Abstract
Objective
Conventionally, the bidirectional Glenn procedure (BDG) is performed on cardiopulmonary bypass (CPB) using aortobicaval cannulation. This study discusses the procedural details of open anastomosis technique of the BDG and outcomes.
Method
Between September 2013 and November 2014, 15 patients (age 49 ± 47.9 months, weight 14.1 ± 10.3 kg) underwent BDG using the open technique (OT). CPB was instituted by aortic cannulation and a single venous cannula in the right atrium. Superior vena cava (SVC) was not cannulated and all the venous return from it was returned via a cardiotomy sucker. This facilitated an open anastomosis. Parameters studied were CPB time, Glenn pressure, SVC clamp time, neurocognitive score, near-infrared spectrometry (NIRS), inotropic score, SpO2, intensive care unit (ICU) stay, hospital stay and immediate complications.
Results
Saturation increased from pre-operative 64 to 87 % after operation. Post-operative Glenn pressure was 15 ± 3.8 mmHg. CPB time was 28.6 ± 17.4 min, inotropic score was 8.0 ± 2.5, duration of ventilator support was 8.8 ± 3.6 h, ICU stay was 17.78 ± 3.14 h and hospital stay was 4.4 ± 0.5 days. There was progressive increase of the neurocognitive function post-operatively. NIRS monitoring showed no significant drop in values from base line level in OT group suggesting adequate cerebral perfusion. There were no deaths or major morbidity.
Conclusions
BDG can be performed quickly and safely with open anastomosis technique on CPB.
Similar content being viewed by others
Introduction
The bidirectional Glenn shunt (BDG) consists of an end-to-side anastomosis between the superior vena cava (SVC) and the right pulmonary artery (RPA). It is a well-established palliative surgical procedure in patients with a univentricular heart and is performed in younger patients as a staged procedure or in older patients as a part of single-stage total cavopulmonary connection [1]. Commonly this procedure is performed with the support of cardiopulmonary bypass (CPB), although many including us have popularized the BDG without the use of CPB [2, 3]. When the procedure is performed on CPB, aortobicaval cannulation is usually performed. In this report, we present our alternative technique of open anastomosis of BDG without cannulating the SVC. Early results are presented. This technique was used initially by the Mee group from Melbourne and later Cleveland but was never published by them to the best of our knowledge.
Methods
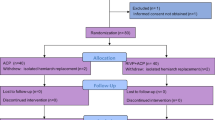
This prospective study was carried out at All India Institute of Medical Sciences, New Delhi, between September 2013 to November 2014. Fifteen patients had the procedure performed with CPB support by a single surgeon (ST). Informed consent was obtained from parents of all the patients and the study protocol was approved by the institute ethics committee. Patient profile is listed in Table 1.
Mean age at operation was 49 ± 47.9 months (range = 10–192 months, median = 36 months). The commonest diagnosis was tricuspid atresia with ventricular septal defect and pulmonary stenosis (TA, VSD, PS) in 7 of the 15 patients. Mean pre-operative systemic saturation (SpO2) was 64 ± 0.08 % (range = 53–80 %, median = 63 %). Two patients had earlier undergone modified Blalock-Taussig shunt (BT shunt) via thoracotomy: one on right side and another on left side. Both shunts were patent. No patient needed intracardiac procedure or pulmonary artery (PA) plasty as a part of BDG. A concomitant PA plasty was, however, not considered a contraindication to this technique.
All patients had a small cannula placed in the internal jugular vein on the side of the SVC for monitoring the pressure in the SVC. Invasive arterial pressure monitoring line and central venous access was achieved by an arterial cannula and a triple-lumen catheter in the femoral artery and vein, respectively. Near-infrared spectroscopy (NIRS) was monitored for adequacy of cerebral perfusion. Bispectral index (BIS) was monitored for the depth of anaesthesia. Operating room temperature was kept cool to ensure cerebral protection. Ventilation was adjusted in a manner to achieve PaCo2 between 40 and 45 mmHg. Elective dopamine was started (5 mcg/kg/min) prior to weaning off CPB.
