Abstract
Introduction
This study was designed to evaluate the efficacy and safety of 3% diquafosol ophthalmic solution in dry eye patients in clinical practice.
Methods
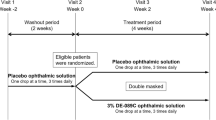
Subjects were dry eye patients who had never used diquafosol, and observation was conducted prospectively over 2 months. The corneal and conjunctival fluorescein staining score, tear film break-up time, 12 dry eye-related subjective symptoms, patient-reported outcomes, and adverse events were investigated.
Results
Data were collected from 465 medical institutions for 3,196 patients. Diquafosol led to significant improvement in all subjective symptoms and objective findings (P < 0.001, paired t test). Diquafosol was effective regardless of the degree of severity according to the corneal and conjunctival fluorescein staining score or therapeutic pattern. Overall, 76.0% patients responded that their condition had improved. Adverse reactions were observed in 6.3% of patients. The major adverse reactions were eye discharge, eye irritation, and eye pain.
Conclusion
Diquafosol was effective for various dry eye patients in clinical practice, and no significant safety-related problems occurred.






Similar content being viewed by others
References
Shimazaki J. Dry Eye Research Group. Diagnostic criteria of dry eye 2006 [in Japanese]. Atarashii Ganaka (J Eye). 2007;24:181–4.
The Definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of International Dry Eye Work Shop. Ocul Surf. 2007;5:75–92.
Uchino M, Schaumberg DA, Dogru M, et al. Prevalence of dry eye disease among Japanese visual display terminal users. Ophthalmology. 2008;115:1982–8.
Albietz JM. Prevalence of dry eye subtypes in clinical optometry practice. Optom Vis Sci. 2000;77:357–63.
Murakami T, Fujihara T, Horibe Y, Nakamura M. Diquafosol elicits increases in net Cl- transport through P2Y2 receptor stimulation in rabbit conjunctiva. Ophthalmic Res. 2004;36:89–93.
Murakami T, Fujihara T, Nakamura M, Nakata K. P2Y(2) receptor elicits PAS-positive glycoprotein secretion from rabbit conjunctival goblet cells in vivo. J Ocul Pharmacol Ther. 2003;19:345–52.
Cowlen MS, Zhang VZ, Warnock L, Moyer CF, Peterson WM, Yerxa BR. Localization of ocular P2Y2 receptor gene expression by in situ hybridization. Exp Eye Res. 2003;77:77–84.
Hosoya K, Ueda H, Kim K, Lee VHL. Nucleotide stimulation of Cl− secretion in the pigmented rabbit conjunctiva. J Pharmacol Exp Ther. 1999;291:53–9.
Li Y, Kuang K, Yerxa B, Quan W, Rosskothen H, Fischbarg J. Rabbit conjunctival epithelium transports fluid, and P2Y2 receptor agonists stimulate Cl− and fluid secretion. Am J Physiol Cell Physiol. 2001;281:C595–602.
Jumblatt JE, Jumblatt MM. Regulation of ocular mucin secretion by P2Y2 nucleotide receptors in rabbit and human conjunctiva. Exp Eye Res. 1998;67:341–6.
Matsumoto Y, Ohashi Y, Watanabe H, Tsubota K. Diquafosol Ophthalmic Solution Phase 2 Study Group. Efficacy and safety of diquafosol ophthalmic solution in patients with dry eye syndrome: a Japanese phase 2 clinical trial. Ophthalmology. 2012;119:1954–60.
Takamura E, Tsubota K, Watanabe H, Ohashi Y. Diquafosol Ophthalmic Solution Phase 3 Study Group. A randomized, double-masked comparison study of diquafosol versus sodium hyaluronate ophthalmic solutions in dry eye patients. Br J Ophthalmol. 2012;96:1310–5.
Yamaguchi M, Tsubota K, Watanabe H, Ohashi Y. The safety and efficacy of long-term treatment with 3% diquafosol ophthalmic solution for dry eye [in Japanese]. Atarashii Ganaka (J Eye). 2012;29:527–35.
Koh S, Watanabe H, Hosohata J, et al. Diagnosing dry eye using a blue-free barrier filter. Am J Ophthalmol. 2003;136:513–9.
