Abstract
Background:
Non-compliance with oral treatment in oncology is an emerging health issue. For breast cancer (BC) patients, few data are available on compliance and persistence to tamoxifen in younger women and to aromatase inhibitors (AIs) as compared with tamoxifen in older women.
Methods:
We constituted a cohort of 13 479 women with BC who received at least one prescription of tamoxifen or AI between 1998 and 2008, in the United Kingdom General Practice Research Database. Days covered by medication and treatment discontinuation were studied. Time to treatment discontinuation was calculated using Kaplan–Meier estimates.
Results:
Overall, 18.9% (95% CI: 15.1–23.0) of women on AIs as compared with 31.0% (95% CI: 29.6–32.2) of women on tamoxifen had discontinued their treatments within the first 5 years (P<0.001). This rate raised to 50.7% (95% CI: 43.0–57.9) among the 416 women under 40 years receiving tamoxifen as initial hormonal therapy. Among older women, treatment discontinuation was less frequent for AIs as compared with tamoxifen (P<0.001). Among women on AI therapy, 14% of them (n=374) had switched treatments.
Conclusion:
Among older women, the real-life patterns of use of AI show high rates of compliance. In younger women, tamoxifen is prematurely discontinued for half of patients.
Similar content being viewed by others
Main
In the field of oncology, the use of oral therapy is increasing and treatment compliance issues are of growing interest (Partridge et al, 2002; Ruddy et al, 2009). Oral adjuvant hormonal therapy in hormonal-responsive early breast cancer (BC) reduces the risk of recurrence and increases survival rates (Early Breast Cancer Trialists’ Collaborative Group (EBCTCG), 2005). For the last 20 years, a 5-year tamoxifen treatment was the standard therapy for all women diagnosed with hormone-sensitive BC. More recently, aromatase inhibitors (AIs) were shown to further reduce the risk of recurrence or death from BC as compared with tamoxifen in post-menopausal women (Crivellari et al, 2008; Forbes et al, 2008) and constitute an alternative option now recommended for the adjuvant treatment of early BC (National Institute for Health and Clinical Excellence, 2006; Goldhirsch et al, 2009; Burstein et al, 2010).
Non-compliance and early discontinuation of hormonal treatments are likely to affect treatment efficacy in BC patients (Early Breast Cancer Trialists’ Collaborative Group (EBCTCG), 2005; McCowan et al, 2008; Dezentje et al, 2009). In previously published observational studies, depending on the methodology used, discontinuation rates for tamoxifen ranged from 17% at 2 years to 49% at 5 years (Demissie et al, 2001; Partridge et al, 2003; Fink et al, 2004; Lash et al, 2006; Barron et al, 2007; Kahn et al, 2007; Owusu et al, 2008; Ziller et al, 2009; Hershman et al, 2010) and from 21 to 51% at a 3-year maximal follow-up for AIs (Partridge et al, 2008; Ziller et al, 2009; Hershman et al, 2010). Comparison of non-persistence between tamoxifen and AIs is difficult as the majority of past studies have often used different methodologies rendering external comparison inappropriate.
Tamoxifen and AIs present different side-effect profiles that may in turn affect the patient's compliance with the treatment differently outside controlled clinical trials. Specific functional side effects of AIs such as arthralgia, observed in routine check-ups, are likely to further reduce compliance. The superiority of the efficacy of AIs over tamoxifen observed in clinical trials, where compliance is likely to be optimal (Osterberg and Blaschke, 2005), may be diminished in real life owing to differential non-compliance rates. Studying further the difference in compliance between tamoxifen and AIs is therefore crucial.
Few data are available on compliance with and persistence to tamoxifen in younger women. Indeed, most studies focused on older women and excluded premenopausal women. Only four studies included women with a large age range (Partridge et al, 2003; Barron et al, 2007; Kahn et al, 2007; Hershman et al, 2010). These four studies found younger age to be associated with lower compliance or higher discontinuation rates. However, they did not provide detailed data for this age group and relied on self-reports of compliance or on databases covering specific subsamples of the general population. Therefore to date, no study on younger women has provided detailed data on tamoxifen use in a population-based setting.
