Abstract
Background
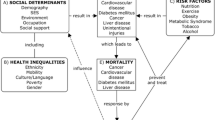
Despite recognition that the health outcomes of Asian American subgroups are heterogeneous, research has mainly focused on the six largest subgroups. There is limited knowledge of smaller subgroups and their health outcomes. This scoping review identifies trends in the health outcomes, reveals those which are under-researched, and provide recommendations on data collection with 24 Asian American subgroups.
Methods
Our literature search of peer-reviewed English language primary source articles published between 1991 and 2018 was conducted across six databases (Embase, PubMed, Web of Sciences, CINAHL, PsychINFO, Academic Search Complete) and Google Scholar, yielding 3844 articles. After duplicate removal, we independently screened 3413 studies to determine whether they met inclusion criteria. Seventy-six studies were identified for inclusion in this review. Data were extracted on study characteristics, content, and findings.
Findings
Seventy-six studies met the inclusion criteria. The most represented subgroups were Chinese (n = 74), Japanese (n = 60), and Filipino (n = 60), while Indonesian (n = 1), Malaysian (n = 1), and Burmese (n = 1) were included in only one or two studies. Several Asian American subgroups listed in the 2010 U.S. Census were not represented in any of the studies. Overall, the most studied health conditions were cancer (n = 29), diabetes (n = 13), maternal and infant health (n = 10), and cardiovascular disease (n = 9). Studies showed that health outcomes varied greatly across subgroups.
Conclusions
More research is required to focus on smaller-sized subgroup populations to obtain accurate results and address health disparities for all groups.
Similar content being viewed by others
Introduction
Asian Americans are the fastest-growing minority population in the United States (U.S.) and include a range of subgroup populations. According to the 2010 U.S. Census, an Asian individual is defined as a person who has origins in the Far East, Southeast Asia, or India [1]. In the U.S., there are more than 23 million Asian Americans, who are from more than 20 countries in East and Southeast Asia as well as the Indian subcontinent [1]. It is projected that the Asian American population will surpass 46 million by 2060 [1].
Research has demonstrated that Asian Americans differ in social characteristics, including language, education attainment, economics, insurance coverage, and health outcomes. For example, although the median annual income for Asian American households was $85,000 in 2019, only two Asian American groups exceeded this figure—Indians ($119,000) and Filipinos ($90,400). In contrast, Burmese ($44,400) and Nepalese ($55,000) had the lowest median household incomes [1]. Asian American subgroups not only differ socioeconomically but in citizenship status, immigration and refugee history, English proficiency, and acculturation, as well as by generation. Furthermore, nativity status, that is, the location of one’s birth, can also influence one’s health status and health outcomes. Research has shown that Asian individuals who are U.S.-born have different mental health, birth, cardiovascular health, and other outcomes than those who are foreign-born [2, 3]. Despite these differences, researchers often aggregate the subgroups under one racial label: “Asian.” It was only in 2000 that the U.S. Census began separating Asians and Pacific Islanders in data reports and in 2003 that the Secretary of Human and Health Services approved this separation and added the following Asian subcategories: Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese, and Other Asian. In addition, prior to 2003, only seven states required reporting of different subgroups—California, Hawaii, New York, New Jersey, Texas, Washington, and Illinois [4]. This brief overview of the history of data collection for Asian American subgroups provides some context for the difficulties in disaggregating Asian American data and highlights the omission of several subgroups in overall research efforts.
A common stereotype associated with Asian Americans is “the model minority,” which argues that Asian Americans are not a disadvantaged or underprivileged minority group. The term “model minority” was coined in the mainstream media of the 1960s and used by white conservatives to oppose the message of the Black Power Movement during the 1960s and 1970s, which claimed that “America was a fundamentally racist society,” and deny the existence of institutional racism [5]. This myth has negatively impacted Asian Americans by dividing them from other racial/ethnic groups and by being indiscriminately applied to all Asian American subgroups despite the differences in culture, history, and socioeconomic status as noted above. Moreover, it has trickled down into beliefs that Asian Americans do not experience health disparities and do not require assistance at an individual, societal, or governmental level [6]. The model minority myth, as well as the failure to disaggregate health data for Asian American subgroups, may mask disparities which result in inaccurate conclusions about such subgroups [7]. For example, in a women’s health study, researchers found that Asian American women had the lowest median high-sensitivity C-reactive protein levels of all categories compared (Asian, non-Hispanic white (NHW), black, and Hispanic women) [117]. However, an international study conducted with Asian subgroups showed that Asian Indians in the UK have higher levels of C-reactive protein than their European counterparts [8].
In 2009, Executive Order 13515 was signed by President Obama to improve the collection of health data among Asian Americans. However, current national and research priorities only focus on the six largest Asian American groups—Chinese, Japanese, Vietnamese, Korean, Filipino, and Indian. Although reviews on Asian American groups exist, they have been carried out exclusively on one group, on the aforementioned larger groups, or on a specific health condition (e.g., colorectal cancer [9], overweight, obesity, type 2 diabetes [10], depression [11], and breast cancer [12]). Although a common conclusion from these reviews is that there is heterogeneity among Asian American subgroups, few studies have attempted to focus on all such subgroups; hence, many disparities remain unknown among the smaller subgroups.
The purpose of this study is to conduct a scoping review to increase understanding of the state of science in disaggregated data on 24 Asian American subgroups. We chose 24 subgroups, as outlined by the 2010 U.S. Census brief on the Asian American population, namely Asian Indian, Bangladeshi, Bhutanese, Burmese, Cambodian, Chinese, Taiwanese, Filipino, Hmong, Indonesian, Iwo Jiman, Japanese, Korean, Lao, Malaysian, Maldivian, Mongolian, Nepalese, Okinawan, Pakistani, Singaporean, Sri Lankan, Thai, and Vietnamese [1]. Our aims were to identify heterogeneity among subgroups, trends in disaggregating Asian American health outcomes, and under-researched subgroups, as well as to provide recommendations about how data could be collected on all 24 subgroups. Understanding health outcomes across Asian American subgroups will allow us to identify gaps and disparities.
Methods
Design
A scoping literature review was performed to synthesize knowledge regarding disaggregated data on the health outcomes of 24 adult Asian American subgroups in the U.S. According to Munn et al. (2018), a scoping review is preferred over a systematic review to identify certain characteristics or concepts in papers or studies and to map, report, or discuss these characteristics or concepts [13]. Arksey and O’Malley (2005) state that a scoping review can be utilized when a research area is complex or has not previously been comprehensively reviewed and can help in identifying research gaps in the existing literature [14]. Since no review has been carried out on the health outcomes of the 24 selected adult Asian American subgroups, a scoping study was chosen.
Search Strategy and Sample
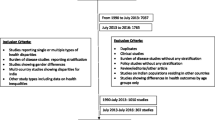
A university librarian was consulted to determine which databases and keywords would identify qualitative, quantitative, and mixed-methods research reports that focus on disaggregated data on the health outcomes of adult Asian American subgroups. As outlined in Fig. 1, Embase, PubMed, Web of Sciences, CINAHL, PsychInfo, Google Scholar, and Academic Search Complete were utilized. The search terms were “disaggregate,” “health,” and “Asian” OR “Asian American.”
Studies were included if they were written in the English language; focused on health outcomes in Asian American subgroups, including at least two subgroups; were U.S.-based; and were primary source articles. Studies were excluded if they did not focus on health outcomes, focused on the pediatric population, or were commentary or method papers.
Analytic Strategy
All studies from the search, including their abstracts and citations, were uploaded into Covidence.org, which is a systematic review management website. Through an iterative process, two members of our study team (SY and ML) individually reviewed and screened each article’s abstract and full text based on the inclusion criteria. Afterward, they came together to consolidate their screenings, and if any discrepancies occurred between their selections, they reviewed the article’s abstract and full text together. A total of 76 studies met the criteria (see Fig. 1). No specific time period was chosen, as the authors were interested in analyzing the temporal trends of studies published. The included studies were published between 1991 and 2018.
Data from studies that met the eligibility criteria were extracted into a Microsoft Excel spreadsheet. Data extraction included information about each study’s purpose; the methods, including subgroups and geographical locations of the study being conducted; and the results. All study results were organized into themes based on the research area of focus.
Results
Study Characteristics
A total of 76 articles met our inclusion criteria. The majority of the studies were conducted in California (n = 34) and nationally (n = 18). The number of studies focusing on Asian American subgroups increased after 2000, with most studies conducted in 2013 (see Fig. 2). The majority of the studies were secondary analysis or retrospective in nature, using either a cross-sectional (n = 21) or longitudinal (n = 51) design. Only four studies were prospective studies. The sample size ranged from 211 to 271,488,278.
The subgroups most represented in the studies were Chinese (n = 76), Japanese (n = 60), and Filipino (n = 60), while the following subgroups were only represented in one study: Burmese, Hmong, Indonesian, Lao/Thai, Malaysian, Mongolian, South Asian/Pakistani, and South East Asian (see Fig. 3). In these 76 studies, the South Asian category was often used as an aggregation of subgroups that could include Asian Indians, Pakistanis, Sri Lankans, Bangladeshis, Bhutanese, Nepalese, and Sikh, while Southeast Asian could include Cambodians, Laos, Burmese, Thai, Malaysians, Vietnamese, Singaporeans, and Indonesians.
