Abstract
Aurora kinase overexpression has been observed in patients with hematologic malignancies. MK-0457, a pan-aurora kinase inhibitor that also inhibits the ABL T315I mutant, was evaluated to treat patients with chronic myelogenous leukemia (CML) or Philadelphia chromosome (Ph+) acute lymphoblastic leukemia (ALL) with the T315I mutation. Adults with Ph+ chronic phase (CP)-, accelerated phase (AP)- or blast phase (BP)-CML, or ALL and documented BCR-ABL T315I mutation were treated with a 5-day continuous infusion of MK-0457 administered every 14 days at 40 mg/m2/h, 32 mg/m2/h or 24 mg/m2/h. Fifty-two patients (CP, n=15; AP, n=14; BP, n=11; Ph+ ALL, n=12) were treated. Overall, 8% of patients achieved major cytogenetic response; 6% achieved unconfirmed complete or partial response; 39% had no response. Two patients (CP CML) achieved complete hematologic response. No patients with advanced CML or Ph+ ALL achieved major hematologic response. The most common adverse event (AE) was neutropenia (50%). The most common grade 3/4 AEs were neutropenia (46%) and febrile neutropenia (35%). MK-0457 demonstrated minimal efficacy and only at higher, intolerable doses; lower doses were tolerated and no unexpected toxicities were observed. These data will assist in the development of future aurora kinase inhibitors and in the selection of appropriate target patient populations.
Similar content being viewed by others
Introduction
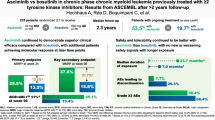
Significant progress has been made in the treatment of chronic myelogenous leukemia (CML); however, patients who progress from chronic phase (CP) CML to advanced disease respond poorly to therapy and have inadequate survival.1 Critical to the pathogenesis of CML and a subset of Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) is a chromosomal rearrangement that results in a fusion gene, BCR-ABL, which encodes an unregulated cytoplasm-targeted tyrosine kinase.2 Although first- and second-generation tyrosine kinase inhibitors—such as imatinib, dasatinib and nilotinib—have been used successfully to treat both CP and advanced CML, intolerance or resistance to these compounds presents a major challenge to treatment and the most common cause of treatment failure.3 For instance, median survival of patients with blast phase (BP) CML who are refractory or intolerant to imatinib is 3 to 9 months.4,5 Of particular concern is the ABL T315I ‘gatekeeper’ mutation, which renders leukemia cells resistant to all commercially available tyrosine kinase inhibitors other than ponatinib.3,6
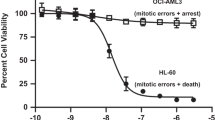
Aurora kinases (aurora-A, -B, -C) are serine/threonine protein kinases involved in the regulation of processes crucial for mitosis. Deregulation of aurora kinase activity promotes aberrant mitosis and chromosome instability. Overexpression of aurora kinases has been linked to tumorigenesis in a number of human cancers, including solid tumors and hematologic malignancies.7 A high proportion of patients with hematologic malignancies—including acute myelogenous leukemia (AML), Ph+ leukemias, aggressive non-Hodgkin lymphoma and Hodgkin lymphoma—overexpress aurora-A and -B; in some cases, overexpression has been linked to poorer outcomes.8
MK-0457 is a potent, small-molecule pan-aurora kinase inhibitor (binding affinity [Ki]=~0.6–18 nM) that disrupts mitotic progression and induces apoptosis. MK-0457 also inhibits the activity of other kinases, including FLT3 (Ki=~30 nM), JAK-2 (Ki=~190 nM) and both wild type (Ki ~30 nM) and T315I-mutated ABL (Ki ~42 nM).9, 10, 11 MK-0457 has been investigated for the treatment of both hematologic malignancies and solid tumors.4,11, 12, 13 The ability to inhibit multiple kinases, including the imatinib-resistant ABL T315I mutant, may be advantageous in the treatment of newly diagnosed and advanced disease.
In a phase 1/2 dose-escalation study in patients with refractory hematologic malignancies, treatment with MK-0457 was generally well tolerated.4 Forty-four percent of CML patients with the BCR-ABL T315I mutation achieved a response, and responses were reported as durable.4 The current phase 2 study was conducted to further evaluate MK-0457 in patients with CML or Ph+ ALL carrying the T315I mutation.