Our objective was therefore to study patterns of use of tamoxifen and AIs in an observational population-based cohort of women with BC. We secondly focused on two specific aspects: first, tamoxifen use in younger women with BC; second, AI use as compared with tamoxifen use in older women.
Methods
Source of data
The United Kingdom (UK) General Practice Research Database (GPRD) constituted the primary source of data. It comprises data on over 4.4 million currently active individuals (approximately 7% of the English population) collected prospectively from 1987 to present. Data collected to date comprise over 55 million person years of research quality data. As the UK National Health Service provides universal coverage, the database is population based, all segments of the population being represented. The medical practices participating in the GPRD show a geographic distribution representative of the UK population. Age and sex distributions of patients in the GPRD reflect those reported by the National Population Census (Garcia Rodriguez et al, 2002).
In the UK, GPs are the primary care givers for all patients in the National Health Service and therefore all consultants are required to inform the referring GP on clinical events and medical diagnoses whenever a patient is seen in hospital or by an outpatient specialist.
The database records a large amount of medical information including comprehensive records of prescriptions written, all clinically medical diagnoses both in-patient and outpatient, and referrals to hospitals. Prescriptions supplied by GPRD physicians are automatically recorded in the database. The recorded information on drug exposures and diagnoses has been validated (Lawrenson et al, 1999, 2000; Jick et al, 2003). More specifically, the GPRD has been shown to provide BC incidence closely similar to the national registration data (Kaye et al, 2000).
The study protocol was approved by the Scientific and Ethical Advisory Group of the GPRD.
Study population
Cohort definition.
We constituted a cohort of women diagnosed with BC and who received at least one prescription of tamoxifen, anastrozole, letrozole, or exemestane between 1 January 1998 and 30 June 2008. Breast cancer was identified using a code for breast surgery combined with a diagnostic code of invasive cancer. All diagnoses were identified using a list of codes for diagnosis and procedures available in the GPRD relying on the READ classification. Medications from the recorded prescriptions are identified using the coded drug dictionary based on the UK Prescription Pricing Authority Dictionary.
Cohort entry was defined as the date of first prescription of tamoxifen/AI. The maximum delay between the diagnostic code and the first prescription was 1 year to increase the likelihood that the treatment was prescribed as an adjuvant treatment for primary BC. We excluded patients who had a previous history of BC. We also excluded women who were metastatic at diagnosis or within the first 6 months after diagnosis. Patients who were prescribed simultaneously tamoxifen and AI and patients who had less than a year of data before cohort entry were also excluded.
All patients were followed from cohort entry to the end of treatment (theoretically 5 years), or until death from any cause, BC recurrence or contralateral BC, thrombo-embolic event, or endometrial cancer, whichever came first. If a patient switched between tamoxifen and AI or between two AIs during the study period, follow-up was censored at the time of the switch to calculate the compliance and persistence to the first drug.
Subcohorts were constituted according to age and date of diagnosis to account for the changes over time in clinical guidelines. Compliance and persistence were studied separately for women under 40 years of age and women 50 years and over at the time of diagnosis. For the younger group, tamoxifen was the only treatment studied as it remains the main therapeutic option for hormonal treatment in this mostly pre-menopausal subgroup of patients (Tam 40). For the latter group, owing to the recent recommendations on the use of AIs as adjuvant hormonal treatment in post-menopausal patients, these women were stratified according to the date of diagnosis to create an historical comparison group of tamoxifen users. This reference group was defined as having a diagnostic date before 2000 (Tam 50), when tamoxifen was generally prescribed for a 5-year period. Compliance and persistence to medication in this reference group was compared with the compliance and persistence to AIs among women diagnosed after 2006 (AI 50). Indeed, anastrozole and letrozole were licensed as adjuvant treatments for early BC in post-menopausal women in 2004 and 2005, respectively, in the UK, and UK clinical guidelines were updated in 2006 (National Institute for Health and Clinical Excellence, 2006).
Definition of measures of medication compliance and persistence.
