Introduction
For several decades, mental health policies and practices across Europe have focused on shifting the balance from hospital-based to integrated community-based services (Thornicroft and Tansella, Reference Thornicroft and Tansella2003, Reference Thornicroft and Tansella2004; Knapp et al., Reference Knapp, Beecham, McDaid, Matosevic and Smith2011). In most developed countries, the balance and mix of services have changed in response to new policy directions and to demands for more individualised psycho-social interventions (Thornicroft and Tansella, Reference Thornicroft and Tansella2005). For example, personalisation is a prominent policy aspiration in England, aiming to enhance choice and control for people using both health and social care services (Larsen et al., Reference Larsen, Ainsworth, Harrop, Patterson, Hamilton, Szymczynska, Tew, Manthorpe and Pinfold2013). Moreover, there is a growing interest in recovery-oriented treatments within mental health. Thus, the relevance of interventions to promote social re-engagement, such as getting a job, or making new friends, or learning new skills, has been acknowledged (Slade, Reference Slade2009; Knapp et al., Reference Knapp, Andrew, McDaid, Iemmi, McCrone, Park, Parsonage, Boardman and Shepherd2014; Slade et al., Reference Slade, McDaid, Shepherd, Williams and Repper2017). All these initiatives were further enhanced by approval of the World Health Organization (WHO) ‘Framework on Integrated People-Centred Health Services’ in 2016. This highlighted the need to rebalance care provision towards inclusive community care by promoting care integration and coordination across provider settings (WHO, 2016). The emergence of the discipline of ‘health care delivery science’ advocating for better standards and tools for the international comparison of universal access and service variation across geographical areas (Mulley et al., Reference Mulley, Wennberg, Weinstein, Fisher and Binagwaho2013) has also been helpful.
Despite this reorientation, discussion of the funding, planning and delivery of European mental health services is not grounded in evidence from actual comparisons of integrated service availability and capacity across geographical areas. It is therefore important in any comparative analysis of mental health across Europe to incorporate service provision delivered outside the health care sector and understand the interfaces between these other services and core health care (McDaid et al., Reference McDaid, Oliveira, Jurczak and Knapp2007).
The boundaries between service provision delivered through the health system and those delivered elsewhere are far from clear and can vary substantially within and across countries. What is regarded as a health v. a non-health or social service also depends on country-specific regulations and financing mechanisms (Straßmayr et al., Reference Straßmayr, Katschnig, Amaddeo, Brunn, Cetrano, Chevreul, Cid, McDaid, Järvelin, Kalseth, Kalseth, Malin, Matosevic, Pauna, Salvador-Carulla and Sfetcu2013). There are also different levels of decentralisation and devolution for health and other services. These differences may mean that if the focus is on health care systems, two countries with similar mixes of services may appear to have very different levels of service availability, depending on the extent to which services lie within the health care system (McDaid et al., Reference McDaid, Oliveira, Jurczak and Knapp2007). Problems of comparability are even more evident when exploring interfaces with services provided in other sectors.
Moves towards a standardised classification system to facilitate descriptions of mental health services across different geographical areas and settings have evolved over the last two decades. For example, the Description and Evaluation of Services and Directories in Europe for Long Term Care (DESDE-LTC), an evolution of the European Service Mapping Schedule (ESMS) for the evaluation of services in mental health (Johnson et al., Reference Johnson and Kuhlmann2000), was developed as a means of standardising descriptions and classifications of services (Salvador-Carulla et al., Reference Salvador-Carulla, Poole, González-Caballero, Romero, Salinas and Lagares-Franco2006, Reference Salvador-Carulla, Alvarez-Galvez, Romero, Gutiérrez Colosía, Weber, McDaid, Dimitrov, Sprah, Kalseth, Tibaldi, Salinas-Perez, Lagares-Franco, Romá-Ferri and Johnson2013).
