Abstract
Background
Peritonectomy is an important component in surgical treatment for peritoneal surface malignancies. Visual inspection and palpation to estimate the extent of tumor involvement are unreliable. Most gynecologic oncologists are skeptical regarding the benefits of complete peritonectomy and do not perform them, worrying about the benefit and associated morbidity. They believe it is the inherent tumor biology that determines the resectability of the tumor, not surgical aggressiveness. The aim of this study was to assess the recurrence pattern, oncological outcomes, morbidity and mortality based on the extent of parietal peritonectomy performed during CRS and HIPEC in stage IIIc epithelial ovarian cancers.
Methods
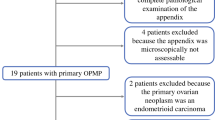
Patients diagnosed with stage IIIc epithelial carcinoma ovary underwent selective parietal peritonectomy (SPP) or complete parietal peritonectomy (CPP) with CRS–HIPEC. All pre- and intraoperative data were compared and analyzed with main focus on postoperative morbidity, mortality, recurrence pattern and oncological outcomes.
Results
From February 2013 to December 2017, 110 patients with stage IIIc epithelial ovarian cancers underwent CRS–HIPEC of which 20 were upfront primary, 55 had interval surgery and 35 were recurrent cases. Forty and 70 patients underwent CPP and SPP, respectively. The median peritoneal cancer index was 14 for CPP and 10 for SPP. CPP group had longer duration of surgery (10.7 vs. 8.9 h) and more blood loss (1062 vs. 653 ml) when compared to SPP group. The morbidity was more common in SPP group 26 (37%) than CPP group 20 (50%), and it was not statistically significant (p = 0.133). There was equal number of operative mortality in both groups: CPP versus SPP—3 (7.5%) versus 3 (4.2%), p = 0.406. With a median follow-up of 45 months, progression-free survival (PFS) was significantly higher in CPP group (33 months vs. 25 months, p < 0.05) and median overall survival (OS) was 48 months in SPP group (yet to be achieved in CPP group). The 3-year PFS was 42% versus 38%. The 3-year OS was 80% for CPP and 75% for SPP. In 30% (12 of 40 patients) undergoing CPP, pathologic examination detected microscopic disease involvement in parietal peritoneum with no visually evident tumor at surgery by the surgeon.
Conclusions
Patients who underwent complete peritonectomy had significantly higher PFS. This indicates aggressive surgical resection has a benefit with manageable postoperative morbidity. However, longer follow-up and a prospective randomized study need to be designed for more evidence of the same.


Similar content being viewed by others
References
van Driel WJ, Koole SN, Sikorska K, Schagen van Leeuwen JH, Schreuder HW, Hermans RH, et al. Hyperthermic intraperitoneal chemotherapy in ovarian cancer. N Engl J Med. 2018;378:230–40.
Griffiths CT. Surgical resection of tumor bulk in the primary treatment of ovarian carcinoma. Natl Cancer Inst Monogr. 1975;42:101–4.
Hoskins WJ, McGuire WP, Brady MF, Homesley HD, CreasmanWT Berman M, et al. The effect of diameter of largest residual disease on survival after primary cytoreductive surgery in patients with suboptimal residual epithelial ovarian carcinoma. Am J Obstet Gynecol. 1994;170:974–9.
Bookman MA. Optimal primary therapy of ovarian cancer. Ann Oncol. 2016;27(Suppl 1):i58–62.
Chi DS, Eisenhauer EL, Zivanovic O, et al. Improved progression- free and overall survival in advanced ovarian cancer as a result of a change in surgical paradigm. Gynecol Oncol. 2009;114:26–31.
Bristow RE, Chi DS. Platinum-based neoadjuvant chemotherapy and interval surgical cytoreduction for advanced ovarian cancer: a meta-analysis. Gynecol Oncol. 2006;103:1070–6.
Eisenkop SM, Spirtos NM, Friedman RL, Lin WC, Pisani AL, Perticucci S. Relative influences of tumor volume before surgery and the cytoreductive outcome on survival for patients with advanced ovarian cancer: a prospective study. Gynecol Oncol. 2003;90:390–6.
Baratti D, Kusamura S, Cabras AD, Deraco M. Cytoreductive surgery with selective versus complete parietal peritonectomy followed by hyperthermic intraperitoneal chemotherapy in patients with diffuse malignant peritoneal mesothelioma: a controlled study. Ann Surg Oncol. 2012;19:1416–24.
Sugarbaker PH, editor. Peritoneal carcinomatosis: principles of management. Boston: Kluwer Academic; 1996.
Somashekhar SP, Ashwin KR, Kumar R, Natraj N, Ramya Y, Shabber SZ, et al. Standardization of patient selection and hyperthermic intraperitoneal chemotherapy protocol for peritoneal surface malignancy in Indian patients IJGO; 2017. https://doi.org/10.1007/s40944-017-0154-9.
Common Terminology Criteria for Adverse Events (CTCAE) version 4.0 (v4.03: June 14, 2010). U.S. Department of Health and Human Services, National Institutes of Health. Bethesda: National Cancer Institute; 2009.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–96.
Hynninen J, Laasik M, Vallius T, Kemppainen J, Grönroos S, Virtanen J, et al. Clinical value of 18F-fluorodeoxyglucose positron emission tomography/computed tomography in response evaluation after primary treatment of advanced epithelial ovarian cancer. Clin Oncol. 2018;30(8):507–14.
Hillemanns P, Wimberger P, Reif J, Stepp H, Klapdor R. Photodynamic diagnosis with 5-aminolevulinic acid for intraoperative detection of peritoneal metastases of ovarian cancer: a feasibility and dose finding study. Lasers Surg Med. 2017;49:169–76. https://doi.org/10.1002/lsm.22613.
Hynninen Johanna, Lavonius Maija, Oksa Sinikka, Grénman Seija, Carpén Olli, Auranen Annika. Is perioperative visual estimation of intra-abdominal tumor spread reliable in ovarian cancer surgery after neoadjuvant chemotherapy? Gynecol Oncol. 2013;128(2):229–32. https://doi.org/10.1016/j.ygyno.2012.11.007.
Acknowledgements
The authors thank Dr. Arun Kumar, Consultant Biostatistician, for statistical analysis and sample size calculation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
conflict of interest
The authors declare that they have no competing interests.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.


Rights and permissions
About this article
Cite this article
Somashekhar, S.P., Ashwin, K.R., Kumar, R. et al. Comparison of Outcomes Following Complete and Selective Parietal Peritonectomy During Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy for Advanced Epithelial Ovarian Cancer: A Study by Indian Society of Peritoneal Surface Malignancies (ISPSM). Indian J Gynecol Oncolog 16, 71 (2018). https://doi.org/10.1007/s40944-018-0241-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40944-018-0241-6