Compliance was defined as the numbers of days covered by medication divided by the number of days between cohort entry and end of study participation. This proportion corresponds to the medication possession ratio (MPR) (Andrade et al, 2006; Cramer et al, 2008). For each woman, number of days covered by medication was calculated from the number of tablets prescribed combined with dosing instruction. From this information, we calculated the duration of the prescription. Durations of overlapping prescriptions were not added. A conventional cutoff of 80% or more days covered was used to calculate the proportion of women who where compliant with treatment (Fisher et al, 1989; Love, 1990; Waterhouse et al, 1993; Partridge et al, 2008). Women whose MPR was less than 80% were considered as non-compliant. We studied non-persistence to treatment defined as the first treatment discontinuation longer than 3 months. A gap of 3 months or more in medication coverage identified treatment discontinuation.
All treatments were handled similarly to limit differential misclassification of exposure.
Statistical analysis
Descriptive statistics were computed for continuous data (mean±standard deviation (s.d.)) and categorical data (sample size and percentage). Time to treatment discontinuation was calculated using Kaplan–Meier estimates to account for censored data. Patients follow-up was censored at 5 years (the theoretical duration of treatment), or at the date of death, BC recurrence or contralateral BC, thrombo-embolic event, endometrial cancer, or switch to a different antihormonal treatment, whichever came first. Results are expressed as cumulative probabilities of treatment discontinuation with 95% confidence intervals (CIs). Kaplan–Meier estimates of treatment discontinuation of the different subgroups were compared using the log-rank test.
All analyses were conducted with SAS version 9.1 (SAS Institute, Cary, NC, USA).
Results
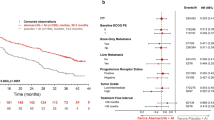
In the GPRD, we identified 24 489 women who received a first prescription of tamoxifen, anastrozole, letrozole or exemestane after 1 January 1998, who also had at least 1 year of data before this prescription in the database. We excluded 4218 women owing to the absence of a BC diagnostic code in their records, 5517 women because BC was diagnosed before the study period, 397 women because of metastases before or within the first 6 months after diagnosis and 17 had no date of diagnosis. We further excluded 516 women who received their first prescription more than 3 months before BC diagnosis, 328 who received their treatment more than a year after diagnosis and 17 women who were prescribed two drugs concomitantly (Figure 1). We therefore constituted a cohort of 13 479 women who received tamoxifen (n=10 806) or one of the AIs (n=2673) following the diagnosis of BC. Mean age at cohort entry was 62 years (s.d.=14.0) in the tamoxifen group and 70.8 (s.d.=12.4) in the AI group (Table 1).
We identified 416 women under 40 receiving tamoxifen as initial hormonal therapy (Tam 40), 1435 women over 50 diagnosed with BC before 2000 and receiving tamoxifen (Tam 50) and 1562 women over 50 diagnosed after 2006 and receiving AI (AI 50).
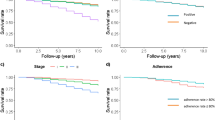
In the entire cohort, treatment discontinuation reached 29.8% of patients at 5 years. This rate ranged from 18.9% (95% CI: 15.1–23.0) for AIs users to 31.0% (95% CI: 29.6–32.2) for tamoxifen users (P<0.001) (Figure 2).
In the three subcohorts, rates of the treatment discontinuation in the first year ranged from 5.2% (95% CI: 4.0–6.6) to 20.1% (95% CI: 16.2–24.2) in the AI 50 and in the Tam 40 groups, respectively (Figure 3). At 5 years, more than half of the women (50.7%; 95% CI: 43.0–57.9) in the Tam 40 group had discontinued their treatment. Among women over 50, treatment discontinuation was less frequent for AIs as compared with tamoxifen (P<0.001).
Table 2 describes non-compliance, that is, MPR lower than 80% for patients receiving at least one prescription within that year. In the first year of treatment, non-compliance ranged from 9.5% in the AI 50 group to 23.6% in the Tam 40 group. Non-compliance reached 51.8% at 5 years in the latter group.