DESDE-LTC is used to distinguish between core health and other care provision. ‘Core health care’ refers to services whose explicit aim is direct clinical treatment (in this case for mental health problems) usually provided by health professionals with over 3 years of training in health sciences (i.e., physicians, nurses, psychologists, physiotherapists) (WHO, 2006). ‘Other care’ is typically provided by other staff and its main aim is not direct and highly specialised clinical treatment. It typically includes accommodation, training, promotion of independence and autonomy, case management, employment support and social skills. It also implies more integration, inclusion, social participation and encouragement of mental, as well as social capital, within communities (Slade et al., Reference Slade, Amering, Farkas, Hamilton, O'Hagan, Panther, Perkins, Shepherd, Tse and Whitley2014; Thornicroft et al., Reference Thornicroft, Szmukler, Mueser and Drake2011, Reference Thornicroft, Deb and Henderson2016). This classification draws on similar constructs used elsewhere, such as by the International Classification of Functioning, Disability and Health (ICF) (WHO, 2013), which distinguishes between ‘health professionals’ and ‘other professionals’. The International Standard Classification of Occupations (ISCO-08) (ILO, 2012) identifies different health workforce subgroups (mainly health and associate professionals) according to assumed differences in skill level and specialisation required to fulfil job tasks and duties. This approach has also been followed by the System of Health Accounts (SHA 2.0) produced by OECD, Eurostat and WHO (OECD, 2011).
The definition ‘other care’ (or ‘associated care’ according to the OECD terminology) does not necessarily mean being funded or governed differently. The DESDE-LTC typology concentrates on the main activity provided by the service rather than funding source and governance structure. Such a functional approach is innovative as it avoids traditional comparisons based on the agency/department responsible for the oversight and governance of specific services. These have proved problematic due to wide geographical variations across European mental health services. Therefore, the DESDE-LTC classification allows for separate analysis and comparison of groups of services undertaking similar activities and provided in similar settings to facilitate territorial comparisons of like-with-like (Salvador-Carulla et al., Reference Salvador-Carulla, Poole, González-Caballero, Romero, Salinas and Lagares-Franco2006, Reference Salvador-Carulla, Alvarez-Galvez, Romero, Gutiérrez Colosía, Weber, McDaid, Dimitrov, Sprah, Kalseth, Tibaldi, Salinas-Perez, Lagares-Franco, Romá-Ferri and Johnson2013; Gutierrez-Colosía et al., Reference Gutiérrez-Colosía, Salvador-Carulla, Salinas-Pérez, García-Alonso, Cid, Salazzari, Montagni, Tedeschi, Cetrano, Chevreul, Kalseth, Hagmair, Straßmayr, Park, Sfetcu, Ala-Nikkola, González-Caballero, Rabbi, Kalseth and Amaddeo2017).
Undertaken as part of the European Union funded REFINEMENT project (REsearch on FINancing systems’ Effect on the quality of MENTal health care) (http://www.refinementproject.eu), which compared differences in financing mechanisms to understand their impact on the quality and efficiency of European mental health systems, the two main aims of this specific analysis were:
(1) To use DESDE-LTC to identify and compare core health and other care services provided to people with mental health problems in selected areas of eight European countries.
(2) To investigate the balance of care by analysing the types (residential, outpatient, day care), target group (mental health v. general health) and characteristics (staff and bed availability) of services that provide core health and other care in selected areas.
Method
Instruments
This present paper draws on data collected within the REFINEMENT project using the REMAST tool (Refinement Mapping Services Tool). This tool has five main sections (Table 1), with the focus on the MHSI (Mental Health Services Inventory) used to classify and describe mental health services in the eight study areas. The core of the MHSI is represented by DESDE-LTC, which provides most of the information needed to complete this inventory. The feasibility, reliability and validity of DESDE-LTC has previously been described (Salvador-Carulla et al., Reference Salvador-Carulla, Atienza, Romero, Guimon and Sartorius2000, Reference Salvador-Carulla, Dimitrov, Weber, McDaid, Venner, Sprah, Romero, Ruiz, Tibaldi and Johnson2011a, Reference Salvador-Carulla, Romero, Weber, Dimitrov, Sprah, Venner and McDaid2011b, Reference Salvador-Carulla, Alvarez-Galvez, Romero, Gutiérrez Colosía, Weber, McDaid, Dimitrov, Sprah, Kalseth, Tibaldi, Salinas-Perez, Lagares-Franco, Romá-Ferri and Johnson2013; Gutierrez-Colosía et al., Reference Gutiérrez-Colosía, Salvador-Carulla, Salinas-Pérez, García-Alonso, Cid, Salazzari, Montagni, Tedeschi, Cetrano, Chevreul, Kalseth, Hagmair, Straßmayr, Park, Sfetcu, Ala-Nikkola, González-Caballero, Rabbi, Kalseth and Amaddeo2017).