Overall, cancer was the most studied health condition (n = 29), followed by diabetes (n = 13), maternal and infant health (n = 10), and cardiovascular disease (n = 9; see Fig. 4). In contrast, viral disease and tuberculosis (TB; n = 5), cerebrovascular disease (n = 3), hip fracture (n = 2), oral health (n = 1), and autoimmune disease (n = 1) were the least represented health conditions among the studies included in this review. In the following section, we report the findings of all the health conditions.
Cancer Results
Twenty-nine studies focused on cancers,Footnote 1 of which 20 focused on a single cancer, while nine considered multiple cancers. Breast cancer was the most included cancer type in the studies (n = 13), while laryngeal (n = 1), and testicular (n = 1) cancers were the least included types. These cancer studies focused mainly on incidence rate (n = 10), survival outcomes (n = 8), mortality rate (n = 6), histologic cell type (n = 5), staging differences (n = 3), treatment outcome (n = 3), and genetic subtypes (n = 1). Of the 29 studies, Chinese was included in all 29. Japanese was included in 28 of the 29 studies. Lao was included in only 3 of the 29 studies.
Six main data sources were used in the 29 cancer studies, namely the Surveillance, Epidemiology, and End Results (SEER) program (n = 12), the California Cancer Registry (CCR) (n = 10), the Death Statistical Master File for California and National Death Index (n = 1), census data (n = 1), national death certificates (n = 1), medical records (n = 1), and a registry (n = 1).
Among cancer studies, research questions related to incidence and mortality rates of cancers were most frequently studied. Overall, cancer incidence and mortality rates varied among Asian American subgroups based on the cancer type and data set used, as well as across time. Breast, colorectal, gastric, liver, and lung cancers were the most studied cancers relating to incidence and mortality, and lung and liver cancers were also the most studied forms of cancer regarding only mortality rates. Oral, nasopharynx (n = 1), larynx (n = 1), esophageal (n = 1), and melanoma (n = 1) cancers were less studied among Asian American subgroups.
In the following section, we summarized the results among the most frequently studied cancers. Tables 1, 2, and 3 contain all combined cancer data across Asian American subgroups [15–25].
Breast Cancer
Breast cancer was the most widely studied cancer. Researchers have examined the incidence (n = 2), mortality (n = 3), incidence and mortality (n = 3), genetics and staging differences (n = 1), and treatment outcomes (n = 1) of breast cancer among Asian American subgroups.
Among the breast cancer incidence studies, Japanese and Filipina women had the highest incidence rates of breast cancer, ranging from 102.5 to 126.5 and 97.4 to 102.4, respectively. However, breast cancer incidence rates among women showed that for Chinese, Japanese, Filipina, Korean, Vietnamese, and Asian Indian/Pakistani groups, breast cancer was the leading form of cancer from 1990 to 2008, with the exception of Kampuchean/Cambodian and Lao populations. For the Kampuchean/Cambodian population, breast cancer had been the third leading cancer site until it became the first in 2008. In contrast, for Laos, breast cancer was in fourth position in 1990 and then in first position in 2008 [21].
In regard to mortality rate, overall, Japanese and Filipina women had higher mortality rates than the other subgroups, ranging from 12.7 to 56.2 and 15.2 to 41.2, respectively. Lauderdale and Huo’s (2008) study, which focused on adults aged 65 and older, reported significantly higher mortality rates for each subgroup [22].
Concerning genetic subtypes and staging differences of breast cancer, the Japanese tended to have better detection and treatment outcomes [26]. Iqbal (2015) reported the odds ratio of Asian American subgroups, compared to NHWs, being stage I breast cancer at diagnosis as 1.24 for Japanese, 0.97 for Chinese, 0.66 for South Asian, and 0.80 for Other Asian [27]. Furthermore, Gelber et al. found that Japanese and Filipina women were less likely to receive breast conserving surgery (BCS) for primary resection and that among women treated with BCS, radiation use seemed lower among Filipina women [28].
Colorectal Cancer
Nine studies focused on colorectal cancer. Researchers examined incidence (n = 1), mortality (n = 3), incidence and mortality (n = 3), and staging and survival outcomes (n = 2). Regarding colorectal cancer incidence, Chinese, Japanese, and Korean men had the highest colorectal cancer incidence rates, ranging from 52.2 to 54, 49.3 to 75.9, and 48.8 to 57.8, respectively [15, 16, 18]. For females, also, Chinese and Japanese subgroups had the highest incidence rates, ranging from 38.9 to 41.5 and 49.3 to 51.9, respectively[15, 16, 18]. When incidence rates were separated by sex and by age (< 50 and > 50 years old) among Chinese, Japanese, Filipino/a, Korean, Asian Indian/Pakistani, and Vietnamese subgroups, the rates were higher overall in males and among those in the 50-and-older category, with the highest incidences found in Japanese and Korean males aged 50 and older [29]. Among males, Koreans and Japanese had the highest incidence rates, while for females, the highest rates were found among Japanese, Chinese, and Koreans [29].
Regarding mortality, for both males and females, Chinese, Japanese, and Koreans had the highest mortality rates for colorectal cancer among the six subgroups represented. These results remained true in Lauderdale and Huo’s study (2008), which sampled only adults aged 65 and older [22].
For staging and survival outcomes of colorectal cancer, Lin et al. (2002) studied survival differences among Chinese, Japanese, and Filipino/a subgroups and NHWs using SEER data from 1988 to 2000 [30]. They found that among males, Filipinos were significantly less likely than other racial or ethnic groups to receive a diagnosis of localized or stage I disease, while for females, the proportions of stage I disease were lower among Chinese and whites. Moreover, among males, Filipino/as had poorer survival after colorectal carcinomas than other groups, while Chinese and white females had poorer five-year survival. Chien et al. (2005) assessed the same database as Lin and observed that, among Asian American subgroups, Japanese had a decreased risk of stage IV cancer but not of stage III; Chinese and Koreans had an increased risk of stage III cancers, but not of stage IV; and Filipino/as had increased risks of both stage III and IV cancers. These findings suggest that Filipino/as, especially males, are at higher risk of being diagnosed with colorectal cancers far later [31].
Gastric Cancer
Eight studies focused on gastric cancer. Researchers examined incidence (n = 1), mortality (n = 3), incidence and mortality (n = 3), and outcome differences (n = 1). The studies on incidence indicated that Korean, Japanese, and Vietnamese populations have the highest gastric cancer incidence rates, ranging from 50 to 54.6, 26.6 to 29.3, and 25.6 to 28.1, respectively, for males and 26.1 to 27.5, 14 to 15.1, and 13.8 to 14.5, respectively, for females [15, 16, 18]. One study demonstrated that Korean Americans had the highest incidence of gastric cancer between 1988 and 2012 in California [32].
The studies that focused on gastric cancer mortality rates examined data from 1997 to 2011 and found that overall, Koreans had the highest mortality rate for gastric cancer among the six subgroups, with the Japanese having the second highest rate [15, 16, 18, 22–24]. This remained true in Lauderdale and Huo’s study (2008), which sampled only adults aged 65 and older [22].
Kim’s study (2009) focused on gastric outcome differences among the Asian American subgroups from 1988 to 2006 [33]. Filipino/as had the worst overall survival, while Koreans had the best. Specifically, the median survival times for Korean, Japanese, Chinese, Vietnamese, and Filipino/a subgroups were 22.4 months, 13.7 months, 16.8 months, 16.3 months, and 10.3 months, respectively. When compared, Koreans generally had favorable features, with high rates of localized disease and low rates of lymph node metastasis, while Filipino/as had higher rates of distant metastatic disease [33].
Liver Cancer
Among the studies on liver cancer, researchers examined incidence rates (n = 2), mortality rates (n = 3), incidence and mortality rates (n = 3), and survival outcomes (n = 2). Although liver incidence rates appeared to be high across Asian American subgroups, Vietnamese, Cambodian, and Lao subgroups had the highest, ranging from 47.3 to 55.5, 42.8 to 29.1, and 45.6 to 79.4, respectively, for males and 14.4 to 16.8, 11.7 to 14.1, and 12.3 to 23.1, respectively, for females [15, 16, 18, 19]. Gomez’s study (2013) demonstrated that liver cancer remained one of the top five cancers for Chinese males, Filipino males, Korean males, Vietnamese males, Cambodian males and females, and Lao males and females from 1990 to 2008 [21]. Likewise, Pham’s study (2018) reported that Southeast Asian American subgroups (Vietnamese, Lao, and Cambodian) had an eight to nine times higher risk of developing hepatocellular carcinoma than other Asian ethnic groups and NHWs [19].
Based on the findings of the studies that focused on liver cancer mortality rates from 1988 to 2011, overall, Vietnamese had the highest mortality rate among the six subgroups for males, while mortality rates for females were lower than those of males[15, 16, 18, 22–24]. Moreover, Japanese, Filipino/a, and Asian Indian subgroups had lower mortality rates than the other ethnic groups [15, 16, 18, 22–24] (see Table 3).
With respect to the two studies that focused on outcome differences, first, Kwong’s study (2010) compared median survival outcomes among nine subgroups [34]. The median survival outcomes for Chinese, Vietnamese, Filipino/a, Korean, Japanese, Lao/Hmong, Cambodian, South Asian, and Thai subgroups were 10 months, 12 months, 7 months, 11 months, 12 months, 2 months, 6 months, 12 months, and 4 months, respectively [34]. Second, in Stewart’s study (2016), Lao/Hmong and Cambodians experienced significantly higher mortality rates, were less likely to receive curative treatment, and had the lowest cause-specific medial survival in weeks than the Chinese, Filipino/a, Japanese, Korean, South Asian, Thai, Vietnamese, Other Asians, and NHW [35].