In the AI 50 group, 9.6% of women (150 out of 1562) had switched treatment by June 2008, corresponding to last data available for our study. Half of them switched from one AI to another AI, and the other half switched from AI to tamoxifen. Switches occurred within the first year of treatment in 76% of cases. Among women over 50 years of age who started a tamoxifen therapy after 2000, 31% switched to AI over the course of the study. Of these women, 12% switched within the first year of treatment (11.1 and 13.7% for women diagnosed in 2000–2004 and after 2005, respectively). A switch within the first year indicates a change in treatment not in accordance with medical guidelines, which recommend continuing tamoxifen treatment for a minimum of 2–3 years. This may indicate a switch for other reasons such as side effects.
Discussion
Among older women, the real-life patterns of use of AI show high rates of persistence to treatment. As compared with tamoxifen, AI therapy appears to be less frequently discontinued. In younger women, tamoxifen is prematurely interrupted for half of patients.
In clinical trials, compliance is likely to be optimal owing to the close monitoring of patients and the volunteer nature of such studies (Osterberg and Blaschke, 2005). Indeed, in the three largest trials on adjuvant tamoxifen for BC, about 20% of women discontinued their treatment prematurely (2001). In the ATAC trial, 88% of women allocated to AIs as compared with 87% on tamoxifen reported to be compliant with their treatment at 5 years (Forbes et al, 2008). Compliance rates in observational studies such as ours are expected to be lower than those reported in trials, and indeed our results are closer to those of previously published observational studies. Partridge et al (2008) reported for the first time data on AI compliance in a large commercial database. The mean compliance with anastrozole ranged from 82 to 88% in the first 12 months of treatment, and from 62 to 79% in the third year. Our results, taking into account that Partridge et al (2008) were focusing on prescription claims, whereas we are studying the prescription issued by the physician, are consistent.
However, our results comparing tamoxifen to AI use in older women contrast with these from the only comparative study available to date (Ziller et al, 2009). This German retrospective study on women initiating a treatment in 2004–2005 reported, in a small sample of women (n=89), a lower compliance with anastrozole (80 vs 69%). In the study time period, anastrozole was not a standard treatment according to the German treatment guidelines, although already largely prescribed. In this study, women who received anastrozole were older (65 years old on average for tamoxifen vs 72 for anastrozole) and had different tumour characteristics as compared with those receiving tamoxifen (e.g., 20% of in situ tumours for tamoxifen as compared with 3% for anastrozole) (i.e., indication bias). The different characteristics of women in the two groups may translate into different compliance rates. Oldest age group has been showed to be associated with lower compliance rates (Partridge et al, 2003; Barron et al, 2007; Kahn et al, 2007; Owusu et al, 2008). As tamoxifen is nowadays considered a less efficient adjuvant therapy to lower the risk of BC recurrence, it is in most cases only prescribed owing to personal characteristics of the patient (indication bias). To avoid this bias, compliance with AIs should be compared to compliance with tamoxifen when tamoxifen was the only therapeutic option. This is the reason why we used an historical cohort for the tamoxifen reference group when this latter treatment was the reference treatment.
Negative beliefs about treatment are known to decrease compliance in numerous diseases (Horne and Weinman, 1999). A similar association was found for tamoxifen in BC (Fink et al, 2004; Lash et al, 2006). Little is known on patients’ beliefs on AIs. However, as physicians were prompt to adopt AIs in replacement of tamoxifen even before publications of guidelines (Buzdar and Macahilig, 2005; Chlebowski, 2008), one can speculate that physicians were confident in the efficacy of a newer treatment and conveyed this message to patients. This may be a possible explanation for the lower rates of treatment discontinuation among women on AI, observed in our study. We need further studies and data to support this hypothesis. An alternative or complementary explanation may be a better treatment tolerance in the AI group as compared with tamoxifen as previously reported in the ATAC trial (Buzdar et al, 2006).