Materials and Methods
Study design and patient eligibility
This was a multicenter, open-label, nonrandomized, phase 2 study that evaluated the safety and efficacy of MK-0457 in patients with either CML or Ph+ ALL and confirmed BCR-ABL T315I mutation (ClinicalTrials.gov identifier: NCT00405054; http://clinicaltrials.gov/ct2/show/ NCT00405054; Protocol 008). Bone marrow aspirate and blood for molecular analysis were collected at screening and analyzed locally to detect the BCR-ABL T315I mutation. Bone marrow aspiration and/or biopsy was conducted before every other cycle for the first 3 months and then every 3 months, at the time of discontinuation and every 3 months during follow-up, and/or as clinically indicated or to confirm a response. Locally available assays were used for detection of the T315I mutation (examples included direct sequencing, fluorescence resonance energy transfer hybridization probe detection and denaturing high performance liquid chromatography).
Patients 18 years of age or older with Ph+ (or BCR-ABL+) CP CML, BP CML, accelerated phase (AP) CML or ALL were eligible. The Eastern Cooperative Oncology Group (ECOG) performance status had to be 2 or lower for CP CML patients and 3 or lower for all other patients. There were no restrictions on the number of prior therapies; however, administration of cytotoxic agents was not permitted within 2 weeks prior to study drug treatment, and a period of at least five half-lives was required for non-cytotoxic anti-leukemic agents. Hydroxyurea was permitted through the first treatment cycle to control peripheral blood leukemic cell counts. Patients must have had adequate liver and renal function (with the exception of Gilbert’s syndrome affecting total bilirubin) and were excluded if they had uncontrolled symptomatic congestive heart failure, angina or a myocardial infarction in the preceding 3 months; active infections including HIV, HBV and HCV; severe concurrent disease; or an active second malignancy, or if they had undergone an allogeneic bone marrow transplant within 3 months of starting the trial or had active uncontrolled graft-versus-host disease. Patients with known hypersensitivity to components of the study drug or analogs, or who were pregnant or breastfeeding, were also excluded. The study was conducted in accordance with the principles of the Declaration of Helsinki and followed Good Clinical Practice guidelines. All documents were reviewed and approved by the individual institution review boards and all patients provided written informed consent prior to trial enrollment.
Treatment plan and assessments
Patients were treated using a 5-day continuous intravenous infusion of MK-0457 administered every 14 days, which constituted one cycle of treatment. The maximum tolerated dose was initially identified as 40 mg/m2/h for the 5-day dosing schedule of MK-0457. The protocol was subsequently amended to include a lower starting dose of MK-0457 (32 mg/m2/h) because of significant toxicity at 40 mg/m2/h. Additional patients were enrolled at a lower dose of 24 mg/m2/h, with further dose reductions permitted in patients for toxicity. Patients who were candidates for bone marrow transplant were permitted to leave the study for transplantation. Those patients who achieved a hematologic response prior to bone marrow transplantation were followed for disease outcomes. Patients were allowed to receive additional treatment cycles as long as they did not display clinically significant disease progression and continued to tolerate the study drug. Primary efficacy end points were major cytogenetic response (MCyR) for patients with CP CML and major hematologic response for patients with AP CML, BP CML and Ph+ ALL.14 Key secondary efficacy end points were complete hematologic response in patients with CP CML and best cytogenetic response in patients with AP CML, BP CML and Ph+ ALL. Hematologic and cytogenetic responses were evaluated throughout the study from peripheral blood, bone marrow and lumbar puncture (for patients who were central nervous system positive). Hematologic response was required to be maintained for at least 28 days to be classified as a response. All patients were assessed for safety, which included physical examination, vital signs, chest X-rays, ECOG performance status, laboratory assessments and monitoring of adverse events (AEs). Adverse events were graded according to the United States National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE) version 3.0. Each of the four populations was considered an independent substudy. A Simon two-stage minimax design was used with a one-sided type 1 error of 0.025 and type 2 error of 0.10 using early stopping rules to terminate the substudy if the primary end point was unlikely to be met. A more conservative stopping rule was employed for the CP, BP and AP CML populations if none of the first 22 patients responded to treatment. The rate of response (MCyR for CP CML; major hematologic response for AP CML, BP CML and Ph+ ALL) in each population to declare the substudy positive with 90% power was 30% in BP, 30% in Ph+ ALL, 45% in AP and 35% in CP.
