Abstract
Background:
Women using unopposed estrogens during menopause are at increased risk of ovarian cancer. It is uncertain whether oestrogen plus progestin therapy exerts similar effects.
Methods:
We evaluated menopausal hormone use and incident ovarian cancer (n=426) in 92 601 post-menopausal women enrolled in the National Institutes of Health-AARP (NIH-AARP) Diet and Health Study. Participants were administered questionnaires in 1996–1997 and followed through 2006. Hazard rate ratios (RR) and 95% confidence intervals (CIs) were estimated using Cox regression.
Results:
Increased risks were associated with long duration (10+ years) use of unopposed oestrogen (RR 2.15, 95% CI: 1.30–3.57 among women with a hysterectomy) and oestrogen plus progestin (RR 1.68, 95% CI: 1.13–2.49 among women with intact uteri) therapy. Similar risks were associated with progestins that were used sequentially (<15 days progestin per month) (RR 1.60, 95% CI: 1.10–2.33) or continuously (>25 days progestin per month) (RR 1.43, 95% CI: 1.032–2.01; P-value for heterogeneity=0.63).
Conclusion:
Our findings suggest that long duration use of both unopposed estrogens and oestrogen plus progestins are associated with increased risks of ovarian cancer, and that risk associated with oestrogen plus progestin use does not vary by regimen (sequential or continuous).
Similar content being viewed by others
Main
Menopausal hormone therapy has been associated with increased ovarian cancer incidence and mortality (Rodriguez et al, 2001; Danforth et al, 2007; Greiser et al, 2007; Rossing et al, 2007). Recently, the Endocrine Society published a formal statement concluding that long-term unopposed oestrogen menopausal hormone therapy use is associated with an increased, albeit small, risk of ovarian cancer (Santen et al, 2010). The report cited that the association between oestrogen plus progestin menopausal hormone therapy and ovarian cancer risk is inconclusive and requires further study (Santen et al, 2010). A greater reduction in ovarian cancer risk with oral contraceptives containing high-dose progestins (Schildkraut et al, 2002) has led to the suggestion that progestins may be protective and mitigate some of the ovarian cancer risk associated with unopposed estrogens. Not all studies, however, support an antagonistic role for progestins. Some have reported increased ovarian cancer risk associated with combination oestrogen plus progestin hormone therapy compared with non-users (Lacey et al, 2006; Beral et al, 2007; Morch et al, 2009). Further, it remains unclear among combination users whether the regimen of progestin use is important; although some studies report lower ovarian cancer risk estimates for continuous as compared with sequential progestin use (Pearce et al, 2009), other studies report no substantial differences by regimen (Morch et al, 2009).
To address outstanding questions regarding ovarian cancer risk as related to the use of menopausal hormone therapy, specifically oestrogen plus progestin therapy, we conducted an analysis in the National Institutes of Health-AARP (NIH-AARP) Diet and Health Study, a large prospective study with comprehensive data on menopausal hormone use. An increased risk of ovarian cancer with oestrogen plus progestin use was previously reported using data from this cohort with follow-up through 2000 (Lacey et al, 2006). The results from the prior analysis, albeit based on small numbers, suggested that sequential oestrogen plus progestin users had a greater risk of ovarian cancer than continuous users. Given 6 additional years of follow-up and twice as many ovarian cancer cases, we were able with increased power to evaluate the risks associated with long duration oestrogen plus progestin use and regimen (sequential vs continuous use of progestins) of use.
Materials and methods
Study population
The NIH-AARP Diet and Health Study design and methodology has been described previously (Schatzkin et al, 2001). Briefly, the NIH-AARP Diet and Health Study cohort was established during 1995 and 1996 when 3.5 million AARP members aged 50–71 years and residing in one of six states (California, Florida, Louisiana, New Jersey, North Carolina, and Pennsylvania) or two metropolitan areas (Atlanta, Georgia and Detroit, Michigan) were invited to complete a baseline questionnaire. Approximately 18% of the cohort (n=617 119) returned the self-administered questionnaire, 566 399 of which were non-duplicate and satisfactorily completed. A second questionnaire (1996–1997) collecting detailed information on menopausal hormone therapy use, family history of cancer, and physical activity was mailed to baseline questionnaire respondents who did not have self-reported colon, breast, or prostate cancer and was returned by 334 906 individuals (59%). We excluded male participants (n=188 116) and participants who used a proxy respondent for the baseline (n=6959) or second questionnaire (n=3424). The study population included 136 407 potentially eligible women. The Special Studies Institutional Review Board of the US National Cancer Institute approved the study and all the participants gave informed consent.
The cohort follow-up included periodic matching of the cohort database with the National Change of Address database maintained by the US Postal Service and through processing of undeliverable mail, other address update services, and direct responses from participants. Vital status was ascertained by linkage to the US Social Security Administration Death Master File with verification in the National Death Index Plus. The loss to follow-up of cohort participants was <5%.