Previous observational studies on Tam have identified younger age as a factor associated with lower compliance (Partridge et al, 2003; Barron et al, 2007; Kahn et al, 2007; Hershman et al, 2010). One of these studies focused on self-report of compliance, likely to provide overestimates of compliance (Kahn et al, 2007). The three other studies reported prescription refill rates as estimates of compliance rates; however, they used either commercial database (Hershman et al, 2010) or databases comprising mostly socially disadvantaged women (Partridge et al, 2003; Barron et al, 2007). However, in the subgroup of younger patients, no specific description of the rates of compliance and patterns of treatment discontinuation has been provided. The rapid decrease in use of tamoxifen that we observed is of particular concern in this subgroup of women. They present poorer outcomes of BC as compared with older women (Adami et al, 1986; Chung et al, 1996; Gnerlich et al, 2009). There is no alternative recommended hormonal treatment available and as it has been established that a 1- or 2-year treatment is less effective than a full 5-year course (1998). The high rates of non-persistence contrast with the study of Thewes et al (2005) reporting, using patient preference interviews, that modest gains in survival were sufficient for women under 40 with BC to find worthwhile a 5-year tamoxifen treatment. The reasons for early treatment discontinuation are largely unknown in younger women. However, several specificity of this subgroup may have a role in the difference of compliance observed. Younger women face specific consequences of systemic treatment including menopausal symptoms, sexual dysfunction, and fertility issues (Fallowfield et al, 1999; Pellegrini et al, 2009), and they also suffer from higher psychosocial distress and lower quality of life after BC as compared with older women (Mor et al, 1994; Ganz et al, 2003).
Our study has several strengths. First, it is population based as opposed to studies using commercial health programme databases. These latter sources of data provide results that may be systematically biased because of the exclusion of different subgroups of the general population depending on the programme eligibility. Access to medical care and cost of treatment is likely to impact compliance. In the UK, National Health Services provide universal coverage. During the time period of the study, treatments were dispensed with a fixed prescription charge per item. Exemption of prescription charges are based on patient characteristics (e.g., over 60 years of age). Use of treatment is measured in our study with no differential cost issues between tamoxifen and AIs. The difference observed between the two treatments is therefore independent of cost issues. Second, the validity of the information recorded in our source of data, the GPRD, has been largely studied and shown to be high. In terms of the recorded information on drug exposures and diagnoses, the GPRD has been validated (Lawrenson et al, 1999, 2000; Jick et al, 2003). More specifically, this database provides BC incidence closely similar to that of the national registration data (Kaye et al, 2000). Third, the size of the database enabled the selection of large samples even for our smaller group, BC in younger women. Fourth, we are studying prescriptions written by physicians, an objective measure of exposure, free of recall bias because of the prospective nature of data collection in the GPRD.
A limitation of our study is that we do not have access to exact data on patient compliance. Prescriptions written by physician overestimate what patients actually ingest. However, although methodologies to evaluate compliance are numerous, they all have advantages and disadvantages and none is considered as a gold standard (Osterberg and Blaschke, 2005). Rate of prescription refills is an objective measure and has been shown in countries with universal health coverage to provide accurate measures of overall compliance (Lau et al, 1997). We use a proxy measure of prescription refills as we have access to prescription issued by the GP. Moreover, the clinical significance of our results is not modified by the fact that we underestimate treatment discontinuation rates. At least half of women stop their treatment prematurely, a proportion large enough to stress the need for intervention to improve compliance with and maintenance of treatment. Third, while tamoxifen and AI use may be overestimated, this overestimation affects both groups similarly and therefore the magnitude of the difference between younger and older women and between tamoxifen and AI is not likely to be modified.
To our knowledge, our study is the first large observational study to report comparative data on the use of AIs as compared to tamoxifen and to provide detailed information on real-life use of tamoxifen in younger women.