Results
Patient characteristics and disposition
Between December 2006 and May 2008, 52 patients with T315I-positive CML or Ph+ ALL were enrolled and received at least one dose of study drug (Table 1). Recruitment was halted prior to completion of the planned accrual target of 228 patients because of sponsor decision to discontinue the program due to change in priorities. Enrolled patients included 15 with CP CML, 14 with AP CML, 12 with Ph+ ALL and 11 with BP CML. The overall median age was 52 years (range 22–78) and the majority of patients (92%) had an ECOG performance status of 0 to 2. Fifty-four percent of patients had received at least four prior therapies and 29% had received one to three prior therapies, although therapies received may have been part of the same regimen. Seventeen percent were previously untreated. Twenty-six patients started treatment at 40 mg/m2/h, 11 at 32 mg/m2/h and 15 at 24 mg/m2/h. Eighteen patients (35%) discontinued treatment due to progressive disease, representing half of all patients who discontinued the study. Ten patients (19%) discontinued due to AEs. Other reasons for discontinuation included bone marrow transplant (6%), physician decision (6%) and patient consent withdrawn (6%).
Efficacy
Cytogenetic response was not measureable for almost half (48%) of all patients due to lack of a post-baseline assessment. For evaluable patients, 8% of patients (n=4) achieved a confirmed MCyR, 6% (n=3) achieved an unconfirmed complete cytogenetic response (CCyR) or partial cytogenetic response (PCyR) and 39% had no response (Table 2). Two patients with CP CML (13% of CP patients) experienced a MCyR: one with CCyR and one with PCyR (Table 2). Both patients were in the 40-mg/m2/h treatment group; however, both required significant dose reductions throughout the course of the study. Dose reduction for the patient who achieved a CCyR occurred each cycle until dose stabilization at 16 mg/m2/h at cycle 6. The patient with a PCyR had a dose reduction to 32 mg/m2/h at cycle 2 followed by another dose reduction at cycle 6 to 28 mg/m2/h. Two of 25 patients (8%) with advanced CML achieved a MCyR, one with AP CML achieved a CCyR and one with BP CML achieved a PCyR. Three patients with AP CML or Ph+ ALL (6% of all patients), all in the 40-mg/m2/h treatment group, achieved an unconfirmed CCyR or PCyR. Two of 15 patients (13%) with CP CML achieved a complete hematologic response. Both were in the 40-mg/m2/h treatment group and none of the other patients, including those in lower treatment groups, had confirmed hematologic assessments of response post baseline. None of the 37 patients with AP CML or Ph+ ALL achieved a major hematologic response while in the study. Four patients with AP CML achieved a minor response: three patients in the 40-mg/m2/h treatment group and one in the 32-mg/m2/h treatment group. One patient with Ph+ ALL achieved unconfirmed no evidence of leukemia (24 mg/m2/h) and one patient achieved a minor response (40 mg/m2/h). None of the 11 patients with BP CML achieved any major or minor response.
Safety and tolerability
Overall, 94% of patients had at least one AE; all patients in the 40 mg/m2/h and 32 mg/m2/h treatment groups and 80% of patients in the 24 mg/m2/h group experienced at least one AE (Table 3). Generally, the rate and intensity of AEs were dose dependent (Table 3). The most common AEs were related to blood and lymphatic system disorders (69%) and gastrointestinal disorders (60%). Treatment-emergent AEs included neutropenia (50%), anemia (37%), febrile neutropenia (35%), diarrhea (35%), thrombocytopenia (29%) and nausea (23%; Table 3). Although gastrointestinal disorders were experienced by a high number of patients, most were grade 1 or 2. The most common grade 3 or 4 AEs were neutropenia (46%), febrile neutropenia (35%), thrombocytopenia (29%) and anemia (21%; Table 3). Twenty-one patients (40%) experienced an infection and/or infestation during the study, with the highest rate of infection occurring in the 40-mg/m2/h treatment group (58%), followed by 27% and 20% of patients for the 32-mg/m2/h and 24-mg/m2/h treatment groups, respectively. Two grade 4 infections were observed: one patient in the 40-mg/m2/h treatment group experienced septic shock and one patient in the 32-mg/m2/h treatment group developed cellulitis. One patient in the 40-mg/m2/h treatment group died of Klebsiella infection.