Table 1. Study instruments and data collection procedure
Study areas
Each of the eight countries (Austria, England, Finland, France, Italy, Norway, Romania and Spain) selected a study area with a population between 200 000 and 1 500 000 inhabitants, preferably not limited to a macro-urban area within a municipality. Detailed characteristics of the study areas are available on the REFINEMENT webpage (http://www.refinementproject.eu) and in Gutierrez-Colosía et al. (Reference Gutiérrez-Colosía, Salvador-Carulla, Salinas-Pérez, García-Alonso, Cid, Salazzari, Montagni, Tedeschi, Cetrano, Chevreul, Kalseth, Hagmair, Straßmayr, Park, Sfetcu, Ala-Nikkola, González-Caballero, Rabbi, Kalseth and Amaddeo2017).
Units of analysis
We focused on universally accessible publicly funded services that provided mental health care to adults (+18) meeting ICD-10 (International Classification of Diseases) F20–F69 disease classification criteria (WHO, 2010). This excluded services only accessible with fully private insurance or out-of-pocket payment without public reimbursement. Services for people with an ICD-10 diagnosis of organic mental disorders (F00-F09), psychoactive substance use (F10-19), intellectual disability (F70-79) and those for child and adolescent disorders were excluded as they are provided by a separate system in many countries. To classify and compare services, the operational definitions of Basic Stable Inputs of Care (BSIC) and Main Type of Care (MTC) were used (Table 1).
Data analysis
All MTCs in the study areas were analysed separately according to whether they provided core health or other care. Table 2 illustrates DESDE-LTC codes included in each of the two groups.
Table 2. Taxonomy of core health and other care provision for adults with mental health problems
a Main goal is the specific clinical care and at least 20% of the staff is qualified health care professionals.
Both at the overall level and for each study area, the total number of MTCs providing health and other care and the number of MTCs per type of care and target group were computed, as well as the percentage of core health care and other care services as a share of total MTCs. In each study area, the rate of MTCs classified as core health care and other care per 100 000 adult population was also calculated. Services were considered ‘general health’ if they could be used by other users alongside mental health service users, whereas services with ‘mental health’ as target group were those providing care exclusively to people with mental health problems. General practitioners were not included in this analysis.
As for staff/bed availability, only data about services exclusively targeted at mental health service users were considered, since those for general health users were affected by missing data and our focus was on mental health provision.
The overall percentage of staff in core health and other MTCs was calculated, alongside the full-time equivalent staff rate per 100 000 adult population in each area. The percentages of each professional category in total staff numbers were determined for health and other MTCs. A composite indicator for multidisciplinary staff was created. Following Burns's (Reference Burns2004) definition, where there was at least one physician, one nurse, one psychologist and one social worker or occupational therapist, this was classified as multidisciplinary. Self-employed specialists were not included in this indicator since they typically work single-handedly. The global percentage of beds in all areas in health and other care MTCs was computed. Finally, in each area, the average, minimum and maximum number of beds per residential unit was considered, along with the total number of beds per 100 000 adults.
Results
Core health v. other care provision
Table 3 presents the distribution of health and other care services in the study areas. The total number of MTCs in the eight study areas was 1270. Overall, 822 MTCs (65%) provided core health care and 448 (35%) other care. Such ratios ranged from 22% in Suceava to 49% in Verona (Fig. 1).
