Abstract
Aim:
To test the hypothesis that the tissue plasminogen activator (tPA) may counteract the inhibitory effect of plasminogen activator inhibitors (PAI) and attenuate lung injury in a rat model of ventilator-induced lung injury (VILI).
Methods:
Adult male Sprague-Dawley rats were ventilated with a HVZP (high-volume zero PEEP) protocol for 2 h at a tidal volume of 30 mL/kg, a respiratory rate of 25 breaths/min, and an inspired oxygen fraction of 21%. The rats were divided into 3 groups (n=7 for each): HVZP+tPA group receiving tPA (1.25 mg/kg, iv) 15 min before ventilation, HVZP group receiving HVZP+vehicle injection, and a control group receiving no ventilation. After 2 h of ventilation, the rats were killed; blood and lungs were collected for biochemical and histological analyses.
Results:
HVZP ventilation significantly increased total protein content and the concentration of macrophage inflammatory protein-2 (MIP-2) in the bronchoalveolar lavage fluid (BALF) as well as the lung injury score. Rats that received HVZP ventilation had significantly higher lung PAI-1 mRNA expression, plasma PAI-1 and plasma D-dimer levels than the control animals. tPA treatment significantly reduced the BALF total protein and the lung injury score as compared to the HVZP group. tPA treatment also significantly decreased the plasma D-dimer levels and the HVZP ventilation-induced lung vascular fibrin thrombi. tPA treatment showed no effect on MIP-2 level in BALF.
Conclusion:
These results demonstrate that VILI increases lung PAI-1 mRNA expression, plasma levels of PAI-1 and D-dimers, lung injury score and vascular fibrin deposition. tPA can attenuate VILI by decreasing capillary-alveolar protein leakage as well as local and systemic coagulation as shown by decreased lung vascular fibrin deposition and plasma D-dimers.
Similar content being viewed by others
Introduction
Mechanical ventilation is a life-saving treatment that has become the mainstay of management for patients with acute respiratory failure over the last several decades. However, there are several potential complications regardless of the life-saving potential of mechanical ventilation1. Ventilator-induced lung injury (VILI) can be caused by mechanical ventilation with a high tidal volume that damages the alveolar-capillary barrier and activates local and systemic inflammation2. The spectrum of VILI includes disruption of endothelial and epithelial cells, increases in endothelial and epithelial permeability, and alterations in pulmonary and systemic inflammatory mediators2,3,4.
Pulmonary fibrin turnover, the deposition of fibrin in the alveolar space, and increased procoagulant activity of bronchoalveolar lavage fluid (BALF) are the pathognomonic features of VILI5,6. Alveolar fibrin deposition may lead to surfactant dysfunction, poor gas exchange, decreased lung compliance, and increased ventilatory dependence7. Alveolar fibrin deposition is the net result of an imbalance of coagulation and fibrinolysis. Consequently, anticoagulant and fibrinolytic therapies in acute lung injury have recently been investigated with various compounds such as heparin and active site inactivated recombinant factor VIIa8,9,10. Anticoagulant therapy might be a useful tool in the treatment of VILI. The major mechanisms that contribute to increased alveolar fibrin turnover are increased local tissue factor-mediated thrombin generation and depressed urokinase plasminogen activator-mediated fibrinolysis, which is caused by an increase in plasminogen activator inhibitors (PAIs)11. PAI-1, a fibrinolytic antiprotease, is the major plasminogen inactivator in the plasma and the primary inhibitor of tissue plasminogen activator (tPA); therefore, it is responsible for decreased plasmin activity and fibrinolytic potential12,13. High pulmonary and systemic PAI-1 levels and increased alveolar fibrin deposition are features of animal models of VILI14. Increased plasma levels of PAI-1 are associated with adverse clinical outcomes and increased mortality in adults with acute lung injury15. tPA is responsible for fibrin degradation via the activation of plasminogen and has been used for thrombolysis in patients with acute myocardial infarction16. Aerosolized tPA improves pulmonary function in burn/smoke-induced lung injury in sheep17. tPA has both fibrinolytic and anti-inflammatory activity18. The distinctive combination of fibrinolytic and anti-inflammatory properties of tPA has made it an important natural anticoagulant. Theoretical considerations suggest that fibrinolytic therapy with tPA might benefit animals with VILI. We hypothesized that tPA may counteract the inhibitory effect of PAI-1, balance coagulation-fibrinolysis, and attenuate lung injury in an animal model of VILI. The aims of this study were to investigate the effects of tPA on gas exchange, lung cytokine and alveolar protein leakage, and local and systemic coagulation-fibrinolytic activity in a rat model of VILI and to find a potential treatment modality against high tidal volume-induced lung injury.