Lung Cancer
Among the studies on lung cancer, researchers examined incidence rates (n = 1), mortality (n = 3), incidence and mortality (n = 3), differences in histologic cell type (n = 3), and survival outcomes (n = 1). In general, lung cancer incidences were higher among males for all subgroups than for females. Filipino, Vietnamese, Cambodian, and Lao males had the highest incidence rates, ranging from 70.0 to 72.5 and 72.3 to 72.9 for the Filipino and Vietnamese groups, respectively, and Cambodian and Lao males had rates of 82.6 and 87.3, respectively [15, 16, 18]. Gomez (2013) found that lung cancer remained one of the top five cancers for all eight subgroups from 1990 to 2008 [21].
In the studies that focused on mortality rates from 1988 to 2011, such rates were higher among males than females. Vietnamese, Korean, and Chinese males had the highest mortality rates, ranging from 26.2 to 35.5, 18.2 to 26.6, and 14.5 to 20.7, respectively [15, 16, 18, 22–24]. This remained true in Lauderdale’s study (2008) [22].
Furthermore, the studies that focused on differences in histologic cell type for lung cancer found different rates among Asian American subgroups. For example, Cheng et al.’s study (2014) assessed trends in histologic cell types across AANHPI populations (Chinese, Filipino, Japanese, Korean, Vietnamese, Lao, Kampuchean, and Asian Indian/Pakistani subgroups) [36]. These researchers found significant increases in adenocarcinoma in Filipina and Korean women and increases in squamous cell carcinoma among Japanese women. However, trends in rates for the other histologic cell types were declining or remained stable in most subgroups. In addition, Epplein’s study (2005) assessed lung cancer incidence among Chinese, Filipino/a, and Japanese subgroups, adjusting for smoking [37]. They reported that among Chinese women, the risks for adenocarcinoma and large cell undifferentiated carcinoma were six- and fourfold, respectively, while Filipina women had an appreciably higher lung cancer risk for adenocarcinoma. Moreover, Raz’s study (2008) assessed epidemiologic data on the prevalence of non-small cell lung cancer (NSCLC) among Chinese, Filipino/a, Japanese, Korean, Vietnamese, and South Asian subgroups and reported that South Asians had the lowest incidence rates, while Vietnamese had the highest. Japanese and Koreans had intermediate rates of NSCLC. The author also found that Asian American men tended to have higher incidence rates than women and that foreign-born Asian Americans tended to have higher incidence rates, with the exception of South Asians [38].
Trinh’s study (2015) focused on survival outcomes for lung cancer, examining lung-cancer-specific survival among Chinese, Filipino/a, Japanese, Korean, Asian Indian/Pakistani, Vietnamese, and Other Asian populations [39]. Trinh et al. (2015) observed no racial differences among lung cancer patients with stage 1 or 2 disease in receiving treatment; however, among patients with stage 3 disease who did not receive treatment, the Chinese, Filipino/as, and Other Asians had the lowest rates of receiving treatment among subgroups.
Other Cancers
Other cancers included lymphoid (n = 5), leukemia (n = 4), myeloma (n = 3), thyroid (n = 3), lip/oral/nasopharyngeal/laryngeal (n = 3), esophageal (n = 3), pancreatic (n = 4), melanoma (n = 3), kidney and renal pelvis/urinary bladder (n = 3), brain and central neverous system (CNS; n = 3), gallbladder (n = 3), ovarian (n = 6), cervical (n = 7), uterine (n = 4), prostate (n = 10), and testicular cancers (n = 1). Among the lymphoma studies, Miller’s study (2008) reported that the overall incidence rate for Non-Hodgkin’s lymphoma (NHL) was higher among males than females for each subgroup except for Cambodian and Lao women, as data for NHL were not available for these populations [18]. Of the seven subgroups, Japanese, Filipino, Cambodian, and Lao males had the highest incidence rates: 18.3, 19.4, 22.1, and 20.3, respectively [18, 22–24]. Similarly, Gomez’s study (2013) reported that NHL remained one of the top five cancers for only Filipino and Asian Indian/Pakistani males from 1990 to 2008 [21].
The leukemia and myeloma studies showed mixed results across the Asian American subgroups. For instance, Carreon’s study (2008) found that rates were generally higher among men of all subgroups except the Vietnamese; however, the data varied by lymphoid subtype [40]. Moreover, Miller’s study (2008) found that leukemia incidence rates were higher among males than females for each subgroup. Furthermore, Asian Indian/Pakistani males had the highest leukemia incidence rate, at 12.2, and Korean females had the lowest leukemia incidence rate, at 4.6 [18]. In addition, Gomez’s study (2013) demonstrated that leukemia was never among the top five cancers for all eight subgroups from 1990 to 2008 [21]. While leukemia mortality rates were lower among females than males across all six subgroups, older Filipino males (aged 65 and older) had the highest leukemia mortality rates, followed by Chinese and Korean: 32, 28.4, and 22.5, respectively [18, 22–24].
Similarly, myeloma incidence and mortality rates were overall low among the six subgroups [18], and myeloma was never among the top five cancers for all eight subgroups from 1990 to 2008 [21]. However, Miller (2008) reported that Filipino males had the highest myeloma incidence rate, at 5.8, and Korean females had the lowest incidence rate, at 2.0 [18]. See Tables 1, 2, and 3 for additional incidences and trends of other cancers.
Among the cervical cancer studies, Bates’ study (2008) examined cervical cancer subtype variations among Chinese, Filipina, Korean, Japanese, South Asian, and Vietnamese women. The authors found that Chinese, Korean, South Asian, and Vietnamese women had a greater proportion of squamous cell carcinoma subtype and a lower proportion of adenocarcinoma subtype, while the opposite was observed for Japanese and Filipina women [41]. Another study also assessed cervical cancer subtype variations with some results differing from those presented by Bates. Wang et al. (2008) also found that Vietnamese and Korean women had the greatest rates for squamous cell carcinoma subtype; however, for adenocarcinoma, they found that Vietnamese and Filipina women had the highest rates [42].
Of the prostate cancer studies, four assessed variations in survival outcomes among Asian American subgroups. Chao’s study (2016) examined Chinese, Japanese, Filipino/a, Korean, Vietnamese, Asian Indian/Pakistani, and other Asian subgroups and found that all subgroups had a higher chance of being diagnosed with metastatic disease than NHWs [43]. They also found that survival outcomes among Filipino/as and Asian Indian/Pakistani were higher than those of the other subgroups [43]. In addition, Lin’s study (2002) demonstrated that Filipinos were less likely to contract a localized or stage I disease [30]. Robbins’ study (2007) also assessed 10-year risk of death and found that all subgroups (Chinese, Filipino, Japanese, Korean, and Vietnamese), with the exception of South Asian men, had lower 10-year risks of death from prostate cancer [44].
Diabetes
Thirteen articles focused on or included diabetes prevalence and complications due to diabetes mellitus (DM) among the following subgroups: Chinese, Filipino/a, Japanese, Korean, Vietnamese, Asian Indian, South Asian (Asian Indian, Pakistani, Bangladeshi, Sri Lankan, or Nepalese), Southeast Asian (Cambodian, Lao, Burmese, Thai, Malaysian, or Indonesian), and Other Asian. Tables 4 and 5 show combined data on diabetes prevalence and incidence rates among the subgroups. Eight studies included prevalence rates, and, overall, Filipino/as, Asian Indians, South Asians—including Asian Indians, among others—had higher prevalence rates [45–53]. One study included incidence rates, and, similarly, Filipino/a and South Asian subgroups had higher rates [48]. Furthermore, studies that separated data by sex demonstrated that among men, rates and DM likelihood were higher among Filipino and South Asian populations, while among women, higher rates were found among Filipina and Korean women [45, 54]. Three studies included data on complications due to DM, namely renal disease, myocardial infarction, heart failure, stroke, and lower extremity amputation [55, 56].
Rheumatic Disease
One study included prevalence data for arthritis for the following subgroups: Chinese, Cambodian, Vietnamese, and U.S. Asians [51]. Data was collected from local health surveys conducted among Chinese, Cambodian, and Vietnamese communities in Chicago and the American Community Survey from 2005 to 2007. The study did not differentiate between types of arthritis. The study’s results indicated that Cambodian and Vietnamese adults were diagnosed with arthritis twice as often as Chinese and U.S. Asian adults.
Autoimmune Disorders
One study included data regarding systemic lupus erythematosus (SLE) among Chinese, Japanese, and Filipino/a subgroups [57]. Data were collected from five medical centers, five rheumatologists, eight nephrologists, 190 primary care physicians in regard to patients diagnosed with SLE from 1988 to 1989, and the Hawaii Lupus Foundation. The researchers found a statistically significant difference in increased SLE prevalence odds ratios for Chinese and Filipino/a individuals compared to Caucasians.