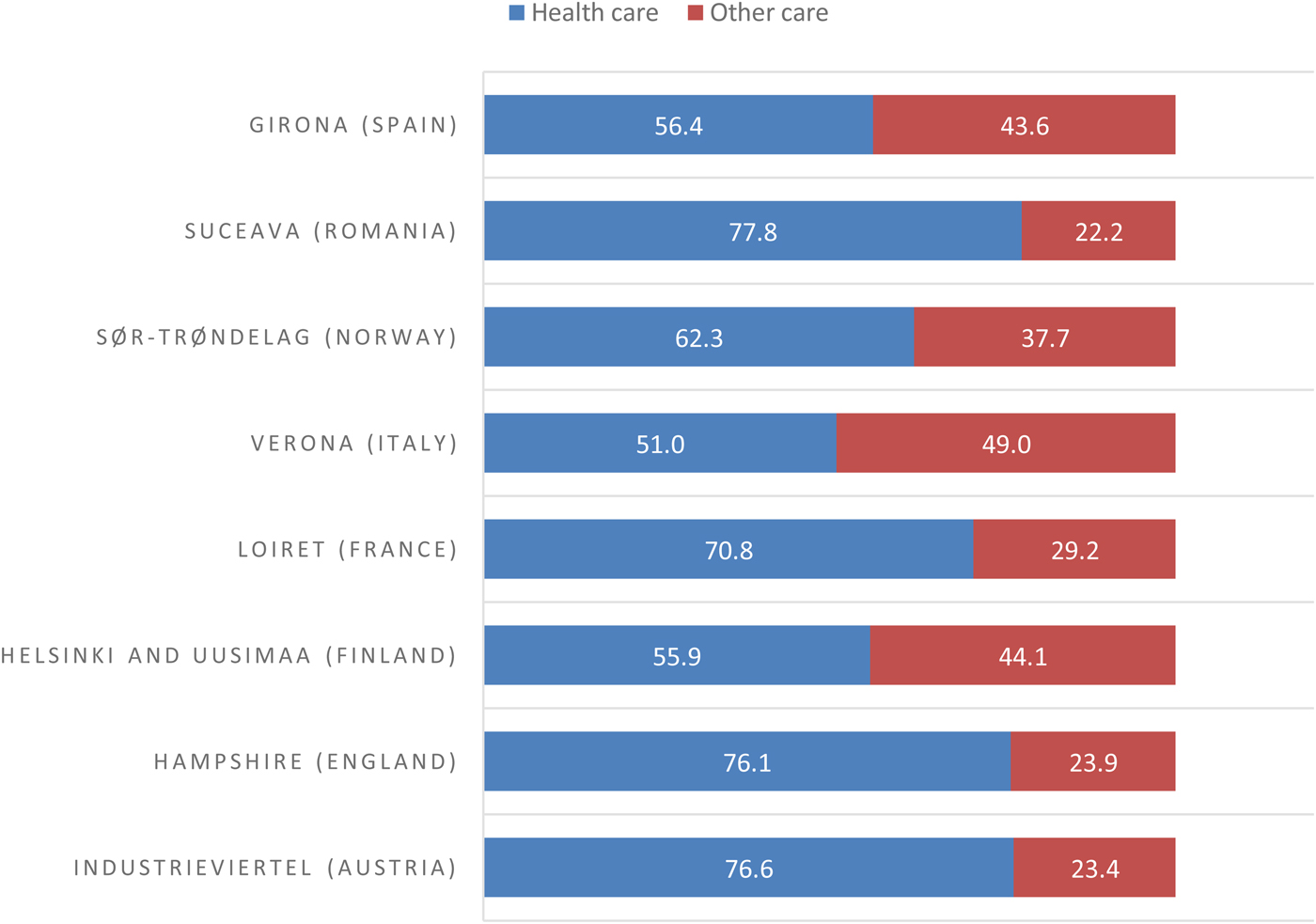
Fig. 1. Balance of care for people with mental health problems in eight European study areas.