Materials and methods
Animals and protocol
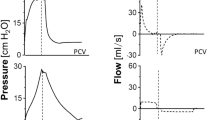
This study was approved by the Animal Care and Use Committee of Taipei Medical University and was performed with adult male Sprague-Dawley rats weighing 250–300 g. The rats were maintained on a 12-h light/dark cycle with free access to food and water. The rats were intraperitoneally anesthetized with pentobarbital (50 mg/kg, Abbott, North Chicago, IL, USA). Fifteen minutes before ventilation, the rats received tPA (1.25 mg/kg in 0.5 mL saline, Actilyse, Boehringer Ingelheim, Germany; n=7) or an equal volume of normal saline (vehicle; n=7) through a tail vein injection. The dosage of tPA was based on recommendations by Choi et al19. A polyethylene catheter (PE-50, Becton Dickinson, Sparks, MD, USA) containing isotonic saline was placed in one femoral artery to sample blood for gas analysis. A tracheostomy was performed, and a 14-gauge plastic cannula was inserted into the trachea. The animals were then ventilated with a high-volume zero positive end-expiratory pressure (PEEP) (HVZP) protocol by a volume-cycled ventilator (Small Animal Ventilator, Model SAR-830/AP; CWE, Ardmore, PA, USA) for 2 h at a tidal volume of 30 mL/kg, zero PEEP, a respiratory rate of 25 breaths/min, and an FiO2 of 0.21. The rats were selected at random to receive this ventilation strategy. Another group that received no ventilation served as the control (n=7). All animals were kept supine for the duration of the experiment, and arterial blood gases were measured with a blood gas analyzer (Model 1620, Instrumentation Laboratories, Lexington, MA, USA) at the beginning and every hour after randomization.
After 2 h of ventilation, the rats were killed with an intravenous injection of pentobarbital (100 mg/kg). Blood was collected from the femoral artery in citrated (0.109 mol/L) vacutainer tubes, placed on ice, and spun at 4 °C, and the resulting plasma was stored at -70 °C until analyzed. The chest was opened, and the lungs were removed intact from the animal with the tracheostomy tube in place. The right lung was ligated, and the left lung was lavaged with 2 mL of 0.9% saline at 4 °C that was washed in and out of the lungs three times and then recovered. This washing procedure was repeated two more times for each animal, with the three washes being pooled, and the total volume was recorded. There were no differences in the total volume of saline infused or recovered after the lavage procedure between the three experimental groups. The right superior lobe was fixed in 10% buffered formalin and embedded in paraffin. An aliquot of the BALF from each animal was used to measure the total protein content with bovine serum albumin as the standard. The value was expressed as mg/kg body weight.
Histology
Specimens were embedded in paraffin, stained with hematoxylin and eosin, and examined by a pathologist who was blinded to the protocol and experimental groups. Lung injury was scored according to the following items: 1) alveolar congestion, 2) hemorrhage, 3) infiltration of neutrophils into the airspace or the vessel wall, and 4) thickness of the alveolar wall14. Each item was graded according to a five-point scale: 0, minimal (little) damage; 1, mild damage; 2, moderate damage; 3, severe damage; and 4, maximal damage.
BALF macrophage inflammatory protein-2 (MIP-2) and plasma PAI-1 and D-dimer assays
BALF MIP-2 was tested by an enzyme-linked immunosorbent assay (ELISA) kit (R&D Systems, Minneapolis, MN, USA), and the value was expressed as pg/mL lavage fluid. Plasma PAI-1 was assayed by a commercially available ELISA kit (Innovative Research, Southfield, MI, USA). Fibrinolytic activity was assessed by measuring plasma concentrations of D-dimers with an ELISA kit purchased from American Diagnostica (Stamford, CT, USA).
