncology, 138(12), 2009–2016.
Travis, W. D., et al. (2004). Tumours of the lung, pleura, thymus and heart: world health organization: international histological classification of tumours. Lyon: IARC Press.
Adelstein, D. J., et al. (1986). Mixed small cell and non-small cell lung cancer. Chest, 89(5), 699–704.
Mangum, M. D., et al. (1989). Combined small-cell and non-small-cell lung cancer. Journal of Clinical Oncology, 7(5), 607–612.
Nicholson, S. A., et al. (2002). Small cell lung carcinoma (SCLC): a clinicopathologic study of 100 cases with surgical specimens. American Journal of Surgical Pathology, 26(9), 1184–1197.
Hage, R., et al. (1998). Surgery for combined type small cell lung carcinoma. Thorax, 53(6), 450–453.
Babakoohi, S., et al. (2012). Combined SCLC clinical and pathologic characteristics. Clinical Lung Cancer, 14(2), 113–119.
Kim, Y. H., Mishima, M., & Date, H. (2013). “Combined” small cell and “pure” small cell lung cancer: is there a clinical difference? Medical Oncology, 30(2), 600.
Tatematsu, A., et al. (2008). Epidermal growth factor receptor mutations in small cell lung cancer. Clinical Cancer Research, 14(19), 6092–6096.
Cedres, S., et al. (2012). Neutrophil to lymphocyte ratio (NLR) as an indicator of poor prognosis in stage IV non-small cell lung cancer. Clinical and Translational Oncology, 14(11), 864–869.
Tomita, M., et al. (2011). Preoperative neutrophil to lymphocyte ratio as a prognostic predictor after curative resection for non-small cell lung cancer. Anticancer Research, 31(9), 2995–2998.
Acknowledgments
This work was supported by grants from the National Natural Science Foundation of China (Nos. 81372517 and 81000899), the Tianjin Municipal Science and Technology Commission Key Application Research Projects (No. 11JCZDJC18900), and the Science Foundation of Tianjin Health Bureau (No. 2010KZ78)
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Xinyue Wang and Richeng Jiang contributed equally to this study.
Rights and permissions
About this article
Cite this article
Wang, X., Jiang, R. & Li, K. Prognostic Significance of Pretreatment Laboratory Parameters in Combined Small-Cell Lung Cancer. Cell Biochem Biophys 69, 633–640 (2014). https://doi.org/10.1007/s12013-014-9845-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-014-9845-3