Table 3. Comparison of core health and other care services in the field of mental health in eight European study areas
a The numbers in brackets refer to single-handed psychiatrists and psychologists.
b Such figures mainly reflect the results in the larger study areas.
In total, 156 residential services (MTCs) were classified as providing core health care and 205 other care. Looking at outpatient services, significantly more services were identified as providing health (595 MTCs) than other care (109 MTCs). This included 273 MTCs for single-handed psychiatrists and psychologists mapped in Industrieviertel, Loiret, Sør-Trøndelag and Suceava. Furthermore, 71 day care services (MTCs) were reported as health and 134 as other care related. Looking at the target group, 1018 were MTCs targeted specifically at people with mental health problems, while 252 were for generic users where at least 20% of users had a mental health problem. In most areas, day and residential care seemed to be the main forms of other care provision. The rate of ‘core health care’ and ‘other care’ services per 100 000 adult population varied from 4.9 and 1.4 in Suceava to 65.3 and 39.5 in Sør-Trøndelag, respectively.
In both Verona and Sør-Trøndelag, outpatient services made up a substantive proportion of other care services for people with mental health problems. This component was delivered by municipalities in Norway and local authority social services in Italy. Although such municipality services also operate in the other study areas, it was not possible to map them due to a lack of information.
MTCs characteristics
Table 4 shows the distribution of staff in health and other care services in the eight study areas. Overall 79% of staff worked in health care services and 21% in other care.
Table 4. Staff in core health and other care services (MTCs) in eight European study areasa
a Only services targeted exclusively at people with mental health problems were included here (N = 1018).
b Staff including at least one physician, one nurse, one psychologist and one social worker or occupational therapist. Single-handed professionals are not included in this indicator.
c The number in brackets refers to services for which data on staff are missing.
Beginning with health-related services, Sør-Trøndelag had the highest number of total staff per 100 000 adult population (359.8). In other care, this rate ranged from 2.6 in Hampshire to 78.6 in Suceava. Some rates may be underestimated due to missing data, especially in Hampshire where about 30% of services had insufficient data on staff.
In general, the staff rate was higher in health care rather than other services, with the exception of Suceava where the opposite was found.
In most areas, healthcare staff were predominantly nurses, including Hampshire, Helsinki and Uusimaa, Loiret, Sør-Trøndelag and Suceava. In Industrieviertel and Girona, physicians dominated, while in Verona, other staff were most common followed by nurses. In services that were not directly health-related, other staff comprised the highest number of staff in all areas, apart from Loiret where nurses predominated.
Multidisciplinary teams seemed to be a frequent model of health care provision in all areas. Suceava showed the highest percentage of services with multidisciplinary staff, both for health (90.0%) and other care (62.5%). After Suceava, Hampshire showed the highest proportion of health services with multidisciplinary staff (88.6%). Multidisciplinary teams were also common in health services in the Finnish area, with 60.1% of services having this element in place. In the other areas, this percentage ranged from 25.7 to 46.7%. A multidisciplinary pattern was less common in services not providing core health care and missing in Industrieviertel, Hampshire, Helsinki and Uusimaa, Sør-Trøndelag. However, missing data mean figures need cautious interpretation.
Table 5 shows great diversity among areas in availability of residential beds for people with mental health problems. In total, 45% of beds were located in health care services and 55% in services not providing direct health care. As far as health care services are concerned, the average number of beds per unit ranged from 13.9 in Verona to 75.0 in Suceava. In other care services, this average ranged from 3.4 in Loiret to 106.4 in Suceava. The highest rates of health care beds per 100 000 adult inhabitants were found in Helsinki and Uusimaa and Sør-Trøndelag. In other care services, the highest rates of beds were found in Helsinki and Uusimaa and Suceava.
Table 5. Provision of core health and other care in residential MTCs in eight European study areasa
a Only services targeted exclusively at people with mental health problems were included here.