Technique
All procedures were performed via the median sternotomy approach. The thymus was excised partially or completely. The pericardium was opened in the midline and stay sutures were placed. Anatomy was assessed, particularly the confluence and adequacy of pulmonary arteries. LSVC was looked for in every case. Marking sutures using 6-0 polypropylene were placed on the SVC on both the medial and lateral aspects where it was expected to align to the left and the right angles respectively of the arteriotomy in the right pulmonary artery (RPA). This ensures proper orientation and prevents anastomotic distortion after SVC transection. After systemic heparinisation, normothermic CPB was established by aortic cannulation and a single right-angled cannula in the right atrial appendage. The SVC was dissected and mobilized completely and the azygous vein was ligated and divided. The branch pulmonary arteries were dissected and mobilized.
The SVC was clamped near the SVC-RA junction avoiding injury to the SA node, and a cardiotomy sucker was placed in SVC immediately and secured in place by the first assistant. The suction on the cardiotomy sucker was increased to ensure proper drainage of blood from the SVC into the sucker. The transected cardiac end of SVC was oversewn with 6-0 prolene and the clamp removed. An appropriate size arteriotomy was made in the right pulmonary artery between stay sutures, and the cephalad end of the transected SVC was anastomosed to it using a continuous 6-0 polypropylene suture (Fig. 1). During the entire anastomosis construction, cardiotomy sucker was kept in SVC ensuring that it was patent and was removed only during completion of the Glenn anastomosis.
Figure shows the technique of open anastomosis during Glenn. The superior vena cava (SVC) has been transected and a cardiotomy sucker (CS) is placed into it. The SVC is anastomosed end-to-side to the right pulmonary artery (RPA). A clamp (C) has been placed at the cardiac end of the SVC which can be closed prior to or after the Glenn
SVC pressure, systolic blood pressure, O2 saturation and NIRS were monitored during the entire procedure. During the entire procedure, SVC pressures were low and in the range of 0–3, which are significantly low when compared to the other standard techniques like SVC cannulation or intermittent clamping of the SVC. After completion of the anastomosis, the patients were weaned off CPB. Rest of the operation proceeded as per any routine procedure.
In the intensive care unit (ICU), the cannula in the internal jugular vein was removed once the patient was stabilized. The patients were weaned off mechanical ventilatory support and inotropes as early as possible. Inotropic score was calculated for each patient using the formula described by Wernovsky et al. [4]: dopamine (mcg/kg/min) + dobutamine (mcg/kg/min) + 100 × epinephrine (mcg/kg/min). Low-dose anti-platelet therapy (Aspirin—5 mcg/kg/day) was started on post-op day 1 and continued indefinitely. After discharge from the hospital, at each follow-up visit, all patients underwent detailed neurocognitive evaluation with the help of Vineland Social Maturity Scale [5, 6]. These scores were compared with the pre-operative scores for any subjective evidence of deterioration in neurocognitive function.
Results
There were no early deaths. No patient required re-operation or revision of the procedure. Post-op SpO2 improved significantly with the mean SpO2 being 87 ± 0.06 % (range = 70–96 %, median 88 %). Mean post-operative Glenn pressure 15.3 ± 3.9 (range 7–22, median = 15). The mean CPB time was 28.7 ± 17.3 min (range = 8–70 min, median = 22 min). There was no hemodynamic instability during any of the procedures, and adequate cerebral oxygenation was maintained throughout the procedure as indicated by the NIRS values. The mean ventilator support duration was 8.8 ± 3.6 h (range = 4–16 h, median = 7 h). The mean ICU stay was 17.78 ± 3.14 h (range = 14–24, median = 16 h)—Table 2. There was no decline in neurocognitive function in any of the patients in the ICU or in the immediate post-op period. All patients made an uneventful post-operative recovery and were discharged within 4 days of the procedure (mean = 4.4 ± 0.5, range = 4–5 days, median = 4.5 days). All patients underwent post-op 2D Echo before discharge which was suggestive of well-functioning BDG with laminar flow. At a mean follow-up of 6.5 ± 5.06 months (range = 1–15, median = 4 months), all patients were doing well with no neurological sequelae.