Miljanovic B, Dana R, Sullivan DA, Schaumberg DA. Impact of dry eye syndrome on vision-related quality of life. Am J Ophthalmol. 2007;143:409–15.
Nakamura M, Mishima H, Nishida T, Otori T. Binding of hyaluronan to plasma fibronectin increases the attachment of corneal epithelial cells to a fibronectin matrix. J Cell Physiol. 1994;159:415–22.
Nakamura M, Nishida T, Hikida M, Otori T. Combined effects of hyaluronan and fibronectin on corneal epithelial wound closure of rabbit in vivo. Curr Eye Res. 1994;13:385–8.
Nakamura M, Hikida M, Nakano T, Ito S, Hamano T, Kinoshita S. Characterization of water retentive properties of hyaluronan. Cornea. 1993;12:433–6.
Yokoi N, Kato H, Kinoshita S. Facilitation of tear fluid secretion by 3% diquafosol ophthalmic solution in normal human eyes. Am J Ophthalmol. 2014;157:85–92.
Shimazaki-Den S, Iseda H, Dogru M, Shimazaki J. Effects of diquafosol sodium eye drops on tear film stability in short BUT type of dry eye. Cornea. 2013;32:1120–5.
Management and therapy of dry eye disease: report of the management and therapy of the international dry eye workshop (2007). Ocul Surf. 2007;5:163–178.
Mathers WD. Ocular evaporation in meibomian gland dysfunction and dry eye. Ophthalmology. 1993;100:347–51.
Paranjpe DR, Foulks GN. Therapy for meibomian gland disease. Ophthalmol Clin North Am. 2003;16:37–42.
Arita R, Suehiro J, Haraguchi T, et al. Topical diquafosol for patients with obstructive meibomian gland dysfunction. Br J Ophthalmol. 2013;97:725–9.
Sakane Y, Yamaguchi M, Yokoi N, et al. Development and validation of dry eye-related quality-of-life score questionnaire. JAMA Opthalmol. 2013;131:1331–8.
Acknowledgments
Sponsorship and article processing charges for this study were funded by Santen Pharmaceutical Co., Ltd. Osaka, Japan. All named authors meet the ICMJE criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published. All authors had full access to all of the data in this study and Takeshi Nishijima takes complete responsibility for the integrity of the data and accuracy of the data analysis.
Conflict of interest
Masahiko Yamaguchi has received honoraria for medical advice on this study and honoraria for writing and reviewing this manuscript from Santen. Takeshi Nishijima is an employee of Santen. Jun Shimazaki has received honoraria for medical advice on this study from Santen, and consulting fees from Otsuka and honoraria for lectures from Abbot, Alcon, Novartis, Otsuka, and Santen. Etsuko Takamura has received honoraria for medical advice on this study from Santen, and consulting fees from Alcon, Astellas, GlaxoSmithKline, Kissei, Kyowa Hakko Kirin, Maruho, MSD, Nippon Boehringer Ingelheim, Novartis, Otsuka, Pfizer, Senju, and Wakamoto. Norihiko Yokoi has received honoraria for medical advice on this study from Santen, and consulting fees from Kissei and Rohto. Hitoshi Watanabe has received honoraria for medical advice on this study from Santen. Yuichi Ohashi has received honoraria for medical advice on this study from Santen, and consulting fees from HOYA, Johnson and Johnson, Otsuka, Santen, and Senju.
Compliance with ethics guidelines
This study was conducted on the basis of a request from a regulatory agency in Japan. It was a multi-institutional, prospective, non-interventional, observational study that conformed to the Good Post-Marketing Study Practice (Ministry of Health, Labor and Welfare ordinance 171, December 20, 2004). The study protocol was reviewed and approved in advance by the Pharmaceuticals and Medical Devices Agency, Japan. For this reason, no ethical review by the individual facilities participating in the study was conducted. Because informed consent was not required for post-marketing observational studies that were requested by the regulatory agency in Japan, the present study did not solicit informed consent from the patients.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yamaguchi, M., Nishijima, T., Shimazaki, J. et al. Clinical Usefulness of Diquafosol for Real-World Dry Eye Patients: A Prospective, Open-Label, Non-Interventional, Observational Study. Adv Ther 31, 1169–1181 (2014). https://doi.org/10.1007/s12325-014-0162-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-014-0162-4