Discussion
To our knowledge, this paper presents the first comprehensive analysis of mental health care provision in Europe following a holistic approach and using a standardised methodology based on service function or activity and not on name, funding or governance systems. In line with previous reports (WHO, 2011, 2014), our results show great diversity in provision of mental health services across Europe. As McDaid et al. (Reference McDaid, Oliveira, Jurczak and Knapp2007) point out, our findings demonstrate that a substantial part of mental health resources in Europe are delivered in services not classified as ‘core health care’. Our data also indicate that other care services play different roles in different countries, resulting in heterogeneous configurations of mental health care provision across Europe. Such diversity was further reflected in great variation among study areas in the availability of services per capita.
Looking at residential bed availability in health and other care services, Industrieviertel, Hampshire, Verona and Girona reported similar and relatively low rates, with Girona having the lowest bed rate in health care services. This pattern may be representative of a typology of care with a stronger community approach (Gutierrez-Colosía et al., Reference Gutiérrez-Colosía, Salvador-Carulla, Salinas-Pérez, García-Alonso, Cid, Salazzari, Montagni, Tedeschi, Cetrano, Chevreul, Kalseth, Hagmair, Straßmayr, Park, Sfetcu, Ala-Nikkola, González-Caballero, Rabbi, Kalseth and Amaddeo2017). In Hampshire, community mental health teams were the predominant way of providing health care services, with multidisciplinary staff being highly prevalent in most services. Moreover, in this area, day care services, mainly run by non-governmental organisations (NGOs) to support social functioning, seemed to play a significant role in providing non-direct health-related care.
Verona showed the highest percentage of services identified as not providing core health care, with nearly half of all mapped services being found in other care settings, including non-acute residential services with various levels of support, home care teams and day services in the community (Amaddeo et al., Reference Amaddeo, Barbui and Tansella2012).
Different patterns were found in Helsinki and Uusimaa, Loiret, Sør-Trøndelag and Suceava. Helsinki and Uusimaa reported the second highest bed rate in health services and highest in other care; residential services also represented the major area of other care provision here. The majority of beds were found in nursing homes with 24 h staffing providing permanent care for people with severe mental health problems. The remainder were mainly beds in nursing homes with less intensive daily support. These categories of beds have been rapidly increasing in Helsinki and Uusimaa and represent trans-institutionalisation (a shift from hospitals to other institutions), as well as private entrepreneurship (the majority of nursing homes are private for-profit companies under public contract and highly profitable) (Pedersen and Kolstad, Reference Pedersen and Kolstad2009). Such findings had important practical implications in Finland and led to changes in resource allocation (Gutierrez-Colosía et al., Reference Gutiérrez-Colosía, Salvador-Carulla, Salinas-Pérez, García-Alonso, Cid, Salazzari, Montagni, Tedeschi, Cetrano, Chevreul, Kalseth, Hagmair, Straßmayr, Park, Sfetcu, Ala-Nikkola, González-Caballero, Rabbi, Kalseth and Amaddeo2017).
The rate of beds in health care units in Loiret was quite high compared with other countries, and highest if only acute beds in hospital settings were considered. This is representative of the French system where hospital care still plays a significant role (Verdoux, Reference Verdoux2007). Interestingly, when looking at other care services in Loiret, not many services were targeted at people with mental health problems, as the majority of services were generic and could be used by anyone with no further specification. Finally, the high prevalence of nursing staff in other care services seems indicative of a rather health-orientated mental health system.
Sør-Trøndelag reported the highest bed rate in residential units providing health care, represented by both acute and non-acute hospital-based services. Half of the beds were in new mental health facilities providing specialist health care with a more community-oriented focus (District Psychiatric Centres) (Gutierrez-Colosía et al., Reference Gutiérrez-Colosía, Salvador-Carulla, Salinas-Pérez, García-Alonso, Cid, Salazzari, Montagni, Tedeschi, Cetrano, Chevreul, Kalseth, Hagmair, Straßmayr, Park, Sfetcu, Ala-Nikkola, González-Caballero, Rabbi, Kalseth and Amaddeo2017). This Norwegian area also had the highest staff rate in health care services. These two figures are indicative of a system with a high availability of community, residential and hospital services.