Change history
29 March 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Clarke M, Collins R, Davies C, Godwin J, Gray R, Peto R (The EBCTCG secretariat) (1998) Tamoxifen for early breast cancer: an overview of the randomised trials. Early Breast Cancer Trialists’ Collaborative Group. Lancet 351: 1451–1467
Early Breast Cancer Trialists' Collaborative Group (2001) Tamoxifen for early breast cancer. Cochrane Database Syst Rev (1): CD000486. doi:10.1002/14651858
National Institute for Health and Clinical Excellence (2006) Hormonal Therapies for the Adjuvant Treatment of Early Oestrogen-Receptor-Positive Breast Cancer – National Institute for Health and Clinical Excellence. Nice Technology Appraisal Guidance 112, NHS: London
Adami HO, Malker B, Holmberg L, Persson I, Stone B (1986) The relation between survival and age at diagnosis in breast cancer. N Engl J Med 315: 559–563
Andrade SE, Kahler KH, Frech F, Chan KA (2006) Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf 15: 565–574; discussion 575–577
Barron TI, Connolly R, Bennett K, Feely J, Kennedy MJ (2007) Early discontinuation of tamoxifen: a lesson for oncologists. Cancer 109: 832–839
Burstein HJ, Prestrud AA, Seidenfeld J, Anderson H, Buchholz TA, Davidson NE, Gelmon KE, Giordano SH, Hudis CA, Malin J, Mamounas EP, Rowden D, Solky AJ, Sowers MR, Stearns V, Winer EP, Somerfield MR, Griggs JJ (2010) American Society of Clinical Oncology clinical practice guideline: update on adjuvant endocrine therapy for women with hormone receptor-positive breast cancer. J Clin Oncol 28: 3784–3796
Buzdar A, Macahilig C (2005) How rapidly do oncologists respond to clinical trial data? Oncologist 10: 15–21
Buzdar A, Howell A, Cuzick J, Wale C, Distler W, Hoctin-Boes G, Houghton J, Locker GY, Nabholtz JM (2006) Comprehensive side-effect profile of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: long-term safety analysis of the ATAC trial. Lancet Oncol 7: 633–643
Chlebowski RT (2008) Clinical trial presentations, agency guidelines, and oncology practice: findings from the arimidex, tamoxifen, alone or in combination trial. Clin Breast Cancer 8: 343–346
Chung M, Chang HR, Bland KI, Wanebo HJ (1996) Younger women with breast carcinoma have a poorer prognosis than older women. Cancer 77: 97–103
Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, Wong PK (2008) Medication compliance and persistence: terminology and definitions. Value Health 11: 44–47
Crivellari D, Sun Z, Coates AS, Price KN, Thurlimann B, Mouridsen H, Mauriac L, Forbes JF, Paridaens RJ, Castiglione-Gertsch M, Gelber RD, Colleoni M, Lang I, Del Mastro L, Gladieff L, Rabaglio M, Smith IE, Chirgwin JH, Goldhirsch A (2008) Letrozole compared with tamoxifen for elderly patients with endocrine-responsive early breast cancer: the BIG 1-98 trial. J Clin Oncol 26: 1972–1979
Demissie S, Silliman RA, Lash TL (2001) Adjuvant tamoxifen: predictors of use, side effects, and discontinuation in older women. J Clin Oncol 19: 322–328
Dezentje V, Van Blijderveen NJ, Gelderblom H, Putter H, Van Herk-Sukel MP, Casparie MK, Egberts AC, Nortier JW, Guchelaar HJ (2009) Concomitant CYP2D6 inhibitor use and tamoxifen adherence in early-stage breast cancer: a pharmacoepidemiologic study. J Clin Oncol 27: 18s
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) (2005) Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 365: 1687–1717
Fallowfield LJ, Leaity SK, Howell A, Benson S, Cella D (1999) Assessment of quality of life in women undergoing hormonal therapy for breast cancer: validation of an endocrine symptom subscale for the FACT-B. Breast Cancer Res Treat 55: 189–199