Lung PAI-1 mRNA expression by real-time polymerase chain reaction (PCR)
The right middle lobe was ground into a powder in liquid nitrogen, and PAI-1 mRNA expression was measured using real-time PCR. Total RNA was extracted using TRIzol reagent (Invitrogen Life Technologies, Paisley, UK). Reverse transcription was performed on 1 μg of RNA with oligo-dT primers and the avian myeloblastosis virus reverse transcriptase (Roche, Indianapolis, IN, USA). The primer sequences for the SYBR green real-time PCR included the following: PAI-1 sense (5′-ATGGCTCAGAACAACAAGTTCAAC-3′) and antisense (5′-CAGTTCCAGGATGTCGTACTCG-3′), and GAPDH mRNA sense (5′-ATGATTCTACCCACGGCAAG-3′) and antisense (5′-CTGGAAGATGGTGATGGGTT-3′). Gene expression was quantitatively analyzed using the comparative CT (ΔCT) method, in which CT is the threshold cycle number (the minimum number of cycles needed before the product can be detected). The arithmetic formula for the ΔCT method is the difference in the number of threshold cycles for a target (PAI-1) and an endogenous reference (the GAPDH housekeeping gene). The amount of target normalized to an endogenous reference and relative to a calibration normalized to an endo-genous reference is given by 2ΔΔCT. The values of the control group were normalized to a value of one, and the values of other groups were normalized to the control group values. Four samples were analyzed for each gene in each group.
Immunohistochemistry of PAI-1 and fibrin
Immunohistochemical staining for PAI-1 and fibrin were performed on paraffin sections with immunoperoxidase visualization. After deparaffinization in xylene and rehydration in an alcohol series, the sections were first preincubated for 1 h at room temperature in 0.1 mol/L PBS containing 10% normal goat serum and 0.3% H2O2 to block endogenous peroxidase activity and nonspecific binding of the antibody before being incubated for 20 h at 4 °C with a rabbit polyclonal antibody against rat PAI-1 or a monoclonal antibody against human fibrin (1:50; American Diagnostica). The sections were then treated for 1 h at room temperature with biotinylated goat anti-rabbit immunoglobulin G (IgG; 1:200, Vector Laboratories, Burlingame, CA, USA). This process was followed by reaction with the reagents from an ABC kit (Avidin-Biotin Complex, Vector) per the manufacturer's recommendations, and the reaction products were visualized by 3,3′-diaminobenzidine and 0.003% H2O2 in 0.5 mol/L TRIS buffer (pH 7.6) before the sections were mounted on gelatin-coated slides using Permount (Fisher Scientific, Pittsburgh, PA, USA). The sections for PAI-1 were mounted in glycerin gelatin and counterstained with hematoxylin.
Quantification of PAI-1 immunoreactivity and fibrin thrombi
A minimum of four random lung fields of immunohistochemically stained sections per animal were captured with a digital camera and imported into the computerized image analysis system, Image-Pro Plus 5.1 for Windows. The automatic object counting and measuring process was used to quantify the immunoreactivity of the sections14. We used the “count/size” command to perform cell number counting operations for PAI-1. These operations generated a percentage of positively stained cells, and the value was expressed as a labeling index. The denominator of the labeling index was the number of cells in the field. The fixed lung was cut into 1-mm-thick horizontal slices, and two slices were systematically and uniformly sampled at random. Slices were sampled with a periodicity of two (eg, 1, 3 or 2, 4). Vascular fibrin thrombi per visual field were counted at a magnification of ×20.
Statistical analysis
The lung injury score data are given as the medians (range); other data are presented as the mean±SD. Statistically significant differences were analyzed by one-way ANOVA with a post-hoc Bonferroni test. The Mann-Whitney U test was used for the analysis of lung injury score. Differences were considered significant at P<0.05.
Results
Effects on gas exchange
The arterial blood gas tensions were comparable among the three study groups before mechanical ventilation (Table 1). Rats that received HVZP ventilation showed a higher mean pH and lower mean carbon dioxide tension than control animals, and tPA treatment exhibited no further effects on gas exchange.
Total protein, MIP-2, and PAI-1 in the BALF
The total protein contents recovered from the BALF were significantly higher in rats ventilated with the HVZP protocol than in the control group (Figure 1A). Treatment with tPA significantly reduced the HVZP ventilation-induced increase in the BALF protein content. The MIP-2 concentrations in the BALF increased after HVZP ventilation, and the values were approximately two-fold higher in the HVZP group compared to the control group (Figure 1B). The addition of tPA did not decrease MIP-2 levels. PAI-1 was undetectable in all BALF samples from control animals and barely detectable in HVZP and HVZP+tPA animals (data not shown).