Infectious Diseases
Hepatitis B and C
Four studies included prevalence data for hepatitis B and/or C (see Table 4). From the prevalence rates, Chinese, Vietnamese, and Cambodian subgroups had higher rates of hepatitis B than the other subgroups [58, 59]. Misra’s study (2013) also noted that first-generation Chinese and Southeast Asian immigrants (from Burma, Cambodia, Indonesia, Laos, Malaysia, the Philippines, Myanmar, Singapore, Thailand, and Vietnam) had higher rates of hepatitis B and C than other Asian subgroups [60]. Likewise, Noah’s study (2018) examined births among Asian American women with hepatitis B infection and found that Chinese American mothers were 10 times more likely to experience this infection than Asian Indian and Japanese American mothers [61].
Juon’s study (2019) also included prevalence rates for hepatitis C. In comparison to other subgroups, hepatitis C infection was higher among Cambodians (10.8%), who also had the highest prevalence rate for hepatitis B in the study [59].
Tuberculosis
Two studies included data on TB, specifically examining the trends in TB case rates among Asian American subgroups from 2002 to 2007. There was a decline in rates among Vietnamese, Filipino/a, Asian Indian, Pakistani, and Korean subgroups, of 17.7%, 12.7%. 17.6, 4.3%, and 20.1%, respectively, while the rates increased among the Cambodian and Chinese subgroups by 20.2% and 4.2%, respectively [62]. Moreover, foreign-born individuals had higher rates than U.S.-born residents. Shah’s study (2010) stated prevalence rates for the Chinese, Cambodian, and Vietnamese communities in Chicago of 6.2, 40.6, and 4.5, respectively [51].
Cardiovascular Diseases
Nine studies involved data on cardiovascular disease, including hypertension, dyslipidemia, and cardiovascular disease mortality rates, odds ratios, and prevalence rates. The majority of the studies included subgroups of the six largest Asian American subgroups. A trend observed across studies was that Asian Indian men and women had higher proportional mortality ratios for coronary heart disease (CHD) among Asian American subgroups [63–65]. One study demonstrated that the odd ratios for CHD were significantly higher among Filipino/a men and women as well as among Asian Indian men [66]. Frank’s study (2014) on dyslipidemia patterns noted that Asian Indian, Filipina, and Vietnamese women and Asian Indian men had the highest risk of having all three dyslipidemia patterns (high triglycerides (TG), low high-density lipoproteins (HDL), high low-density lipoproteins (LDL)) [67]. For data on hypertension, see Table 4 [51, 66, 68–70].
Cerebrovascular Disease
Three studies—all limited to subgroups from the six largest Asian American subgroups—focused on cerebrovascular disease, including overall cerebrovascular disease mortality rates, odds ratios, and prevalence rates. Holland’s study (2011) noted that Filipina women had greater odds of overall stroke and ischemic stroke, while the odds of hemorrhagic stroke were greater for Korean women and Vietnamese men [66]. Furthermore, two studies included proportional mortality ratios (PMRs). First, Wild’s study (1994) examined PMRs among Chinese, Japanese, and Asian Indian subgroups and found PMRs to be higher in the Chinese and Japanese groups than among NHWs and Asian Indians [65]. Second, Jose’s study (2014) examined Chinese, Japanese, Asian Indian, Vietnamese, Korean, and Filipino/a subgroups and noted that PMRs were higher in every Asian American subgroup than among NHWs, particularly the Filipino/a and Vietnamese subgroups [63].
Mental Health
Four articles explored mental health conditions, with two studies assessing substance use disorders and two assessing depression. Park’s study (2010) focused on Chinese and Korean Americans who were receiving alcohol use disorder treatment and noted differences in drinking patterns between the two subgroups [71]. Specifically, Korean Americans consumed significantly more alcohol than Chinese Americans. However, 75% of Chinese and Korean Americans were mandated to receive alcohol treatment by the criminal justice system [71].
Bersamira’s study (2017), in comparison, examined past-year substance use—including marijuana, cocaine, and prescription drugs, among other substances—among Filipino/a, Chinese, Vietnamese, and other Asians. The authors noted heterogeneity among the prevalence rates for each subgroup [72]. Filipino/as had the highest (8.1%) and Vietnamese the lowest (1.5%) prevalence of past-year drug use among all Asian subgroups [72].
The remaining two studies focused on the prevalence of depressive disorders among middle-aged Chinese and Japanese women and on disease onset and prevalence among foreign-born Chinese, Filipino/a, and Vietnamese Americans [73, 74]. Lee and colleagues reported that 6.8% of Vietnamese, Filipino/a, and Chinese aged 18 and older have a major depressive disorder [71]. Among middle-aged women, Chinese and Japanese have a lower crude prevalence of depressive symptoms than either African American or Hispanic women [70].
Mortality
Three articles examined the overall mortality rates among the six largest subgroups: Chinese, Vietnamese, Filipino/a, Japanese, Asian Indian, and Korean. Overall, cardiovascular disease and cancer were the two leading causes of death for both males and females in each subgroup, while the third leading cause for males across all subgroups in 1992 was either cerebrovascular disease or accidents [75]. In comparison, Hastings (2015) examined mortality rates using U.S. mortality records from 2003 to 2011 and reported that for females, cancer was the leading cause of death for all subgroups with the exception of Asian Indians, for whom heart disease was the leading cause [76]. Among females in each subgroup, the top three causes of death were cancer, cardiovascular disease, and cerebrovascular disease, but beyond the top three, the causes varied by subgroup. For males, cancer was the leading cause of death in Chinese, Korean, and Vietnamese populations, whereas heart disease was the leading cause for Filipino, Japanese, and Asian Indian males, and beyond the top three, causes and rates varied similarly among females [76]. Lauderdale (2002) examined mortality rates among elderly Asian Americans enrolled in Medicare Part B from 1990 to 1999 and noted that (a) mortality rates were similar among the subgroups, with the exception of Vietnamese men, who had a somewhat lower probability of death than the other Asian male subgroups; and (b) mortality for Indian women was higher than for other Asian subgroups [77].
Oral Health
One article focused on oral health, assessing trends of edentulism—complete tooth loss—among older Asian Americans from the Chinese, Filipino/a, Asian Indian, and Other Asian subgroups using NHIS data from 1999 to 2008 [78]. Wu’s study (2013) noted that Filipino/as had higher odds of edentulism than the other subgroups; however, overall, rates of decline were similar across the subgroups [78].
Hip Fracture
Two articles focused on hip fractures among Asian American subgroups: Lauderdale’s study (1997) examined hip fracture incidences among Chinese, Japanese, and Korean subgroups, while Patel’s study (2016) examined mortality rates following hip fractures among Chinese, Japanese, and Filipina women [79, 80]. Both studies noted that hip fracture incidence and mortality rates were lower in the Asian American subgroups than among NHW.
Longevity
One study by Park et al. (2009) examined longevity disparities among ethnic groups in Hawaii, including Chinese, Filipino/a, Japanese, and Korean subgroups [81]. Park et al. noted that the East Asian subgroups (Chinese, Japanese, and Korean) demonstrated the greatest longevity of all the Asian subgroups.
Maternal and Infant Health
Ten articles focused on or included maternal and infant health. See Tables 6 and 7 for prevalence and incidence rates, respectively, for the following maternal and infant health outcomes.
Gestational Diabetes Mellitus
Six articles included gestational diabetes mellitus (GDM), with four studies focusing on prevalence rates and two studies on incidence rates among Asian Indian, Japanese, Chinese, Filipina, Korean, Vietnamese, and Other Asian populations. For prevalence rates of GDM, Asian Indians (n = 3 studies) had the highest prevalence rates of all Asian subgroups for GMD, followed by Filipina (n = 2) and Vietnamese (n = 3) (see Tables 6 and 7 for actual rates).
Pregnancy-Associated Hypertension, Preeclampsia, and Eclampsia
Five articles included pregnancy-associated hypertension, preeclampsia, and/or eclampsia [82, 83]. Two included incidence rates for preeclampsia for the Indian/Pakistani, Japanese, Chinese, Filipina, Korean, and Vietnamese subgroups, and one study included prevalence rates for Cambodian, Lao, Vietnamese, and Japanese females [84–86]. The five studies indicated that Filipina women had the highest incidences of PAH (2.86; 6.3), preeclampsia (6.8; 1.5), and eclampsia (0.19) of all the Asian subgroups considered (See Table 7 for incidence comparison).
Preterm Delivery, C-Section, and Cephalopelvic Disproportion
Four articles included incidence rates on either or both preterm deliveries less than 37 weeks and preterm deliveries less than 32 weeks among Chinese, Japanese, Filipina, Asian Indian, Indian/Pakistani, Korean, Vietnamese, Hmong, Cambodian, and Lao/Thai subgroups [82, 83, 85, 86]. Among the four studies, the results differed with regard to which subgroups had higher rates, as each study included different subgroups and largely considered different time periods. For example, Wong et al. (2008). Reported that Filipinas had higher incidence rates (12.62), while Rao et al. (2006) reported that Vietnamese had a higher incidence rate (12.4) of preterm delivery less than 32 weeks [83, 85]. However, one generally consistent finding across the studies was that the rates of preterm deliveries were lower in East Asian American subgroups (Chinese, Japanese, and Korean) than in other subgroups [82, 83, 85, 86]. See Table 7 for incidence rates.