Analytic population
We excluded women who reported a previous diagnosis of cancer other than non-melanoma skin cancer or a prior diagnosis of cancer other than non-melanoma skin cancer on their death certificate (n=9471). We further excluded women who were premenopausal at baseline (n=4421) and women who reported a bilateral oophorectomy (n=27 512), unknown oophorectomy status (n=2107), or menstrual periods that stopped due to radiation or chemotherapy (n=66). Women who developed non-epithelial ovarian cancer during follow-up (n=35), borderline histology (n=1) or non-primary ovarian cancer (n=113) during follow-up were also excluded. Finally, women with missing values for menopausal hormone use variables (n=80) were excluded. After these additional exclusions the analytic cohort consisted of 92 601 women with at least one intact ovary.
Exposure ascertainment
Information on menopausal hormone use was based on data collected in the second questionnaire only, this questionnaire included detailed questions on ‘replacement hormone use’, as described previously (Lacey et al, 2006). Briefly, this questionnaire collected information about oestrogen and progestin use separately and did not include questions about the combined oestrogen plus progestin pill, which was first marketed in 1995. Participants reported the dates of first and last use, recency of use, total duration of use, usual dose, and name of the pill that they took for the longest time for each pill type. For duration of use, women were asked to report the total duration of use in 1-year increments up to 10 years, with a single category for use >10 years.
Incident ovarian cancer ascertainment
Incident ovarian cancers were identified through probabilistic linkage with cancer registries in the original recruitment areas and three common relocation states (Arizona, Nevada and Texas). The state cancer registries have been certified by the North American Association of Central Cancer Registries and capture at least 95% of the cancer incidences within 24 months of cancer occurrence. Further, a validation study that compared registry findings with self-reports and medical records estimated that registry linkage validly identified ∼90% of all incident cancers (Michaud et al, 2005). Of the 92 601 post-menopausal women available for analysis, 426 were diagnosed with incident epithelial ovarian cancer after completing the second questionnaire and on or before December 31, 2006. We further classified the incident epithelial ovarian cancers as serous (n=228), endometrioid (n=31), mucinous (n=20), clear cell (n=14), and other (n=133) based on International Classification of Diseases for Oncology morphology codes as described previously (Yang et al, 2012).
Statistical analysis
Cox proportional hazards regression was used to estimate rate ratios (RR) and 95% confidence intervals (CIs) with age as the time metric and ties handled by complete enumeration. Follow-up time began at the scan date of the second questionnaire and continued until diagnosis of first primary cancer, date of death, date moved out of registry ascertainment area, or December 31, 2006, whichever came first.
Oestrogen plus progestin only was defined if the reported date of progestin therapy use was within 90 days of unopposed oestrogen use. In the oestrogen plus progestin only analyses, we modelled unopposed oestrogen followed by oestrogen plus progestin as a separate variable to avoid any residual influence on risk of former unopposed oestrogen use. We defined sequential regimen usage as oestrogen with progestin use for <15 days per month, and continuous regimen usage as oestrogen with ‘daily’ use of progestin (>25 days per month). The usage pattern that included progestin use 15–25 days per month was modelled as a separate variable in statistical models; however, the number of cases was small and the effect estimates were consistent with sequential and continuous regimens and are not reported.
All models were adjusted for age at cohort entry, race, body mass index (BMI), age at menopause, parity, and duration of oral contraceptive use at baseline. Models evaluating unopposed oestrogen therapy were restricted to women who had reported a hysterectomy at baseline, and models evaluating combination oestrogen plus progestin therapy were restricted to women with intact uteri at baseline. Tests for linear trends across hormone use categories were calculated using a grouped linear variable. Likelihood ratio tests for interaction across levels of oral contraceptive use, parity, smoking history, BMI, and family history of breast cancer were computed based on cross-product terms with hormone use. The assumption of proportional hazards for each adjustment variable and main effect was tested using a likelihood ratio test of interaction with the time-scale (continuous) based on cross-product terms. The P-values for all comparisons were two-sided and an alpha <0.05 indicated statistical significance. SAS statistical software, version 9.2 (SAS Institute Inc., Cary, NC, USA) was used for all analyses.
Results
Characteristics of the cohort
A total of 92 601 women with at least one intact ovary at baseline contributed 822 409 person-years, with mean follow-up of 4.7 years for ovarian cancer cases and 8.9 years for non-cases. The mean age at baseline of all participants was 62.3 years and the study population was predominantly white (91.2%). Ovarian cancer was inversely associated with duration of oral contraceptive use and parity (results not shown).
Hormone usage patterns
Forty-six percent (n=42 204) of the post-menopausal women with at least one intact ovary reported never using menopausal hormones on the second questionnaire, whereas 19.4% (n=17 922) reported using oestrogen-only hormone therapy, 31.0% (n=28 707) reported using any oestrogen plus progestin, and 4.1% (n=3768) reported other or unknown type of hormone therapy. Of the women who reported using any oestrogen plus progestin, 68.7% (n=19 726) reported using oestrogen plus progestin only, 13.3% (n=3822) reported using oestrogen alone followed by some combination of oestrogen plus progestin, and the remaining 18.0% (n=5159) used other combinations of hormones.