Fink AK, Gurwitz J, Rakowski W, Guadagnoli E, Silliman RA (2004) Patient beliefs and tamoxifen discontinuance in older women with estrogen receptor-positive breast cancer. J Clin Oncol 22: 3309–3315
Fisher B, Costantino J, Redmond C, Poisson R, Bowman D, Couture J, Dimitrov NV, Wolmark N, Wickerham DL, Fisher ER, Margolese R, Robidoux A, Shibata H, Terz J, Paterson AHG, Feldman MI, Farrar W, Evans J, Lickley HL, Ketner M, Abramson N, Allegra JC, Beazley R, Berry J, Boatman KK, Carmichael D, Cruz AB, Davies R, Deckers P, Desser R, Dimitrov N, Economou S, Elias EG, Foster RS, Frazier TG, Glass AG, Jochimsen P, Jubelirer S, Kardinal CG, Keyserlingk JR, Lerner HJ, Levick SN, Mahoney L, Mowry P, Nicola M, Oishi R, Pasquale D, Perrault D, Peters G, Pugh R, Robert N, Spector J, Sponzo R, Sterchi JM, Sutherland CM, Thiessen AR, Thirlwell M, Welling R, Wold H, Wozniak T (1989) A randomized clinical trial evaluating tamoxifen in the treatment of patients with node-negative breast cancer who have estrogen-receptor-positive tumors. N Engl J Med 320: 479–484
Forbes JF, Cuzick J, Buzdar A, Howell A, Tobias JS, Baum M (2008) Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 100-month analysis of the ATAC trial. Lancet Oncol 9: 45–53
Ganz PA, Greendale GA, Petersen L, Kahn B, Bower JE (2003) Breast cancer in younger women: reproductive and late health effects of treatment. J Clin Oncol 21: 4184–4193
García Rodríguez LA, Pérez-Gutthann S, Jick S (2002) The UK General Practice Research Database. In Pharmacoepidemiology, Strom BL (ed.) 3rd edn. John Wiley & Sons, Ltd: Chichester, UK
Gnerlich JL, Deshpande AD, Jeffe DB, Sweet A, White N, Margenthaler JA (2009) Elevated breast cancer mortality in women younger than age 40 years compared with older women is attributed to poorer survival in early-stage disease. J Am Coll Surg 208: 341–347
Goldhirsch A, Ingle JN, Gelber RD, Coates AS, Thurlimann B, Senn HJ (2009) Thresholds for therapies: highlights of the St Gallen International Expert Consensus on the primary therapy of early breast cancer 2009. Ann Oncol 20: 1319–1329
Hershman DL, Kushi LH, Shao T, Buono D, Kershenbaum A, Tsai WY, Fehrenbacher L, Lin Gomez S, Miles S, Neugut AI (2010) Early discontinuation and nonadherence to adjuvant hormonal therapy in a cohort of 8769 early-stage breast cancer patients. J Clin Oncol 28: 4120–4128
Horne R, Weinman J (1999) Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res 47: 555–567
Jick SS, Kaye JA, Vasilakis-Scaramozza C, Garcia Rodriguez LA, Ruigomez A, Meier CR, Schlienger RG, Black C, Jick H (2003) Validity of the General Practice Research Database. Pharmacotherapy 23: 686–689
Kahn KL, Schneider EC, Malin JL, Adams JL, Epstein AM (2007) Patient centered experiences in breast cancer: predicting long-term adherence to tamoxifen use. Med Care 45: 431–439
Kaye JA, Derby LE, del Mar Melero-Montes M, Quinn M, Jick H (2000) The incidence of breast cancer in the General Practice Research Database compared with national cancer registration data. Br J Cancer 83: 1556–1558
Lash TL, Fox MP, Westrup JL, Fink AK, Silliman RA (2006) Adherence to tamoxifen over the five-year course. Breast Cancer Res Treat 99: 215–220
Lau HS, de Boer A, Beuning KS, Porsius A (1997) Validation of pharmacy records in drug exposure assessment. J Clin Epidemiol 50: 619–625
Lawrenson R, Todd JC, Leydon GM, Williams TJ, Farmer RD (2000) Validation of the diagnosis of venous thromboembolism in general practice database studies. Br J Clin Pharmacol 49: 591–596
Lawrenson R, Williams T, Farmer R (1999) Clinical information for research: the use of general practice databases. J Public Health Med 21: 299–304
Love RR (1990) Prospects for antiestrogen chemoprevention of breast cancer. J Natl Cancer Inst 82: 18–21