Serious AEs were reported in 65% of patients. The highest rates of serious AEs were observed in the 40-mg/m2/h and 32-mg/m2/h treatment groups (73% and 64%, respectively), and 20% of patients experienced serious AEs in the 24-mg/m2/h group. Serious AEs that occurred in at least two patients included neutropenia (27%), febrile neutropenia (21%), pneumonia (6%), thrombocytopenia (6%), stomatitis (6%), peau d’orange (4%), electrocardiogram QT prolonged (4%) and pyrexia (4%).
Seven patients (14%) died during the study. Causes of death included progressive CML, cardiac failure, cerebral hemorrhage, neutropenia, acute pulmonary edema, Klebsiella infection and ‘somnolence’. Four patients in the 40-mg/m2/h treatment group died, one patient in the 32-mg/m2/h treatment group died and two patients in the 24-mg/m2/h treatment group died. Deaths due to cardiac failure, cerebral hemorrhage and neutropenia were reported by the investigator as drug related. More than 60% of patients starting at the 40-mg/m2/h dose required at least one dose reduction, compared with 7% of patients starting treatment at the 24-mg/m2/h dose. At the time when the study was discontinued, patients had received a median of two treatment cycles (range 1–14; mean 3.04 cycles). One patient, deemed by the investigator to be deriving clinical benefit with MK-0457, was permitted to continue receiving treatment after the study was discontinued and received a total of 25 cycles of treatment.
Discussion
Aurora kinases are critical regulators of mitosis and have been implicated in cancer progression.11 Inhibition of aurora kinases has therefore been pursued for the development of anticancer agents.11 MK-0457 is a potent inhibitor of aurora kinases with cross-reactivity to other kinases such as FLT3 and ABL. Leukemia patients carrying the ABL T315I mutation are often resistant to all available tyrosine kinase inhibitors, presenting the clinical challenge of finding effective treatment options. These patients tend to have a poor prognosis, highlighting the need to develop new therapies to overcome this resistance.6 Recent results from phase 1 and 2 trials evaluating the pan-BCR-ABL inhibitor ponatinib and the protein synthesis inhibitor omacetaxine have demonstrated efficacy in these poor-prognosis patients.15,16 The number of patients who achieved cytogenetic response in a phase 2 trial of ponatinib was high; the subgroup of patients carrying the T315I mutation had higher response rates than those without,17 but cardiovascular and thrombotic AE limit the clinical appeal of this agent.
In this phase 2 study in patients with ABL T315I-mutated leukemia, cytogenetic responses were observed in 14% of patients (8% confirmed, 6% unconfirmed) with chronic and advanced-stage CML or Ph+ ALL. A significant number of patients were not evaluable for cytogenetic (48% of patients) or hematologic (25% of patients) responses; no responses were observed in 39% of patients and 60% of patients, respectively. Bone marrow biopsies were collected every other cycle to assess cytogenetic response and the likelihood of a patient discontinuing (due to toxicity, for example) prior to an assessment was high. The fact that a high percentage of patients were un-evaluable for response, may potentially explain the discrepancy with the positive responses reported in the phase 1/2 dose-escalation study in patients with refractory hematologic malignancies.4 Many of the patients entered the current study heavily pretreated and with advanced disease. In general, MK-0457 was tolerated at lower doses and no unexpected toxicities were observed in this patient population. Higher doses were associated with an increase in the incidence and severity of adverse events.
Preliminary results from a phase 1 study in patients with solid tumors, presented after initiation of the current study, showed that infusion of 10 mg/m2/h MK-0457 over 5 days in a 28-day cycle was the maximum tolerated dose.18 Neutropenia was the most common AE, consistent with previously published reports, and likely due to aurora kinase inhibition on rapidly proliferating non-cancer cells.4,11,13,19 Additional hematologic and gastrointestinal disorders were also observed and overlap with the AE profile reported in other studies. Although gastrointestinal disorders were common, they were primarily grade 1 and 2. Gut epithelium contain rapidly cycling cells, potentially leading to the gastrointestinal events observed.4,11,13,19 In another phase 1 dose-escalation study in patients with advanced solid tumors, MK-0457 was administered as a 24-hour continuous intravenous infusion and was generally well tolerated in this heavily pretreated patient population. The maximum tolerated dose was 64 mg/m2/h. Stable disease was achieved for almost half of the 27 patients.19
A number of aurora kinase inhibitors currently in development for the treatment of hematologic malignancies have also demonstrated inhibitory activity (half maximal inhibitory concentration values ranging from 4 to 81 nmol/l) in patients with the ABL T315I mutation, including ENMD-2076 and AT9283.8 Preclinical studies using cancer cells have demonstrated that aurora kinase inhibitors may provide benefit as part of combination therapy or in select patient populations. Cancer cells depleted of aurora-A were sensitized to the effect of chemotherapeutic agents, including taxanes, cisplatin, docetaxel and ionizing radiation.20, 21, 22, 23 Multiple cancer cell lines with defective p53-p21 pathways were more sensitive to the effects of MK-0457 than cells with wild-type p53-p21 pathways.24 Although clinical development of MK-0457 has ceased, results from this and other studies that have evaluated the effects of aurora kinase inhibitors may help to guide selection and development of future anticancer agents, in combination or in select patient populations, and their use as potential chemosensitizers may be explored further.