Total protein and MIP-2 in BALF in the control, HVZP, and HVZP+tPA groups. All rats were randomly divided into three groups: the control group (n=7) did not receive ventilation; the HVZP group (n=7) received 2 h of ventilation at a tidal volume of 30 ml/kg, a respiratory rate of 25 breaths/min, and an FiO2 of 0.21; and the HVZP+tPA group (n=7) received an intravenous injection of tPA (1.25 mg/kg) 15 min before the HVZP ventilation. (A) Rats that received HVZP and HVZP+tPA ventilation had significantly higher bronchoalveolar lavage fluid (BALF) total protein contents than that of the control group (cP<0.01 vs control group). Compared to the HVZP group, the HVZP+tPA group had significantly lower BALF protein content (eP<0.05 vs HVZP group). (B) MIP-2 concentrations in BALF were significantly higher in rats of the HVZP and HVZP+tPA groups than in the control group (cP<0.01 vs control group).
Histology
After 2 h of ventilation, lung injury was characterized by alveolar congestion, hemorrhage, and inflammatory cell infiltration (Figure 2). The HVZP group showed patchy areas of hemorrhage and thickened alveolar walls, and the HVZP+tPA group showed less hemorrhage and alveolar congestion. No major histological abnormalities were present in the control animals. The HVZP group had a significantly higher lung injury score than did the control group (Table 2). Treatment with tPA significantly decreased the lung injury score compared to the HVZP group.
Lung PAI-1 mRNA expression, plasma PAI-1 levels, and immunohistochemistry of PAI-1
Rats that received HVZP and HVZP+tPA ventilation had significantly higher levels of lung PAI-1 mRNA expression and plasma PAI-1 than that of the control group (Figure 3). PAI-1 immunoreactivities were mainly detected in airway epithelial and mesenchymal cells, and the immunoreactivity significantly increased in the rats that received HVZP when compared with the control group. Treatment with tPA significantly reduced the HVZP ventilation-induced increase in PAI-1 immunoreactivity (Figure 4).
Lung PAI-1 mRNA expression and plasma PAI-1 levels in the control, HVZP, and HVZP+tPA groups. (A) Rats that received HVZP and HVZP+tPA ventilation had significantly higher levels of lung PAI-1 mRNA expression than that of the control group (cP<0.01 vs control group). (B) Compared to the control group, rats that received HVZP and HVZP+tPA ventilation had significantly higher plasma PAI-1 levels (cP<0.01 vs control group).
Immunohistochemical staining for PAI-1 in the (A) control, (B) HVZP, (C) HVZP+tPA groups (×100), and (D) quantitative analysis of PAI-1 immunoreactivity. Positive staining is shown as brown. PAI-1 immunoreactivities were mainly detected in airway epithelial and some mesenchymal cells, and the immunoreactivity markedly increased in rats that received HVZP ventilation when compared with the control group (cP<0.01 vs control group). Treatment with tPA significantly reduced the HVZP ventilation-induced increase in PAI-1 immunoreactivity (eP<0.05 vs HVZP group).
Plasma D-dimers
Rats that received HVZP ventilation exhibited significantly higher levels of plasma D-dimers than did the control animals (Figure 5). Treatment with tPA significantly reduced HVZP ventilation-induced increases in the plasma levels of D-dimers.
Lung vascular fibrin thrombi
After 2 h of ventilation, the HVZP+tPA group exhibited significantly lower numbers of fibrin thrombi per field than did the HVZP group (Figure 6). The HVZP group exhibited significantly higher numbers of vascular fibrin thrombi per lung field than the control group did.
Photomicrograph of fibrin thrombi in the (A) control, (B) HVZP, (C) HVZP+tPA groups (×200), and (D) the number of fibrin thrombi per lung field. Fibrin thrombi (arrow) were stained as brown. The HVZP group had a significantly higher number of fibrin thrombi per field than did the control and HVZP+tPA groups (cP<0.01, fP<0.01 vs control and HVZP+tPA groups).