Discussion
Classic Glenn shunt was performed through a thoracotomy without CPB [7]; however, the distribution was not bidirectional. BDG reduces the ventricular volume overload and improves peripheral saturation with improvement in functional class [8]. It is not always feasible to perform BDG without CPB support, such situations being smaller patients (<5 kg), deep cyanosis, SVC too small to cannulate, concomitant need of extensive PA plasty due to previous shunts [9], emergency procedures due to blocked BT shunt or child with recurrent cyanotic spells or inpatients with anomalies of cardiac situs and position as in heterotaxy syndromes. In such situations, BDG is preferably performed with CPB support and we have found the “open technique” useful.
The main advantage of this open technique of BDG is that there is no need of cannulating or clamping the SVC. With cannulation of the SVC, there is always some traction on the SVC which hinders the performance of the anastomosis and also the snugger around the cannula may lead to distortion of the SVC and may create anastomosis distortion. While tying the purse string on the SVC, there is always the risk of SVC narrowing and even small gradients at the SVC are not tolerated well in the venous circuit by patients undergoing univentricular palliation. With technique of intermittent clamping that is often used to avoid SVC cannulation in small babies, there is always a risk of impairment of cerebral venous drainage even though it is transient and it may lead to impaired neurocognitive development. On the other hand, with the open technique, the SVC drainage is unobstructed and there is no risk of neurological issues. The operation is performed with an open undistorted SVC, so there is no risk of anastomotic distortion.
We have been regularly performing this procedure for more than 5 years now with gratifying early and mid-term results.
Assessment of neurological outcome has always been difficult. We used Vineland Social Maturity Scale [5, 6] to evaluate the effect of open technique BDG procedure in our children, and no children had any deterioration of neurological function in the immediate post-operative or early follow-up period.
Study limitations
This study is an initial experience of a small number of patients operated using the “open technique”, and no comparisons have been made with the standard aortobicaval technique and the intermittent SVC clamping technique. To address this issue, a randomized study comparing the three techniques is already in progress and the results of that study will be reported later.
To conclude, in spite of the relatively small sample size, this study suggests that BDG operation can be performed safely, quickly and reliably with the open technique.
References
Duncan BW, Desai S. Pulmonary arteriovenous malformations after cavopulmonary anastomosis. Ann Thorac Surg. 2003;76:1759–66.
Liu J, Lu Y, Chen H, Shi Z, Su Z, Ding W. Bidirectional Glenn procedure without cardiopulmonary bypass. Ann Thorac Surg. 2004;77:1349–52.
Talwar S, Sharma P, Kumar TKS, Choudhary SK, Gharde P, Airan B. Bidirectional superior cavo-pulmonary anastomosis without cardiopulmonary bypass. Indian J Thorac Cardiovasc Surg. 2008;24:269–76.
Wernovsky G, Wypij D, Jonas RA, et al. Postoperative course and hemodynamic profile after the arterial switch operation in neonates and infants. A comparison of low-flow cardiopulmonary bypass and circulatory arrest. Circulation. 1995;92:2226–35.
Hurst JG. The meaning and use of different scores between the performance on the Stanford-Binet intelligence scale and Vineland Social Maturity Scale. J Clin Psychol. 1962;18:153–60.
Arya S Developmental screening of preschool children: an overview. Indian J Disabil Rehabil. 1987;1:6–22.
Glenn WWL. Circulatory bypass of the right side of the heart. IV. Shunt between superior vena cava and distal right pulmonary artery- report of clinical application. N Engl J Med. 1958;259:117–20.
Reddy MV, Liddicoat JR, Hanley FL. Primary bidirectional superior cavopulmonary shunt in infants between 1 and 4 months of age. Ann Thorac Surg. 1995;59:1120–6.
Lamberti JJ, Spicer RL, Waldman JD, et al. The bidirectional cavopulmonary shunt. J Thorac Cardiovasc Surg. 1990;100:22–30.
Conflict of interest
All authors declare that they have no competing interests and do not receive any research grants from any company, have not received a speaker honorarium from any company, do not own any stock in any company and are not members of a committee.
Compliance with ethical standards
ᅟ
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Talwar, S., Kumar, M.V., Makhija, N. et al. Bidirectional Glenn: open technique of anastomosis on cardiopulmonary bypass. Indian J Thorac Cardiovasc Surg 31, 209–212 (2015). https://doi.org/10.1007/s12055-015-0379-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-015-0379-0