Abstract
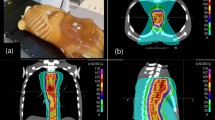
To quantify the dose calculation error and resulting optimization uncertainty caused by performing inverse treatment planning on inaccurate electron density data (pseudo-CT) as needed for adaptive radiotherapy and Magnetic Resonance Imaging (MRI) based treatment planning. Planning Computer Tomography (CT) data from 10 cervix cancer patients was used to generate 4 pseudo-CT data sets. Each pseudo-CT was created based on an available method of assigning electron density to an anatomic image. An inversely modulated radiotherapy (IMRT) plan was developed on each planning CT. The dose calculation error caused by each pseudo-CT data set was quantified by comparing the dose calculated each pseudo-CT data set with that calculated on the original planning CT for the same IMRT plan. The optimization uncertainty introduced by the dose calculation error was quantified by re-optimizing the same optimization parameters on each pseudo-CT data set and comparing against the original planning CT. Dose differences were quantified by assessing the Equivalent Uniform Dose (EUD) for targets and relevant organs at risk. Across all pseudo-CT data sets and all organs, the absolute mean dose calculation error was 0.2 Gy, and was within 2 % of the prescription dose in 98.5 % of cases. Then absolute mean optimisation error was 0.3 Gy EUD, indicating that that inverse optimisation is impacted by the dose calculation error. However, the additional uncertainty introduced to plan optimisation is small compared the sources of variation which already exist. Use of inaccurate electron density data for inverse treatment planning results in a dose calculation error, which in turn introduces additional uncertainty into the plan optimization process. In this study, we showed that both of these effects are clinically acceptable for cervix cancer patients using four different pseudo-CT data sets. Dose calculation and inverse optimization on pseudo-CT is feasible for this patient cohort.



Similar content being viewed by others
References
Verellen D et al (2007) Innovations in image-guided radiotherapy. Nat Rev Cancer 7(12):949–960
Hoogcarspel SJ et al (2014) The feasibility of utilizing pseudo CT-data for online MRI based treatment plan adaptation for a stereotactic radiotherapy treatment of spinal bone metastases. Phys Med Biol 59(23):7383
Metcalfe P et al (2013) The potential for an enhanced role for MRI in radiation-therapy treatment planning. Technol Cancer Res Treat 12(5):429–446
de la Zerda A, Armbruster B, Xing L (2007) Formulating adaptive radiation therapy (ART) treatment planning into a closed-loop control framework. Phys Med Biol 52(14):4137
Lambert J et al (2011) MRI-guided prostate radiation therapy planning: investigation of dosimetric accuracy of MRI-based dose planning. Radiother Oncol 98(3):330–334
Chi Y, Wu Q, Yan D (2007) SU-FF-T-163: dose calculation on Cone Beam CT (CBCT). Med Phys 34(6):2438
Jonsson JH et al (2013) Treatment planning of intracranial targets on MRI derived substitute CT data. Radiother Oncol 108(1):118–122
Karotki A et al (2011) Comparison of bulk electron density and voxel-based electron density treatment planning. J Appl Clin Med Phys 12(4):3522
Dowling JA et al (2012) An atlas-based electron density mapping method for magnetic resonance imaging (MRI)-alone treatment planning and adaptive MRI-based prostate radiation therapy. Int J Radiat Oncol Biol Phys 83(1):e5–e11
Yang Y et al (2007) Evaluation of on-board kV cone beam CT (CBCT)-based dose calculation. Phys Med Biol 52(3):685
Hsu S-H et al (2013) Investigation of a method for generating synthetic CT models from MRI scans of the head and neck for radiation therapy. Phys Med Biol 58(23):8419
Korhonen J et al (2014) A dual model HU conversion from MRI intensity values within and outside of bone segment for MRI-based radiotherapy treatment planning of prostate cancer. Med Phys 41(1):011704
Gudur MSR et al (2014) A unifying probabilistic Bayesian approach to derive electron density from MRI for radiation therapy treatment planning. Phys Med Biol 59(21):6595
Rong Y et al (2010) Dose calculation on kv cone beam ct images: an investigation of the hu-density conversion stability and dose accuracy using the site-specific calibration. Med Dosim 35(3):195
Hatton J, McCurdy B, Greer PB (2009) Cone beam computerized tomography: the effect of calibration of the Hounsfield unit number to electron density on dose calculation accuracy for adaptive radiation therapy. Phys Med Biol 54(15):N329
Lim K et al (2009) Pelvic radiotherapy for cancer of the cervix: is what you plan actually what you deliver? Int J Radiat Oncol Biol Phys 74(1):304–312
Burdett N et al (2010) MILXView: a medical imaging, analysis and visualization platform, in E-Health. Springer, New York, pp 177–186
Lambert J et al (2011) MRI-guided prostate radiation therapy planning: investigation of dosimetric accuracy of MRI-based dose planning. Radiother Oncol 98:330–334
Roberson PL et al (2005) Use and uncertainties of mutual information for computed tomography/magnetic resonance (CT/MR) registration post permanent implant of the prostate. Med Phys 32:473
Holloway LC et al (2012) Comp plan: a computer program to generate dose and radiobiological metrics from dose-volume histogram files. Med Dosim 37(3):305–309
Whelan B, Holloway L (2014) SU-ET-194: from Dicom-RT to radiobiological dose metrics in 5 minutes. Med Phys 41(6):267
Gay HA, Niemierko A (2007) A free program for calculating EUD-based NTCP and TCP in external beam radiotherapy. Physica Med 23(3):115–125
Ebert MA (2000) Viability of the EUD and TCP concepts as reliable dose indicators. Phys Med Biol 45:441
Burman C et al (1991) Fitting of normal tissue tolerance data to an analytic function. Int J Radiat Oncol Biol Phys 21(1):123–135
Venselaar J, Welleweerd H, Mijnheer B (2001) Tolerances for the accuracy of photon beam dose calculations of treatment planning systems. Radiother Oncol 60(2):191–201
White GDR WI (1992) Photon, electron, proton and neutron interaction data for body tissues. ICRU report 46
Fogliata A et al (2007) On the dosimetric behaviour of photon dose calculation algorithms in the presence of simple geometric heterogeneities: comparison with Monte Carlo calculations. Phys Med Biol 52(5):1363
Aspradakis MM et al (2003) Experimental verification of convolution/superposition photon dose calculations for radiotherapy treatment planning. Phys Med Biol 48(17):2873
Bortfeld T (2006) IMRT: a review and preview. Phys Med Biol 51(13):R363
Batumalai V et al (2012) How important is dosimetrist experience for intensity modulated radiation therapy? A comparative analysis of a head and neck case. Pract Radiat Oncol 3:e99–e106
Arumugam S et al (2014) Independent calculation-based verification of IMRT plans using a 3D dose-calculation engine. Med Dosim 38(4):376–384
Acknowledgments
The authors would like to acknowledge Dr Mike Milosevic & Dr Anthony Fyles from Prince Margaret Hospital for supplying the patient CT data used in this study. Brendan Whelan would like to acknowledge The Cancer Institute NSW, Liverpool and Macarthur Cancer Therapy Centres, and the Ingham Institute for scholarship support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Whelan, B., Kumar, S., Dowling, J. et al. Utilising pseudo-CT data for dose calculation and plan optimization in adaptive radiotherapy. Australas Phys Eng Sci Med 38, 561–568 (2015). https://doi.org/10.1007/s13246-015-0376-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-015-0376-z