Suceava had a high number of beds both in health and other care services, mostly indefinite stay beds with daily support. This area also had the highest percentage of services with multidisciplinary staff. However, one possible explanation for these results is that these services consist mainly of large institutions where many categories of staff work. Also, in Romania there is no catchment area organisation and mental health services usually serve the whole country population (Junjan et al., Reference Junjan, Miclutia, Popescu, Ciumageanu, Sfetcu and Ghenea2009). The data adjusted for the study area population must therefore be interpreted as an approximation rather than a clear indicator of service use and availability. Future studies are needed to analyse balance of care patterns, including service availability and capacity in Eastern European countries, with a particular focus on the deinstitutionalisation process and mental health care reforms.
Typologies of services specific to certain areas were also found. For example, in Industrieviertel, Loiret, Sør-Trøndelag and Suceava, single-handed psychiatrists and psychologists were an important organisational component of the mental health system. In Sør-Trøndelag and Verona, municipalities and local authority social services played a substantial role in providing care to people with mental health problems.
We also identified some ‘grey zones’ that were more difficult to map and analyse. We are referring here to day care/rehabilitation activities and supported housing. For example, in Norway supported housing took the form of apartments rented by service users who then received mobile support from staff working for municipalities. Even though the apartments typically were co-located with personnel services that provide 24 h access to care, these were considered home-based services and not institutional/residential care and hence were coded as outpatient care and not as community residential care as in other areas where residential homes were managed by public agencies or NGOs.
Strengths and limitations
Our study involved the use of an internationally standardised instrument for service assessment, online training materials, a brief face-to-face training course and monitoring of data collection by the coordinating group. This study provides multi-country, multi-site analysis of patterns and balance of mental health care provision across Europe. This is a major advance over previous studies that compared services availability between areas in two countries such as Spain and Italy (Salvador-Carulla et al., Reference Salvador-Carulla, Tibaldi, Johnson, Scala, Romero and Munizza2005), Spain and Finland (Sadeniemi et al., Reference Sadeniemi, Almeda, Salinas-Pérez, Gutiérrez-Colosía, García-Alonso, Ala-Nikkola, Joffe, Pirkola, Wahlbeck, Cid and Salvador-Carulla2018), Spain and Chile (Salvador-Carulla et al., Reference Salvador-Carulla, Saldivia, Martinez-Leal, Vicente, Garcia-Alonso, Grandon and Haro2008), and Norway and Russia (Dahl et al., Reference Dahl, Rezvyy, Bogdanov and Øiesvold2017). This methodology can be used in future studies for longitudinal monitoring of service change within an area, for monitoring mental health reform in different world regions, as well as being applied to other areas of integrated care, such as for older people. However, the large number of researchers needed to collect data across the eight partner countries, variable levels of information available in different databases in these countries, as well as the practicality of the assessment tool and the complexity of assessment of mental health systems and integrated care may have led to data inconsistencies. The identification of the minimal units of care at every service required considerable time, effort and revision of the information gathered in each study area. A further limitation relates to missing information, particularly in ‘other care’ services. For example, a consistent proportion of services in the English study area had missing information on staff. Moreover, the differences found in services availability and characteristics among the study areas do not necessarily represent differences at the country level.
Furthermore, population-based figures should be interpreted with caution as in some countries, such as Austria and Romania, there are no health care catchment areas. Especially in densely populated areas with short travel distances, patients from outside the geographical study area may use a service in the study area, and, vice versa, patients from the selected study area may use services outside the area.