References
Cooper S, Giles FJ, Savona MR . Overcoming resistance in chronic myelogenous leukemia. Leuk Lymphoma 2009; 50: 1785–1793.
Rowley JD . Letter: A new consistent chromosomal abnormality in chronic myelogenous leukaemia identified by quinacrine fluorescence and Giemsa staining. Nature 1973; 243: 290–293.
Fava C, Rege-Cambrin G, Saglio G . Chronic myeloid leukemia: state of the art in 2012. Curr Oncol Rep 2012; 14: 379–386.
Giles FJ, Swords RT, Nagler A, Hochhaus A, Ottmann OG, Rizzieri DA et al. MK-0457, an Aurora kinase and BCR-ABL inhibitor, is active in patients with BCR-ABL T315I leukemia. Leukemia 2013; 27: 113–117.
Hochhaus A . Imatinib mesylate (Glivec, Gleevec) in the treatment of chronic myelogenous leukemia (CML) and gastrointestinal stromal tumors (GIST). Ann Hematol 2004; 83 (Suppl 1): S65–S66.
Branford S, Rudzki Z, Walsh S, Parkinson I, Grigg A, Szer J et al. Detection of BCR-ABL mutations in patients with CML treated with imatinib is virtually always accompanied by clinical resistance, and mutations in the ATP phosphate-binding loop (P-loop) are associated with a poor prognosis. Blood 2003; 102: 276–283.
Li JJ, Li SA . Mitotic kinases: the key to duplication, segregation, and cytokinesis errors, chromosomal instability, and oncogenesis. Pharmacol Ther 2006; 111: 974–984.
Farag SS . The potential role of Aurora kinase inhibitors in haematological malignancies. Br J Haematol 2011; 155: 561–579.
Carter TA, Wodicka LM, Shah NP, Velasco AM, Fabian MA, Treiber DK et al. Inhibition of drug-resistant mutants of ABL, KIT, and EGF receptor kinases. Proc Natl Acad Sci USA 2005; 102: 11011–11016.
Cheetham GM, Charlton PA, Golec JM, Pollard JR . Structural basis for potent inhibition of the Aurora kinases and a T315I multi-drug resistant mutant form of Abl kinase by VX-680. Cancer Lett 2007; 251: 323–329.
Pollard JR, Mortimore M . Discovery and development of aurora kinase inhibitors as anticancer agents. J Med Chem 2009; 52: 2629–2651.
Giles FJ, Cortes J, Jones D, Bergstrom D, Kantarjian H, Freedman SJ . MK-0457 a novel kinase inhibitor, is active in patients with chronic myeloid leukemia or acute lymphocytic leukemia with the T315I BCR-ABL mutation. Blood 2007; 109: 500–502.
Harrington EA, Bebbington D, Moore J, Rasmussen RK, Ajose-Adeogun AO, Nakayama T et al. VX-680, a potent and selective small-molecule inhibitor of the Aurora kinases, suppresses tumor growth in vivo. Nat Med 2004; 10: 262–267.
Baccarani M, Cortes J, Pane F, Niederwieser D, Saglio G, Apperley J et al. Chronic myeloid leukemia: an update of concepts and management recommendations of European LeukemiaNet. J Clin Oncol 2009; 27: 6041–6051.
Cortes J, Lipton JH, Rea D, Digumarti R, Chuah C, Nanda N et al. Phase 2 study of subcutaneous omacetaxine mepesuccinate after TKI failure in patients with chronic-phase CML with T315I mutation. Blood 2012; 120: 2573–2580.
Cortes JE, Kantarjian H, Shah NP, Bixby D, Mauro MJ, Flinn I et al. Ponatinib in refractory Philadelphia chromosome-positive leukemias. N Engl J Med 2012; 367: 2075–2088.