Two articles included cesarean section incidence rates and mentioned the following subgroups: Asian Indian, Indian/Pakistani, Japanese, Chinese, Filipina, Korean, and Vietnamese [82, 83]. Rao (2006) did not note significant differences among the subgroups regarding cesarean delivery. However, Wong (2008) noted a higher incidence among Asian Indians (23.7) than among the other Asian American subgroups—Chinese [17.24], Filipina [19.13], Japanese [16.25], Vietnamese [17.58], and Korean [18.22] (see Table 7 for more details of incidence rates). Furthermore, one study included cephalopelvic disproportion (CPD) among the following subgroups: Chinese, Japanese, Filipina, Asian Indian, Korean, and Vietnamese [83]. Overall, the incidence of CPD was low among Asian American subgroups, with incidences ranging from 1.76 to 3.01.
Birth Weight and Infant Mortality
Three studies included birth weight, specifically assessing incidence rates for birthweight less than 2500 g and birthweight greater than 4000 g among the following subgroups: Cambodian, Chinese, Filipino/a, Asian Indian, Indian/Pakistani, Japanese, Korean, Lao, Thai, and Vietnamese [82, 83, 87]. See Table 7 for incidence rates.
A study by Wang et al. (1992) examined infant mortality rates among Japanese, Chinese, and NHW Americans. Wanget al. (1992) noted that although Japanese and Chinese Americans had somewhat lower rates of infant mortality than NHW Americans, they had a higher risk of sudden infant death syndrome than NHW Americans, particularly Chinese females (OR = 2.84) [88].
Discussion
This scoping review provides a better understanding of health outcomes for 24 Asian American subgroups. Specifically, we found clear differences in the prevalence, incidence, and mortality of health outcomes across the subgroups, highlighting the heterogeneity of Asian Americans. Cancer was the most studied health condition, followed by diabetes, among Asian American subgroups. It is not surprising that cancer and diabetes are the most studied health conditions, as these areas have received the most funding through the National Cancer Institute and National Institute of Diabetes and Digestive and Kidney Diseases. Although multiple studies have documented differences in subgroups, most have compared two subgroups or were disease-focused [89–91]. Our study is the first to examine the incidences and prevalence of different health outcomes across 24 Asian American subgroups.
Although mental health and substance abuse are highly prevalent conditions in the U.S., we were surprised that such health conditions were not heavily focused on in the literature among Asian American subgroups, given they were addressed by only four studies. Mental health impacted 51.5 million people in the U.S. in 2019 [92]. Additionally, approximately 10 million people aged 12 and older misused opioids in 2019, including misuse of prescription pain relievers [93]. Such high prevalence warrants more research on substance abuse, including opioids, among subgroups of Asian American populations.
We also found that the existing studies on Asian American subgroups mainly focused on the six largest Asian American subgroups, and many subgroups remained underrepresented or omitted in research (see Fig. 3). Although listed in the 2010 U.S. Census, the following subgroups were omitted from any of the studies examined in this review as a single non-aggregated subgroup: Bangladeshi, Bhutanese, Taiwanese, Iwo Jiman, Maldivian, Nepalese, Okinawan, Singaporean, and Sri Lankan. In addition, many of the studies aggregated subgroups under larger labels, such as South Asian, Southeast Asian, or Other Asian [17, 19, 27, 29, 31, 34, 35, 38, 39, 41, 43–45, 48–50, 52, 54, 55, 58, 61, 72, 75, 78, 94, 95].
However, we observed a small increase in the inclusion of other, smaller, Asian American subgroups after 2009 (see Fig. 2). Half of the six most commonly represented Asian American subgroups are of East Asian origin (i.e., Chinese, Japanese, and Korean), which do not fully represent the heterogeneity of the Asian continent. It is possible that Executive Order 13515 signed by President Obama to improve the collection of health data among Asian Americans may have had some impact on this trend. Despite the recognition of the importance of including subgroups in research, a recent study has reported that Asians are underrepresented in high-impact medical research studies [96] and research funding [97]. Interestingly, the National Institute of Health (NIH) did not consider Asians to be an underrepresented minority (URM) in their recent analysis of R01 grant outcomes of T32 postdoctoral participants nor as a group that is underrepresented in biomedical research [98]. The NIH website lists the following groups as underrepresented: “Blacks or African Americans, Hispanics or Latinos, American Indians or Alaska Natives, Native Hawaiians, and other Pacific Islanders” [99]. This omission of Asian Americans is reflected in their research funding, as it has been reported that funding for Asian American populations at the NIH amounted to only 0.17% from 1992 to 2018 [100]. In addition, while there has been an increase in Asian American participation in NIH clinical trials, namely from 2.5% in 2011 to 12.1% in 2016, this increase has not translated into increased data disaggregation [97]. A plausible reason for the frequent omission of Asian American populations from the discussion regarding disparities and the fact they are not considered as a URM group may be the erroneous model minority myth. The myth of Asian Americans successfully adapting to the U.S. and being financially better off and physically healthier than other minorities may have resulted from limited and sample-biased studies. This myth has been and continues to be perpetuated in academia, which often categorizes Asian Americans as a monolith, consequently ignoring and masking any within-group socioeconomic and health disparities that exist [101, 102].
Representation and inclusion of all racial and ethnic minority populations is critical in providing equitable care. Aggregation and masking within-group differences is not unique to Asian Americans; rather, it an issue affecting several other races and ethnicities, including, but not limited to, Native Americans, Black and African Americans, and Hispanic and Latinx Americans [103]. Native Americans have over 500 recognized nations in the U.S. Meanwhile, Black and African Americans include individuals and families born and raised in the U.S. as well as immigrants from different countries in Africa and the Caribbean. Moreover, Hispanic and Latinx Americans include individuals and families who originate from several different countries, including, but not limited to, Mexico, Puerto Rico, Cuba, Peru, Honduras, and the Dominican Republic. Reflecting the heterogeneity of Asian American subgroups, these subgroups also have distinct languages, cultures, immigration histories, and generation statuses of their own that have varying impacts on health outcomes [103]. Arroyo-Johnson et al. (2016) and Griffith et al. (2011) examined heterogeneity among Hispanic and Black American subgroups, respectively [104, 105]. Arroyo-Johnson’s study (2016) was the first to disaggregate diabetes prevalence trends over time among Hispanic subgroups, which included Mexican/Mexican American, Puerto Rican, and Cuban/Cuban American [104]. Arroyo-Johnson et al. noted that over the 15-year period studied, diabetes prevalence differed significantly by race/ethnicity and education. The 5-year trend in diabetes prevalence among participants with less than a high school education was highest among Cubans/Cuban Americans, Puerto Ricans, non-Hispanic blacks, and NHWs, while among participants with more than a high school education, non-Hispanic blacks had the highest prevalence [104]. These differences would have been masked by utilizing an aggregated Hispanic label. Hence, the need to study subgroup differences is greater than ever, as subgroup populations have diverse social determinants of health, including, but not limited to, immigration histories, immigration status, differing cultures, languages, English proficiency, economic status, educational status, and access to health care.
All of the studies reviewed only considered English-speaking individuals. However, the Asian American subgroups have diverse languages and cultural backgrounds. Over 40% of languages are spoken by Asian Americans in the U.S. [106], and over 67 million people speak a foreign language at home [107]. It is thus critical that non-English speakers, including Asian American subgroups, are included in research. Research has demonstrated that having limited English proficiency (LEP) is associated with poor access to healthcare, poor health outcomes, and higher levels of dissatisfaction with care [118, 119, 120]. The disparity gap in care may be larger for Asian American subgroups with LEP than among English-speaking Asian Americans subgroups. Therefore, it is critical that researchers do not see language as a barrier to participating in research. Researchers must urgently devise innovative solutions to target or reach all populations by starting with language-appropriate surveys.
This review has some limitations. First, we only included 24 Asian American subgroups; hence, interpretations of our findings should be made with caution. Second, our search terms were rather broad (i.e., “Disaggregate,” “Health,” and “Asian” OR “Asian American”); thus, we were unable to cover specific topics such as eye care, counseling, rehabilitation services, and more. Additionally, we did not search the gray literature. It is thus possible that we may have missed some studies. Future research could conduct a review on specific health topics to gain a deeper understanding of their impact on Asian American subgroups’ health. Third, we did not review studies focusing on social determinants of health among Asian American subgroups. Future reviews could examine such areas of focus.
Research and Policy Recommendations
The majority of the studies reviewed were from existing databases, such as cancer registries, national surveys, Medicare, and/or electronic health records. Additionally, the majority of the studies were secondary or retrospective longitudinal analyses. These factors contribute to the existing challenge of data disaggregation, including small sample sizes, oversampling of certain Asian Americans, and/or uneven distribution of geographic representation [108, 109]. A limited number of studies were prospective works targeting smaller-sized Asian American subgroups in general. Therefore, we want to echo and emphasize many other scholars’ recommendations to oversample Asian Americans, particularly the smaller-sized groups, eliminating the umbrella “Asian American” label, and allowing for the reporting of race and ethnicity to include Asian American subgroup categories, as well as many others [5, 110]. While it may appear challenging to oversample or include smaller-sized Asian American subgroups, and the use of traditional methods of recruitment and data collection may not be appropriate, community-based participatory research (CBPR) may offer a solution whereby individuals from each community can actively be involved and drive the research. There is strong evidence that CBPR is an effective and appropriate solution to working with minority or vulnerable populations [111, 112].