Another limitation lies in the terminology itself. The term ‘other care’ is broad and services have been reported here to a varying degree. The definition of ‘service’ and on how beds are reported may differ between countries. Differences may arise both related to how services are organised and funded and how they are reported in national statistics (Kalseth et al., Reference Kalseth and Magnussen2013). In order to overcome these terminological problems, we have produced an international glossary of terms for health systems research in health care (Montagni et al., Reference Montagni, Salvador-Carulla, McDaid, Straßmayr, Endel, Näätänen, Kalseth, Kalseth, Matosevic, Donisi, Chevreul, Prigent, Sfetcu, Pauna, Gutiérrez-Colosia, Amaddeo and Katschnig2017). Furthermore, data on availability and care capacity should be completed with information on financing, demand for and outcomes of services. These aspects have been analysed in other work packages of the REFINEMENT project (Kalseth et al., Reference Kalseth and Magnussen2013).
Finally, a fully bottom-up approach was missing in our study and not all areas surveyed included full mapping of all available services. In some instances, with hindsight, the only way to obtain information on the individual non-health care services would have been by contacting mental health advocacy groups and/or service user groups. Hence, for future studies, a triangulation of data, involving relevant stakeholder groups including service users and carers, is recommended.
Conclusion
Better coordination and integration of health and other care services are urgently needed in Europe (Valentijn et al., Reference Valentijn, Schepman, Opheij and Bruijnzeels2013). However, very little information is available on the overall availability and capacity of mental health provision. Developing harmonised mental health data across Europe is an essential step towards better mental health care (Wahlbeck, Reference Wahlbeck2011). This paper presents the first cross-national comparison of services for mental health care focusing on the balance between ‘core health care’ and ‘other care’. The distinction between health and other care provided in our study overcomes the traditional division between ‘health’ and ‘social’ services which is mainly based on service governance. Our paper offers an original taxonomy built on the DESDE-LTC instrument which enables classification of services according to core activities provided.
Acknowledgements
The members of the REFINEMENT Group: Florian Endel, Gisela Hagmair, Heinz Katschnig, Sonja Scheffel, Christa Straßmayr, Barbara Weibold (Austria); Tihana Matosevic, David McDaid, A-La Park (England); Taina Ala-Nikkola, Niklas Grönlund, Irja Hemmilä, Grigori Joffe, Jutta Järvelin, Raija Kontio, Maili Malin, Petri Näätänen, Sami Pirkola, Minna Sadeniemi, Eila Sailas, Marjut Vastamäki, Kristian Wahlbeck (Finland); Matthias Brunn, Karine Chevreul, Amélie Prigent (France); Francesco Amaddeo, Gaia Cetrano, Valeria Donisi, Laura Grigoletti, Ilaria Montagni, Laura Rabbi, Damiano Salazzari, Federico Tedeschi (Italy); Øyvind Hope, Jorid Kalseth, Brigitte Kalseth, Jon Magnussen (Norway); Juan M Cabases, Jordi Cid, Ana Fernandez, Andrea Gabilondo, Carlos García, Juan Luis González-Caballero, Mencía R. Gutiérrez-Colosía, Ana Fernandez, Alvaro Iruin, Esther Jorda, Cristina Molina, Emma Motrico, Jose Alberto Salinas, Luis Salvador-Carulla, Bibiana Prat, Carlos Pereira, Jose Juan Uriarte (Spain); Lucian Albu, Mugur Ciumageanu, Nona Chiriac, Dan Ghenea, Simona Musat, Cristian Oana, Raluca Sfetcu, Alexandru Paziuc, Carmen Pauna (Romania). Collaborators and observers from public health agencies: Institut d'Assistència Sanitària (Girona, Spain); Mental Health Plan, Department of Health (Catalonia, Spain); Mental Health Departments of Bizkaia and Gipuzkoa (Basque Country, Spain).
Availability of data and materials
Supplementary materials are available upon request and at: http://www.refinementproject.eu.
Financial support
The REFINEMENT project was funded by the European Commission under the Seventh Framework Programme within the Specific Programme ‘Cooperation’ – Theme ‘Health’: HEALTH.2010.3.2–1: Financing systems’ effect on quality of health care (Project number: 261 459, duration: January 2011 to December 2013).
Conflict of interest
None.
Ethical standards
Ethical approval was not required as the study did not include data on individual patients.