Discussion
The spectrum of VILI includes the disruption of endothelial and epithelial cells, as well as increases in endothelial and epithelial permeability and pulmonary inflammatory mediators2,3,4. The outcomes of our in vivo lung injury model are consistent with alterations known to occur in VILI. The main findings of this study are that VILI is associated with increased lung PAI-1 mRNA expression, plasma levels of PAI-1 and D-dimer, lung injury score, PAI-1 immunoreactivity, and vascular fibrin deposition. Administration of tPA reduced plasma D-dimer levels, the lung injury score, PAI-1 immunoreactivity, and vascular fibrin deposition. These data indicate that high tidal volume ventilation may enhance local and systemic coagulation and suppress systemic fibrinolysis.
Deposition of fibrin in the alveolar space and increased procoagulant activity of the BALF are pathognomonic features of acute lung injury8,20. Studies of animal models of VILI showed that high tidal volume ventilation increases alveolar fibrin deposition and systemic PAI-1 activity while lung-protective mechanical ventilation decreases BALF levels of PAI-1, attenuates coagulation, and enhances fibrinolysis14,21. Although aerosol administration offers the theoretical advantage of the lungs receiving high concentrations of tPA, we chose intravenous administration because intra-alveolar and intravascular fibrin deposition and high systemic PAI-1 levels are frequently found in the setting of acute lung injury or VILI5,15. Intraperitoneal tPA lavage could also reduce intra-abdominal PAI-1 concentrations in experimental peritonitis20. The half-life of active tPA is very short, and the majority of the administered tPA forms complexes with PAI-122. tPA inhibits PAI-1 by forming these stable complexes and attenuates the expression of PAI-1 in lung tissue but not the production of plasma PAI-123. Plasma PAI-1 is synthesized from endothelial cells of the vessel wall and is quickly induced by high tidal volume ventilation14,23. We speculate that the reduction of plasma PAI levels by tPA administration is partially reversed by ongoing PAI production during VILI. This reversal may explain why the decreased plasma levels of PAI-1 after tPA administration compared with HVZP are not significant. In the animal model of VILI, we found tPA intervention reduced vascular fibrin deposition and decreased local PAI-1 expression. These results support our hypothesis that tPA treatment balances coagulation-fibrinolysis in the VILI animal model.
D-dimers are derived from the degradation of cross-linked fibrin polymers, which come from clots, not from free circulating fibrin or fibrinogen. Elevated levels of D-dimers indicate increases in blood coagulation and turnover of cross-linked intravascular fibrin activation24. In this rat model of VILI, we found that high tidal volume ventilation caused a substantial increase in lung vascular fibrin formation and plasma levels of D-dimers, and the administration of tPA reduced intravascular fibrin formation and decreased plasma levels of D-dimers. The decreasing effects of tPA therapy on plasma D-dimer levels have been reported with profibrinolytic drugs in animal and human studies25,26. Teke et al found that recombinant human activated protein C therapy significantly reduced plasma D-dimer levels in intestinal reperfusion-induced acute lung injury. Bernard et al also found significantly reduced plasma D-dimer levels in sepsis patients after administrating recombinant human activated protein C.
tPA is an endogenous serine protease with anti-inflammatory actions in addition to its fibrinolytic properties. MIP-2 is associated with leukocyte migration and activation and has been found to be closely associated with animal models of pneumonia and VILI27,28. In this study, although lung vascular fibrin deposition was significantly decreased, the BALF levels of MIP-2 were not decreased in the HVZP + tPA group. These changes imply that the fibrinolytic effect of tPA is independent of its anti-inflammatory activity. Although tPA influences neutrophil function in vitro, no data exists regarding the effect of exogenous tPA on MIP-2 levels in vivo27. In this study, we found that tPA treatment decreased HVZP ventilation-induced increases in plasma D-dimers but did not decrease BALF levels of MIP-2. These data on BALF MIP-2 are consistent with those of Stringer et al who demonstrated that tPA did not change interleukin-1-induced increases in lung myeloperoxidase activity and the dose of tPA required for anti-inflammatory activity was higher than that needed for fibrinolysis20,29. These results suggest that tPA attenuates high tidal volume-induced lung injury mostly through fibrinolytic effects rather than anti-inflammatory effects in this animal model.