The lack of funding and recognition of Asians as a URM at the federal level is ultimately the underlying barrier to further investigating health disparities among Asian American subgroups. Additionally, most research on Asian American subgroups has historically been performed with East Asians. Therefore, we recommend that funders such as NIH include Asian American subgroups as URM and that researchers aim to recruit or include all 24 subgroups. Recruiting or including all 24 subgroups in research requires innovative solutions. First and foremost, there is a need for science to be applied in research recruitment and for racial and ethnic minority populations, including Asian American subgroups, to be engaged.
Conclusions
This scoping review has examined trends in disaggregating 24 Asian American subgroups’ health outcomes and identified under-researched subgroups. The study findings confirm that health outcomes vary greatly across subgroups, suggesting that certain subgroups are at higher risk than others. However, the reporting on health outcomes of small-sized subgroups was limited due to the underrepresentation of those populations in disaggregated research. This review also clearly shows that there are many Asian American subgroups that are not merely underrepresented but not represented at all in biomedical research and national health priorities. This finding calls for a dismantling and restructuring of how national policies, funding priorities, and academia perceive Asian American populations without the “model minority” lens. It also calls for a better understanding and education on the various historical, cultural, and immigration differences between these subgroups. With the current social and political climate (e.g., COVID and Asian hate crimes), different Asian American subgroups are disproportionately affected. However, data on Asian American subgroups continues to be aggregated as if describing a monolithic group at the national level (for example by the Centers for Disease Control and Prevention) [113]. As an aggregate, Asian American deaths from COVID-19 appear to be lower than their population share. However, aggregating such data obscures any disparities that exist among subgroups as well as any variation that can be seen by location, as Asian Americans are not uniformly spread across the nation [114]. In addition, Asian American deaths may be unknown in some states, such as Florida and South Carolina, which continue to classify Asian American as “Other” or aggregate them with other larger racial groups ([115, 116]. National efforts, including funders, are needed to address data aggregation among subgroup populations.
Availability of data and material
Not applicable.
Code Availability
Not applicable.
Notes
The numbers reported in this result section are numbers from the initial cancer studies.
References
Hoeffel EM, Rastogi S, Kim MO, Shahd H. The Asian Population: 2010. 2010 Census Briefs. 2012;24.
Budiman A, Ruiz NG. Asian Americans are the fastest-growing racial or ethnic group in the U.S. [Internet]. Pew Res. Cent. 2021 [cited 2021 Jun 17]. Available from: https://www.pewresearch.org/fact-tank/2021/04/09/asian-americans-are-the-fastest-growing-racial-or-ethnic-group-in-the-u-s/
Sun F, Lee J, Liu S, Wardian J, Guo M. Major depressive disorder and dysthymia disparities between U.S.-born and foreign-born Chinese Americans. Asian Am J Psychol. 2020;11:138–46.
Lee JR, Maruthur NM, Yeh H-C. Nativity and prevalence of cardiometabolic diseases among U.S. Asian immigrants. J Diabetes Complications. 2020;34:107679.
Holland AT, Palaniappan LP. Problems with the collection and interpretation of Asian-American health data: omission, aggregation, and extrapolation. Ann Epidemiol. 2012;22:397–405.
Kawai Y. Stereotyping Asian Americans: the dialectic of the model minority and the Yellow Peril. Howard J Commun. 2005;16:109–30.
Yi SS, Kwon SC, Sacks R, Trinh-Shevrin C. Commentary: persistence and health-related consequences of the model minority stereotype for Asian Americans. Ethn Dis. 2016;26:133–8.
Forouhi NG, Sattar N, McKeigue PM. Relation of C-reactive protein to body fat distribution and features of the metabolic syndrome in Europeans and South Asians. Int J Obes Relat Metab Disord J Int Assoc Study Obes. 2001;25:1327–31.
Gu M, Thapa S. Colorectal cancer in the United States and a review of its heterogeneity among Asian American subgroups. Asia Pac J Clin Oncol. 2020;16:193–200.
Lu W, Diep CS, McKyer LJ. Risk factors for childhood obesity among Asian Americans: a systematic review of literature and recommendations for health care research. J Health Care Poor Underserved. 2015;26:171–90.
Kim HJ, Park E, Storr CL, Tran K, Juon H-S. Depression among Asian-American adults in the community: systematic review and meta-analysis. PloS One. 2015;10:e0127760.
Wen K-Y, Fang CY, Ma GX. Breast cancer experience and survivorship among Asian Americans: a systematic review. J Cancer Surviv Res Pract. 2014;8:94–107.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:143.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
Kwong SL, Chen MS, Snipes KP, Bal DG, Wright WE. Asian subgroups and cancer incidence and mortality rates in California. Cancer. 2005;104:2975–81.
McCracken M, Olsen M, Chen MS, Jemal A, Thun M, Cokkinides V, et al. Cancer incidence, mortality, and associated risk factors among Asian Americans of Chinese, Filipino, Vietnamese, Korean, and Japanese Ethnicities. CA Cancer J Clin. 2007;57:190–205.
Gomez SL, Quach T, Horn-Ross PL, Pham JT, Cockburn M, Chang ET, et al. Hidden breast cancer disparities in Asian women: disaggregating incidence rates by ethnicity and migrant status. Am J Public Health. 2010;100(Suppl 1):S125-131.
Miller BA, Chu KC, Hankey BF, Ries LAG. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U.S. Cancer Causes Control CCC. 2008;19:227–56.
Pham C, Fong T-L, Zhang J, Liu L. Striking racial/ethnic disparities in liver cancer incidence rates and temporal trends in California, 1988–2012. JNCI J Natl Cancer Inst. 2018;110:1259–69.
Wang SS, Carreon JD, Gomez SL, Devesa SS. Cervical cancer incidence among 6 asian ethnic groups in the United States, 1996 through 2004. Cancer. 2010;116:949–56.
Gomez SL, Noone A-M, Lichtensztajn DY, Scoppa S, Gibson JT, Liu L, et al. Cancer incidence trends among Asian American populations in the United States, 1990–2008. J Natl Cancer Inst. 2013;105:1096–110.
Lauderdale DS, Huo D. Cancer death rates for older Asian-Americans: classification by race versus ethnicity. Cancer Causes Control CCC. 2008;19:135–46.
Thompson CA, Gomez SL, Hastings KG, Kapphahn K, Yu P, Shariff-Marco S, et al. The burden of cancer in Asian Americans: a Report of national mortality trends by Asian ethnicity. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol. 2016;25:1371–82.
Chu KC, Chu KT. 1999–2001 Cancer mortality rates for Asian and Pacific Islander ethnic groups with comparisons to their 1988–1992 rates. Cancer. 2005;104:2989–98.
Herrinton LJ, Schwartz SM, Weiss NS. Ovarian cancer incidence among Asian migrants to the United States and Their Descendants. J Natl Cancer Inst. 1994;86:4.
Chuang E, Christos P, Flam A, McCarville K, Forst M, Shin S, et al. Breast cancer subtypes in Asian-Americans differ according to Asian Ethnic group. J Immigr Minor Health. 2012;14:754–8.
Iqbal J, Ginsburg O, Rochon PA, Sun P, Narod SA. Differences in breast cancer stage at diagnosis and cancer-specific survival by race and ethnicity in the United States. JAMA. 2015;313:165–73.
Gelber RP, McCarthy EP, Davis JW, Seto TB. Ethnic disparities in breast cancer management among Asian Americans and Pacific Islanders. Ann Surg Oncol. 2006;13:977–84.
Giddings BH, Kwong SL, Parikh-Patel A, Bates JH, Snipes KP. Going against the tide: increasing incidence of colorectal cancer among Koreans, Filipinos, and South Asians in California, 1988–2007. Cancer Causes Control. 2012;23:691–702.
Lin SS, Clarke CA, Prehn AW, Glaser SL, West DW, O’Malley CD. Survival differences among Asian subpopulations in the United States after prostate, colorectal, breast, and cervical carcinomas. Cancer. 2002;94:1175–82.
Chien C, Morimoto LM, Tom J, Li CI. Differences in colorectal carcinoma stage and survival by race and ethnicity. Cancer. 2005;104:629–39.
Lee E, Liu L, Zhang J, Stern MC, Barzi A, Hwang A, et al. Stomach cancer disparity among Korean Americans by tumor characteristics: comparison with non-Hispanic whites, Japanese Americans, South Koreans, and Japanese. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol. 2017;26:587–96.
Kim J, Mailey B, Senthil M, Artinyan A, Sun C-L, Bhatia S. Disparities in gastric cancer outcomes among Asian ethnicities in the USA. Ann Surg Oncol. 2009;16:2433–41.
Kwong SL, Stewart SL, Aoki CA, Chen MS. Disparities in hepatocellular carcinoma survival among Californians of Asian ancestry, 1988 to 2007. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol. 2010;19:2747–57.
Stewart SL, Kwong SL, Bowlus CL, Nguyen TT, Maxwell AE, Bastani R, et al. Racial/ethnic disparities in hepatocellular carcinoma treatment and survival in California, 1988–2012. World J Gastroenterol. 2016;22:8584.
Cheng I, Le GM, Noone A-M, Gali K, Patel M, Haile RW, et al. Lung cancer incidence trends by histology type among Asian American, Native Hawaiian, and Pacific Islander populations in the United States, 1990–2010. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol. 2014;23:2250–65.