Cortes JE, Kim DW, Pinilla-Ibarz J, le Coutre P, Paquette R, Chuah C et al. A phase 2 trial of ponatinib in Philadelphia chromosome-positive leukemias. N Engl J Med 2013; 369: 1783–1796.
Rubin EH, Shapiro GI, Stein MN, Watson P, Begstrom D, Xiao A et al. A phase I clinical and pharmacokinetic (PK) trial of the aurora kinase (AK) inhibitor MK-0457 in cancer patients. J Clin Oncol 2006; 24 (Suppl): 18s (Abstr 3009).
Traynor AM, Hewitt M, Liu G, Flaherty KT, Clark J, Freedman SJ et al. Phase I dose escalation study of MK-0457, a novel Aurora kinase inhibitor, in adult patients with advanced solid tumors. Cancer Chemother Pharmacol 2011; 67: 305–314.
Briassouli P, Chan F, Savage K, Reis-Filho JS, Linardopoulos S . Aurora-A regulation of nuclear factor-kappaB signaling by phosphorylation of IkappaBalpha. Cancer Res 2007; 67: 1689–1695.
Hata T, Furukawa T, Sunamura M, Egawa S, Motoi F, Ohmura N et al. RNA interference targeting aurora kinase a suppresses tumor growth and enhances the taxane chemosensitivity in human pancreatic cancer cells. Cancer Res 2005; 65: 2899–2905.
Sehdev V, Katsha A, Ecsedy J, Zaika A, Belkhiri A, El-Rifai W . The combination of alisertib, an investigational Aurora kinase A inhibitor, and docetaxel promotes cell death and reduces tumor growth in preclinical cell models of upper gastrointestinal adenocarcinomas. Cancer 2013; 119: 904–914.
Tao Y, Zhang P, Frascogna V, Lecluse Y, Auperin A, Bourhis J et al. Enhancement of radiation response by inhibition of Aurora-A kinase using siRNA or a selective Aurora kinase inhibitor PHA680632 in p53-deficient cancer cells. Br J Cancer 2007; 97: 1664–1672.
Gizatullin F, Yao Y, Kung V, Harding MW, Loda M, Shapiro GI . The Aurora kinase inhibitor VX-680 induces endoreduplication and apoptosis preferentially in cells with compromised p53-dependent postmitotic checkpoint function. Cancer Res 2006; 66: 7668–7677.
Acknowledgements
This study was sponsored by Merck & Co., Inc., Whitehouse Station, NJ, USA. Writing and editorial assistance was provided by Jennifer Granit, PhD, Integrus Scientific, and was funded by Merck & Co., Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
ER and PW are employees of and may own stock in Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Whitehouse Station, NJ, USA. FJG received a grant from Merck for this study. TH received grants from Novartis, BMS and ARIAD outside the submitted work. JLJ received a grant from Merck outside the submitted work. JCortes received grants and consulting fees from ARIAD, BMS, Novartis, Pfizer and Teva outside the submitted work. JClark is an employee of Incyte Corporation. GM received personal fees from Novartis, Roche, BMS and Pfizer outside the submitted work. DWK received a grant from Novartis during this study, honoraria from Novartis, BMS and ILYANG, and a grant from Pfizer outside the submitted work. JFS, AN, PR, F-XM, ID, AH and CP have no conflict of interest to disclose.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Seymour, J., Kim, D., Rubin, E. et al. A phase 2 study of MK-0457 in patients with BCR-ABL T315I mutant chronic myelogenous leukemia and philadelphia chromosome-positive acute lymphoblastic leukemia. Blood Cancer Journal 4, e238 (2014). https://doi.org/10.1038/bcj.2014.60
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bcj.2014.60
This article is cited by
-
Differential ABC transporter expression during hematopoiesis contributes to neutrophil-biased toxicity of Aurora kinase inhibitors
Nature Communications (2022)
-
Targeting AURKA in Cancer: molecular mechanisms and opportunities for Cancer therapy
Molecular Cancer (2021)
-
Third-line therapy for chronic myeloid leukemia: current status and future directions
Journal of Hematology & Oncology (2021)
-
Alternative approaches to target Myc for cancer treatment
Signal Transduction and Targeted Therapy (2021)
-
Aurora kinase A, a synthetic lethal target for precision cancer medicine
Experimental & Molecular Medicine (2021)