In conclusion, this study shows that high tidal volume ventilation increased lung capillary-alveolar permeability and induced lung and systemic coagulation-fibrinolysis ab-normalities. Intravenous administration of tPA attenuates VILI by decreasing the protein leakage from plasma to alveoli and local and systemic coagulation, as indicated by decreasing lung vascular fibrin deposition and plasma D-dimers. tPA is not only a serine protease that converts plasminogen into biologically active plasmin but also a cytokine that activates intracellular signaling pathways and controls gene expression. Although tPA improves pulmonary function in burn/smoke-induced lung injury and attenuates VILI in this study, both the protease activity and the cytokine functions of tPA have been reported to play potential roles in the pathogenesis of renal fibrosis30. Therefore, more studies are needed to develop specific therapeutic agents that discretely target the fibrinolytic activity and avoid the fibrotic function of tPA in the treatment of VILI.
Author contribution
Chung-ming CHEN performed research, coordinated experiments, analyzed the data, wrote part of the paper, and drafted the manuscript; Leng-fang WANG performed animal and molecular experiments; Hsiu-chu CHOU performed histological experiments and was responsible for image analysis; Liang-ti HUANG performed part of the research and wrote the paper.
Abbreviations
BALF, bronchoalveolar lavage fluid; ELISA, enzyme-linked immunosorbent assay; MIP-2, macrophage inflammatory protein-2; PAI, plasminogen activator inhibitor; PCR, polymerase chain reaction; PEEP, positive end-expiratory pressure; tPA, tissue plasminogen activator; VILI, ventilator-induced lung injury.
References
Mutlu GM, Factor P . Complications of mechanical ventilation. Respir Care Clin N Am 2000; 6: 213–52.
Dos Santos CC, Slutsky AS . Invited review: mechanisms of ventilator-induced lung injury: a perspective. J Appl Physiol 2000; 89: 1645–55.
Jaecklin T, Otulakowski G, Kavenagh BP . Do soluble mediators cause ventilator-induced lung injury and multi-organ failure? Intensive Care Med 2010; 36: 750–7.
Peng XQ, Damarla M, Skirball J, Nonas S, Wang XY, Han EJ, et al. Protective role of PI3-kinase/Akt/eNOS signaling in mechanical stress through inhibition of p38 mitogen-activated protein kinase in mouse lung. Acta Pharmacol Sin 2010; 31: 175–83.
Dahlem P, Bos AP, Haitsma JJ, Schultz MJ, Meijers JC, Lachmann B . Alveolar fibrinolytic capacity suppressed by injurious mechanical ventilation. Intensive Care Med 2005; 31: 724–32.
Abraham E . Coagulation abnormalities in acute lung injury and sepsis. Am J Respir Cell Mol Biol 2000; 22: 401–4.
Idell S . Coagulation, fibrinolysis, and fibrin deposition in acute lung injury. Crit Care Med 2003; 31: S213–20.
Li LF, Huang CC, Lin HC, Tsai YH, Quinn DA, Liao SK . Unfractionated heparin and enoxaparin reduce high-stretch ventilation augmented lung injury: a prospective, controlled animal experiment. Crit Care 2009; 13: R108.
Dixon B, Schultz MJ, Hofstra JJ, Campbell DJ, Santamaria JD . Nebulized heparin reduces levels of pulmonary coagulation activation in acute lung injury. Crit Care 2010; 14: 445.
Vincent JL, Artigas A, Petersen LC, Meyer C . A multicenter, randomized, double-blind, placebo-controlled, dose-escalation trial assessing safety and efficacy of active site inactivated recombinant factor VIIa in subjects with acute lung injury or acute respiratory distress syndrome. Crit Care Med 2009; 37: 1874–80.
Choi G, Schultz MJ, Levi M, Van Der Poll T, Millo JL, Garrard CS . Protein C in pneumonia. Thorax 2005; 60: 705–6.
Urano T, Ihara H, Suzuki Y, Takada Y, Takada A . Coagulation-associated enhancement of fibrinolytic activity via a neutralization of PAI-1 activity. Semin Thromb Hemost 2000; 26: 39–42.
Cesarman-Maus G, Hajjar KA . Molecular mechanisms of fibrinolysis. Br J Haematol 2005; 3: 307–21.
Chen CM, Chou HC, Wang LF, Lang YD . Captopril decreases plasminogen activator inhibitor-1 in rats with ventilator-induced lung injury. Crit Care Med 2008; 36: 1880–5.
Prabhakaran P, Ware LB, White KE, Cross MT, Matthay MA, Olman MA . Elevated levels of plasminogen activator inhibitor-1 in pulmonary edema fluid are associated with mortality in acute lung injury. Am J Physiol 2003; 285: L20–8.