Epplein M, Schwartz SM, Potter JD, Weiss NS. Smoking-adjusted lung cancer incidence among Asian-Americans (United States). Cancer Causes Control. 2005;16:1085–90.
Raz DJ. Epidemiology of non-small cell lung cancer in Asian Americans: incidence patterns among six subgroups by nativity. J Thorac Oncol. 2008;3:7.
Trinh Q-D, Nguyen PL, Leow JJ, Dalela D, Chao GF, Mahal BA, et al. Cancer-specific mortality of Asian Americans diagnosed with cancer: a nationwide population-based assessment. JNCI J Natl Cancer Inst. 2015;107:djv054–djv054.
Daniel Carreon J, Morton LM, Devesa SS, Clarke CA, Gomez SL, Glaser SL, et al. Incidence of lymphoid neoplasms by subtype among six Asian ethnic groups in the United States, 1996–2004. Cancer Causes Control. 2008;19:1171–81.
Bates JH, Hofer BM, Parikh-Patel A. Cervical cancer incidence, mortality, and survival among Asian subgroups in California, 1990–2004. Cancer. 2008;113:2955–63.
Wang JH, Sheppard VB, Schwartz MD, Liang W, Mandelblatt JS. Disparities in cervical cancer screening between Asian American and Non-Hispanic white women. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol. 2008;17:1968–73.
Chao GF, Krishna N, Aizer AA, Dalela D, Hanske J, Li H, et al. Asian Americans and prostate cancer: a nationwide population-based analysis. Urol Oncol Semin Orig Investig. 2016;34:233.e7-233.e15.
Robbins AS, Koppie TM, Gomez SL, Parikh-Patel A, Mills PK. Differences in prognostic factors and survival among white and Asian men with prostate cancer, California, 1995–2004. 2007;9.
Huang ZJ, Zheng C. Type 2 diabetes among 6 Asian ethnic groups in California: the nexus of ethnicity, gender, and generational status. J Health Care Poor Underserved. 2015;26:16–35.
Islam NS, Wyatt LC, Kapadia SB, Rey MJ, Trinh-Shevrin C, Kwon SC. Diabetes and associated risk factors among Asian American subgroups in New York City. Diabetes Care. 2013;36:e5.
Kanaya AM, Herrington D, Vittinghoff E, Ewing SK, Liu K, Blaha MJ, et al. Understanding the high prevalence of diabetes in U.S. south Asians compared with four racial/ethnic groups: the MASALA and MESA studies. Diabetes Care. 2014;37:1621–8.
Karter AJ, Schillinger D, Adams AS, Moffet HH, Liu J, Adler NE, et al. Elevated rates of diabetes in Pacific Islanders and Asian subgroups: the Diabetes Study of Northern California (DISTANCE). Diabetes Care. 2013;36:574–9.
Lee JWR, Brancati FL, Yeh H-C. Trends in the prevalence of type 2 diabetes in Asians versus whites: results from the United States National Health Interview Survey, 1997–2008. Diabetes Care. 2011;34:353–7.
Mui P, Bowie JV, Juon H-S, Thorpe RJ. Ethnic group differences in health outcomes among Asian American Men in California. Am J Mens Health. 2017;11:1406–14.
Shah AM, Guo L, Magee M, Cheung W, Simon M, LaBreche A, et al. Comparing selected measures of health outcomes and health-seeking behaviors in Chinese, Cambodian, and Vietnamese communities of Chicago: results from local health surveys. J Urban Health Bull N Y Acad Med. 2010;87:813–26.
Shih M, Du Y, Lightstone AS, Simon PA, Wang MC. Stemming the tide: rising diabetes prevalence and ethnic subgroup variation among Asians in Los Angeles County. Prev Med. 2014;63:90–5.
Wang EJ, Wong EC, Dixit AA, Fortmann SP, Linde RB, Palaniappan LP. Type 2 diabetes: identifying high risk Asian American subgroups in a clinical population. Diabetes Res Clin Pract. 2011;93:248–54.
Choi SE, Liu M, Palaniappan LP, Wang EJ, Wong ND. Gender and ethnic differences in the prevalence of type 2 diabetes among Asian subgroups in California. J Diabetes Complications. 2013;27:429–35.
Kanaya AM, Adler N, Moffet HH, Liu J, Schillinger D, Adams A, et al. Heterogeneity of diabetes outcomes among Asians and pacific islanders in the US: the diabetes study of northern california (DISTANCE). Diabetes Care. 2011;34:930–7.
Bhalla V, Zhao B, Azar KMJ, Wang EJ, Choi S, Wong EC, et al. Racial/ethnic differences in the prevalence of proteinuric and nonproteinuric diabetic kidney disease. Diabetes Care. 2013;36:1215–21.
Maskarinec G, Katz AR. Prevalence of systemic lupus erythematosus in Hawaii: is there a difference between ethnic groups? Hawaii Med J. 1995;54:406–9.
Hur K, Wong M, Lee J, Lee J, Juon H-S. Hepatitis B infection in the Asian and Latino communities of Alameda County. California J Community Health. 2012;37:1119–26.
Juon H-S, Ha E, Kim F, Trang A, Pan J, Blanchard J. Prevalence of viral hepatitis in foreign-born populations in the Baltimore-Washington Metropolitan Area, 2009–2015. J Community Health. 2019;44:203–7.
Misra R, Jiobu K, Zhang J, Liu Q. Racial disparities in hepatitis B infection in Ohio: screening and immunization are critical for early clinical management. J Investig Med. 2013;61:8.
Noah AJ. Heterogeneity of hepatitis B infection among pregnant Asian American and Pacific islander women. Am J Prev Med. 2018;55:213–21.
Manangan LP, Salibay CJ, Wallace RM, Kammerer S, Pratt R, McAllister L, et al. Tuberculosis among persons born in the Philippines and living in the United States, 2000–2007. Am J Public Health. 2011;101:101–11.
Jose PO, Frank ATH, Kapphahn KI, Goldstein BA, Eggleston K, Hastings KG, et al. Cardiovascular disease mortality in Asian Americans. J Am Coll Cardiol. 2014;64:2486–94.
Palaniappan L, Wang Y, Fortmann SP. Coronary heart disease mortality for six ethnic groups in California, 1990–2000. Ann Epidemiol. 2004;14:499–506.
Wild SH, Laws A, Fortmann SP, Varady AN, Byrne CD. Mortality from coronary heart disease and stroke for six ethnic groups in California, 1985 to 1990. Ann Epidemiol. 1995;5:432–9.
Holland AT, Wong EC, Lauderdale DS, Palaniappan LP. Spectrum of cardiovascular diseases inAsian-American racial/ethnic subgroups. Ann Epidemiol. 2011;21:608–14.
Frank ATH, Zhao B, Jose PO, Azar KMJ, Fortmann SP, Palaniappan LP. Racial/ethnic differences in dyslipidemia patterns. Circulation. 2014;129:570–9.
Carlisle SK. Disaggregating race and ethnicity in chronic health conditions: implications for public health social work. Soc Work Public Health. 2014;29:616–28.
Jung MY, Lee S, Thomas SB, Juon H-S. Hypertension prevalence, treatment, and related behaviors among Asian Americans: an examination by method of measurement and disaggregated subgroups. J Racial Ethn Health Disparities. 2019;6:584–93.
Lloyd-Jones DM, Sutton-Tyrrell K, Patel AS, Matthews KA, Pasternak RC, Everson-Rose SA, et al. Ethnic variation in hypertension among premenopausal and perimenopausal women: Study of Women’s Health Across the Nation. Hypertens Dallas Tex. 1979;2005(46):689–95.
Park S-Y, Shibusawa T, Yoon SM, Son H. Characteristics of Chinese and Korean Americans in outpatient treatment for alcohol use disorders: examining heterogeneity among Asian American subgroups. J Ethn Subst Abuse. 2010;9:128–42.
Bersamira CS, Lin Y-A, Park K, Marsh JC. Drug use among Asian Americans: Differentiating use by acculturation status and gender. J Subst Abuse Treat. 2017;79:76–81.
Bromberger JT, Harlow S, Avis N, Kravitz HM, Cordal A. Racial/ethnic differences in the prevalence of depressive symptoms among middle-aged women: The Study of Women’s Health Across the Nation (SWAN). Am J Public Health. 2004;94:1378–85.
Lee S, Choi S, Matejkowski J. Comparison of major depressive disorder onset among foreign-born Asian Americans: Chinese, Filipino, and Vietnamese ethnic groups. Psychiatry Res. 2013;210:315–22.
Hoyert DL. Asian or Pacific Islander Mortality, Selected States, 1992. Mon Vital Stat Rep. 1997;46:64.
Hastings KG, Jose PO, Kapphahn KI, Frank ATH, Goldstein BA, Thompson CA, et al. Leading causes of death among Asian American Subgroups (2003–2011). Chaturvedi V, editor. PLOS ONE. 2015;10:e0124341.
Lauderdale DS, Kestenbaum B. Mortality rates of elderly Asian American populations based on Medicare and Social Security data. Demography. 2002;39:529–40.
Wu B, Liang J, Landerman L, Plassman B. Trends of edentulism among middle-aged and older Asian Americans. Am J Public Health. 2013;103:7.
Lauderdale DS, Jacobsen SJ, Furner SE, Levy PS, Brody JA, Goldberg J. Hip fracture incidence among elderly Asian-American populations. Am J Epidemiol. 1997;146:502–9.
