Abstract
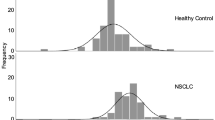
In this study we compared the diagnostic utility of: (1) neuron-specific enolase (NSE); (2) squamous cell carcinoma antigen (SCC); (3) carcinoembryonic antigen (CEA); and (4) cytokeratin markers (CYFRA 21-1, TPA, TPM, TPS) in patients with small-cell lung cancer (SCLC) (21 cases) and non-small-cell lung cancer (94 cases). For comparison we also studied 66 patients with benign lung diseases and nine with pleural mesothelioma. NSE levels in SCLC patients were significantly higher than those in all the other groups studied. No significant variations were found among the SCC levels in all groups. CEA levels in patients with adenocarcinoma were significantly higher than those in all other groups studied. CYFRA 21-1 serum levels significantly increased in patients with squamous cell carcinoma and mesothelioma, while TPA, TPS and TPM increased in patients with lung cancer irrespective of the histological type. In patients with SCLC, high levels of all markers except SCC were found when the disease was extensive. In patients with non-SCLC, the highest levels of all tumour markers were usually found in those with advanced disease, although CYFRA 21-1 gave a sensitivity of 44% when a specificity of 95% was fixed in stage I non-SCLC patients. An analysis of receiver operating characteristic curves revealed that the highest diagnostic accuracies in distinguishing benign from malignant lung diseases were achieved with TPM (81%), CYFRA 21-1 (72%), CEA (78%) or TPA (78%) when using cut-off values of 46 Ul-1, 3.0 micrograms l-1, 2.0 micrograms l-1 and 75 Ul-1 respectively. When all patients were considered, the combined evaluation of more than one marker did not significantly improve the results obtained with TPM alone. However, taking into consideration the fact that CYFRA 21-1 is the most sensitive index of early lung tumours and that its combined determination with TPM did not worsen the overall sensitivity and specificity of the latter, the combined use of these two markers may be suggested as a useful took for the diagnosis of lung tumours.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Plebani, M., Basso, D., Navaglia, F. et al. Clinical evaluation of seven tumour markers in lung cancer diagnosis: can any combination improve the results?. Br J Cancer 72, 170–173 (1995). https://doi.org/10.1038/bjc.1995.296
Issue Date:
DOI: https://doi.org/10.1038/bjc.1995.296