Sakamoto T, Ogawa H, Takazoe K, Yoshimura M, Shimomura H, Moriyama Y, et al. Effect of activated protein C on plasma plasminogen activator inhibitor activity in patients with acute myocardial infarction treated with alteplase: comparison with unfractionated heparin. J Am Coll Cardiol 2003; 42: 1389–94.
Enkhbaatar P, Murakami K, Cox R, Westphal M, Morita N, Brantley K, et al. Aerosolized tissue plasminogen inhibitor improves pulmonary function in sheep with burn and smoke inhalation. Shock 2004; 22: 70–5.
Stringer KA, Dunn JS, Gustafson DL . Administration of exogenous tissue plasminogen activator reduces oedema in mice lacking the tissue plasminogen activator gene. Clin Exp Pharmacol Physiol 2004; 31: 327–30.
Choi G, Hofstra JJ, Roelofs JJ, Florquin S, Bresser P, Levi M, et al. Recombinant human activated protein C inhibits local and systemic activation of coagulation without influencing inflammation during Pseudomonas aeruginosa pneumonia in rats. Crit Care Med 2007; 35: 1362–8.
Van Veen SQ, Meijers JCM, Levi M, Van Gulik TM, Boermeester MA . Effects of intra-abdominal administration of recombinant tissue plasminogen activator on coagulation, fibrinolysis and inflammatory responses in experimental polymicrobial peritonitis. Shock 2007; 27: 534–41.
Ware LB, Matthay MA, Parsons PE, Thompson BT, Januzzi JL, Eisner MD, et al. Pathogenetic and prognostic significance of altered coagulation and fibrinolysis in acute lung injury/acute respiratory distress syndrome. Crit Care Med 2007; 35: 1821–8.
Levin EG, Santell L, Osborn KG . The expression of endothelial tissue plasminogen activator in vivo: a function defined by vessel size and anatomic location. J Cell Sci 1997; 110: 139–48.
Binder B, Christ G, Gruber F, Grubic N, Hufnagl P . Plasminogen activator inhibitor 1: physiological and pathological roles. News Physiol Sci 2002; 17: 56–61.
Dahlbäck B, Villoutreix BO . Regulation of blood coagulation by the protein C anticoagulant pathway: Novel insights into structure-function relationships and molecular recognition. Arterioscler Thromb Vasc Biol 2005; 25: 1311–20.
Teke Z, Sacar M, Yenisey C, Atalay AO, Bicakci T, Erdem E . Activated protein C attenuates intestinal reperfusion-induced acute lung injury: an experimental study in a rat model. Am J Surg 2008; 195: 861–73.
Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, et al. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med 2001; 344: 699–709.
Jiang JS, Wang LF, Chou HC, Chen CM . Angiotensin-converting enzyme inhibitor captopril attenuates ventilator-induced lung injury in rats. J Appl Physiol 2007; 102: 2098–103.
Bonville CA, Bennett NJ, Koehnlein M, Haines DM, Ellis JA, DelVecchio AM, et al. Respiratory dysfunction and proinflammatory chemokines in the pneumonia virus of mice (PVM) model of viral bronchiolitis. Virology 2006; 349: 87–95.
Stringer KA, Hybertson BM, Cho OJ, Cohen Z, Repine JE . Tissue plasminogen activator (tPA) inhibits interleukin-1 induced acute lung leak. Free Radic Biol Med 1998; 25: 184–8.
Hu K, Mars WM, Liu Y . Novel actions of tissue-type plasminogen activator in chronic kidney disease. Front Biosci 2008; 13: 5174–86.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huang, Lt., Chou, Hc., Wang, Lf. et al. Tissue plasminogen activator attenuates ventilator-induced lung injury in rats. Acta Pharmacol Sin 33, 991–997 (2012). https://doi.org/10.1038/aps.2012.66
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2012.66
Keywords
This article is cited by
-
Risk factors and outcomes of diffuse alveolar haemorrhage after allogeneic haematopoietic stem cell transplantation
Bone Marrow Transplantation (2021)
-
COVID-19 as part of the hyperferritinemic syndromes: the role of iron depletion therapy
Immunologic Research (2020)
-
Deferoxamine preconditioning ameliorates mechanical ventilation-induced lung injury in rat model via ROS in alveolar macrophages: a randomized controlled study
BMC Anesthesiology (2018)