McCowan C, Shearer J, Donnan PT, Dewar JA, Crilly M, Thompson AM, Fahey TP (2008) Cohort study examining tamoxifen adherence and its relationship to mortality in women with breast cancer. Br J Cancer 99: 1763–1768
Mor V, Malin M, Allen S (1994) Age differences in the psychosocial problems encountered by breast cancer patients. J Natl Cancer Inst Monogr 1994 (16): 191–197
Osterberg L, Blaschke T (2005) Adherence to medication. N Engl J Med 353: 487–497
Owusu C, Buist DS, Field TS, Lash TL, Thwin SS, Geiger AM, Quinn VP, Frost F, Prout M, Yood MU, Wei F, Silliman RA (2008) Predictors of tamoxifen discontinuation among older women with estrogen receptor-positive breast cancer. J Clin Oncol 26: 549–555
Partridge AH, Avorn J, Wang PS, Winer EP (2002) Adherence to therapy with oral antineoplastic agents. J Natl Cancer Inst 94: 652–661
Partridge AH, LaFountain A, Mayer E, Taylor BS, Winer E, Asnis-Alibozek A (2008) Adherence to initial adjuvant anastrozole therapy among women with early-stage breast cancer. J Clin Oncol 26: 556–562
Partridge AH, Wang PS, Winer EP, Avorn J (2003) Nonadherence to adjuvant tamoxifen therapy in women with primary breast cancer. J Clin Oncol 21: 602–606
Pellegrini I, Sarradon-Eck A, Ben Soussan P, Lacour AC, Largillier R, Tallet A, Tarpin C, Julian-Reynier C (2009) Women's perceptions and experience of adjuvant tamoxifen therapy account for their adherence: breast cancer patients’ point of view. Psychooncology 19 (5): 472–479
Ruddy K, Mayer E, Partridge A (2009) Patient adherence and persistence with oral anticancer treatment. CA Cancer J Clin 59: 56–66
Thewes B, Meiser B, Duric VM, Stockler MR, Taylor A, Stuart-Harris R, Links M, Wilcken N, McLachlan SA, Phillips KA, Beith J, Boyle F, Friedlander ML (2005) What survival benefits do premenopausal patients with early breast cancer need to make endocrine therapy worthwhile? Lancet Oncol 6: 581–588
Waterhouse DM, Calzone KA, Mele C, Brenner DE (1993) Adherence to oral tamoxifen: a comparison of patient self-report, pill counts, and microelectronic monitoring. J Clin Oncol 11: 1189–1197
Ziller V, Kalder M, Albert US, Holzhauer W, Ziller M, Wagner U, Hadji P (2009) Adherence to adjuvant endocrine therapy in postmenopausal women with breast cancer. Ann Oncol 20: 431–436
Acknowledgements
This study was funded by the Canadian Institutes of Health Research (CIHR) and Canada Foundation for Innovation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Huiart, L., Dell'Aniello, S. & Suissa, S. Use of tamoxifen and aromatase inhibitors in a large population-based cohort of women with breast cancer. Br J Cancer 104, 1558–1563 (2011). https://doi.org/10.1038/bjc.2011.140
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2011.140
Keywords
This article is cited by
-
Metformin as a new option in the medical management of breast fibroadenoma; a randomized clinical trial
BMC Endocrine Disorders (2021)
-
Outcomes of primary endocrine therapy in elderly women with stage I–III breast cancer: a SEER database analysis
Breast Cancer Research and Treatment (2020)
-
Factors influencing adherence to adjuvant endocrine therapy in breast cancer-treated women: using real-world data to inform a switch from acute to chronic disease management
Breast Cancer Research and Treatment (2020)
-
First prospective outcome data for the second-generation multigene test Endopredict in ER-positive/HER2-negative breast cancer
Archives of Gynecology and Obstetrics (2020)
-
Factors associated with endocrine therapy adherence among post-menopausal women treated for early-stage breast cancer in Ontario, Canada
Breast Cancer Research and Treatment (2020)