Patel MC, Chandra M, Lo JC. Mortality following hip fracture in Chinese, Japanese, and Filipina women. Am J Manag Care. 2016;22:e358–9.
Park CB, Braun KL, Horiuchi BY, Tottori C, Onaka AT. Longevity disparities in multiethnic Hawaii: an Analysis of 2000 Life Tables. Public Health Rep. 2009;124:579–84.
Rao AK, Daniels K, El-Sayed YY, Moshesh MK, Caughey AB. Perinatal outcomes among Asian American and Pacific Islander women. Am J Obstet Gynecol. 2006;195:834–8.
Wong LF, Caughey AB, Nakagawa S, Kaimal AJ, Tran SH, Cheng YW. Perinatal outcomes among different Asian-American subgroups. Am J Obstet Gynecol. 2008;199:382.e1-382.e6.
Cripe SM, O’Brien W, Gelaye B, Williams MA. Perinatal Outcomes of Southeast Asians with Pregnancies Complicated by Gestational Diabetes Mellitus or Preeclampsia. J Immigr Minor Health. 2012;14:747–53.
Rao AK, Cheng YW, Caughey AB. Perinatal complications among different Asian-American subgroups. Am J Obstet Gynecol. 2006;194:e39-41.
Vang ZM, Elo IT, Nagano M. Preterm birth among the hmong, other Asian subgroups and non-hispanic whites in California. BMC Pregnancy Childbirth. 2015;15:184.
Fuentes-Afflick E, Hessol NA. Impact of Asian ethnicity and national origin on infant birth weight. Am J Epidemiol. 1997;145:148–55.
Wang X, Strobino DM, Guyer B. Differences in cause-specific infant mortality among Chinese, Japanese, and white Americans. Am J Epidemiol. 1992;135:1382–93.
Mui P, Hill SE, Thorpe RJ. Overweight and obesity differences across ethnically diverse subgroups of Asian American Men. Am J Mens Health. 2018;12:1958–65.
Staimez L, Weber M, Narayan K, Oza-Frank R. A systematic review of overweight, obesity, and type 2 diabetes among Asian American Subgroups. Curr Diabetes Rev. 2013;9:312–31.
Hwang H. Colorectal cancer screening among Asian Americans. Asian Pac J Cancer Prev APJCP. 2013;14:4025–32.
NAMI. Mental Health By the Numbers [Internet]. nami.org. 2021. Available from: https://www.nami.org/mhstats
Division (DCD) DC. Opioid Crisis Statistics [Internet]. HHS.gov. https://plus.google.com/+HHS; 2018 [cited 2021 Sep 6]. Available from: https://www.hhs.gov/opioids/about-the-epidemic/opioid-crisis-statistics/index.html
Becerra MB, Becerra BJ. Disparities in age at diabetes diagnosis among Asian Americans: Implications for Early Preventive Measures. Prev Chronic Dis. 2015;12:E146.
Chu SY, Abe K, Hall LR, Kim SY, Njoroge T, Qin C. Gestational diabetes mellitus: all Asians are not alike. Prev Med. 2009;49:265–8.
Nguyen H-AT, Zheng A, Gugel A, Kistin CJ. Asians and Asian Subgroups are underrepresented in Medical Research Studies Published in High-Impact Generalist Journals. J Immigr Minor Health. 2021;23:646–9.
Ðoàn LN, Takata Y, Sakuma K-LK, Irvin VL. Trends in clinical research including Asian American, Native Hawaiian, and Pacific Islander Participants Funded by the US National Institutes of Health, 1992 to 2018. JAMA Netw Open. 2019;2:e197432.
Further demographic analyses of NIH R01 grant outcomes of T32 postdoctoral participants—NIH Extramural Nexus [Internet]. [cited 2021 Sep 4]. Available from: https://nexus.od.nih.gov/all/2021/07/27/further-demographic-analyses-of-nih-r01-grant-outcomes-of-t32-postdoctoral-participants/
Populations underrepresented in the extramural scientific workforce | SWD at NIH [Internet]. [cited 2021 Sep 4]. Available from: https://diversity.nih.gov/about-us/population-underrepresented
Doan LN, Takata Y, Sakuma K-LK, Irvin VL. Trends in clinical research including Asian American, Native Hawaiian, and Pacific Islander Participants Funded by the US National Institutes of Health, 1992 to 2018. JAMA Netw Open. 2019;2:e197432.
Kim W, Keefe RH. Barriers to healthcare among Asian Americans. Soc Work Public Health. 2010;25:286–95.
Lee S, Martinez G, Ma GX, Hsu CE, Robinson ES, Bawa J, et al. Barriers to health care access in 13 Asian American communities. Am J Health Behav. 2010;34:21–30.
Kauh TJ, Read JG, Scheitler AJ. The critical role of racial/ethnic data disaggregation for health equity. Popul Res Policy Rev. 2021;1–7.
Arroyo-Johnson C, Mincey KD, Ackermann N, Milam L, Goodman MS, Colditz GA. Racial and ethnic heterogeneity in self-reported diabetes prevalence trends across Hispanic subgroups, National Health Interview Survey, 1997–2012. Prev Chronic Dis. 2016;13:E10.
Griffith DM, Johnson JL, Zhang R, Neighbors HW, Jackson JS. Ethnicity, nativity, and the health of American Blacks. J Health Care Poor Underserved. 2011;22:142–56.
Bureau UC. Census Bureau Reports at Least 350 Languages Spoken in U.S. Homes [Internet]. U. S. Census Bur. 2015 [cited 2021 Jun 17]. Available from: https://www.census.gov/newsroom/press-releases/2015/cb15-185.html
Zeigler K, Camarota SA. 67.3 Million in the United States Spoke a Foreign Language at Home in 2018 [Internet]. Cent. Immigr. Stud. 2019 [cited 2021 Jun 17]. Available from: https://cis.org/Report/673-Million-United-States-Spoke-Foreign-Language-Home-2018
Islam NS, Khan S, Kwon S, Jang D, Ro M, Trinh-Shevrin C. Methodological issues in the collection, analysis, and reporting of granular data in Asian American populations: historical challenges and potential solutions. J Health Care Poor Underserved. 2010;21:1354–81.
Shimkhada R, Scheitler AJ, Ponce NA. Capturing racial/ethnic diversity in population-based surveys: data disaggregation of health data for Asian American, Native Hawaiian, and Pacific Islanders (AANHPIs). Popul Res Policy Rev. 2021;40:81–102.
Nguyen B-MD, Nguyen MH, Nguyen T-LK. Advancing the Asian American and Pacific Islander data quality campaign: Data disaggregation practice and policy. Asian Am Policy Rev. 2014;24:55–67.
Stacciarini J-MR, Shattell MM, Coady M, Wiens B. Review: community-based participatory research approach to address mental health in minority populations. Community Ment Health J. 2011;47:489–97.
Parra‐Cardona R, Beverly HK, López‐Zerón G. Community‐based participatory research (CBPR) for underserved populations. In: Wampler KS, McWey LM, editors. Handb Syst Fam Ther [Internet]. 1st ed. Wiley; 2020 [cited 2021 Jun 27]. p. 491–511. Available from: https://onlinelibrary.wiley.com/doi/abs/https://doi.org/10.1002/9781119438519.ch21
CDC. Cases, Data, and Surveillance [Internet]. Cent. Dis. Control Prev. 2020 [cited 2021 Sep 6]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html
Wang D, Gee GC, Bahiru E, Yang EH, Hsu JJ. Asian-Americans and Pacific Islanders in COVID-19: emerging disparities amid Discrimination. J Gen Intern Med. 2020;35:3685–8.
South Carolina County-Level Data for COVID-19 | SCDHEC [Internet]. [cited 2021 Sep 6]. Available from: https://scdhec.gov/covid19/covid-19-data/south-carolina-county-level-data-covid-19
Home [Internet]. Fla. Dep. Health COVID-19 Outbreak. [cited 2021 Sep 6]. Available from: https://floridahealthcovid19.gov/
Albert MA, Glynn RJ, Buring J, Ridker PM. C-reactive protein levels among women of various ethnic groups living in the United States (from the Women’s Health Study). Am J Cardiol. 2004;93:1238–42.
Foiles Sifuentes AM, Robledo Cornejo M, Li NC, Castaneda-Avila MA, Tjia J, Lapane KL. The role of limited English proficiency and access to health insurance and health care in the affordable care act era. Health Equity. 2020;4(1):509–17.
Suarez NR, Urtecho M, Nyquist CA, Jaramillo C, Yeow ME, Thorsteinsdottir B, Wilson ME, Barwise AK. Consequences of suboptimal communication for patients with limited English proficiency in the intensive care unit and suggestions for a way forward: a qualitative study of healthcare team perceptions. J Crit Care. 2021;61:247–51.
Jacobs ZG, Prasad PA, Fang MC, Abe-Jones Y, Kangelaris KN. The association between limited English proficiency and sepsis mortality. J Hosp Med. 2020;15(3):140.
Funding
Lor was supported by the National Institute of Nursing Research of the National Institutes of Health under Award Number K23NR019289. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yom, S., Lor, M. Advancing Health Disparities Research: The Need to Include Asian American Subgroup Populations. J. Racial and Ethnic Health Disparities 9, 2248–2282 (2022). https://doi.org/10.1007/s40615-021-01164-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-021-01164-8