Baseline characteristics of the women included in our analyses are presented in Table 1 according to menopausal hormone use (never/ever) and type (oestrogen-only/oestrogen plus progestin-only). Compared with non-hormone users, women who used unopposed estrogens were more often oral contraceptive users, multiparous, and thin, while women who used oestrogen plus progestin were more frequently young, white, older when they experienced natural menopause, oral contraceptive users and thin. As expected, unopposed oestrogen users (72.3%) were more likely to have had a hysterectomy as compared with oestrogen plus progestin only users (2.6%) or non-hormone users (14.9%).
Risk of ovarian cancer among women using unopposed oestrogen only
Among women with a hysterectomy, exclusive use of unopposed estrogens was associated with an increased risk of ovarian cancer compared with women who reported never using menopausal hormones (RR 1.69, 95% CI: 1.05, 2.71) (Table 2). The risk was substantially elevated among women who reported long duration (⩾10 years) unopposed oestrogen only use (RR 2.151, 95% CI: 1.30, 3.57); whereas shorter duration (<10 years) unopposed oestrogen only use was not associated with increased risk (RR 1.25, 95% CI: 0.71, 2.20).
Risk of ovarian cancer among women using only oestrogen plus progestin
Exclusive use of oestrogen plus progestin therapy was associated with an increased risk of ovarian cancer compared with women who reported never using menopausal hormones (RR 1.43; 95% CI: 1.09, 1.86) (Table 3). Long duration (⩾10 years) oestrogen plus progestin use was also associated with increased risk (RR 1.68; 95% CI: 1.13, 2.49). The risk estimate associated with short-duration use was also elevated, although the estimate did not achieve statistical significance. Higher-dose progestins (5 mg and 10 mg) were associated with increased, albeit not statistically significant, risk (5 mg RR 1.60; 95% CI: 0.95, 2.68; 10 mg RR 1.58; 95% CI: 0.90, 2.79). The number of days per month on progestin did not influence ovarian cancer risk (P-trend=0.70). Use of either sequential (<15 days progestin per month) or continuous (>25 days progestin per month) progestins were associated with similar increases in ovarian cancer risk (sequential RR 1.60; 95% CI: 1.10, 2.33; continuous RR 1.43; 95% CI: 1.03, 2.01; P-value for heterogeneity=0.63). We attempted to evaluate how duration of use affected the risk associated with sequential or continuous regimen use, but small numbers of long-term users precluded any definitive conclusions.
Based on the likelihood ratio test of interaction, the association between menopausal hormone use and ovarian cancer was not significantly modified by prior oral contraceptive use (all P-values for interaction in Table 4 >0.05). Although the interaction models in Table 4 suggest that the menopausal hormone-ovarian cancer association is apparent only among women who reported never or short-duration (<1 years) oral contraceptive use, the risk estimates among women who used oral contraceptives for longer durations (⩾1 years) should be interpreted with caution as they are based on a small numbers in some categories. Other factors associated with ovarian cancer risk including parity, smoking history, BMI, or family history of breast cancer did not significantly modify the associations between menopausal hormone use and ovarian cancer risk (results not shown).
We evaluated associations for serous and other histological types, combined as a single group as there were too few endometrioid, clear cell, or mucinous cancers to reliably evaluate their separate relationships (Table 5). We found that the increased risks associated with unopposed oestrogen (RR 2.82; 95% CI: 1.31, 6.04) and oestrogen plus progestin (RR 1.83; 95% CI: 1.28, 2.61) menopausal hormones were limited to women with serous histology. Long duration unopposed oestrogen (RR 3.32; 95% CI: 1.49, 7.44) and long duration oestrogen plus progestin use (RR 1.97; 95% CI: 1.17, 3.34) were associated with serous ovarian cancer risk, as well as sequential (RR 1.87; 95% CI: 1.14, 3.08) and continuous regimen (RR 2.02; 95% CI: 1.32, 3.08) use. The combined category of ‘other’ histologic subtypes was not associated with unopposed oestrogen or oestrogen plus progestin menopausal hormone use.
Associations were not significantly different when evaluated by tumour stage or grade (results not shown). The results were essentially unchanged after further adjustment for calendar time and several additional ovarian cancer risk factors, including age at menarche, age at natural menopause, first-degree family history of breast cancer, marital status, or educational attainment (results not shown). We performed a sensitivity analysis of the association between menopausal hormone therapy and ovarian cancer whereby we truncated the follow-up at June 30th, 2002, to account for potential changes in menopausal hormone therapy use or prescribing patterns following the WHI trial report, suggesting that menopausal hormones should not be recommended for chronic disease prevention in post-menopausal women (Rossouw et al, 2002; Anderson et al, 2003). The truncated results were not substantially different (results not shown).
Discussion
In this large prospective analysis in the NIH-AARP Diet and Health Study cohort, long duration use of either unopposed oestrogen or oestrogen plus progestin menopausal hormone therapy was associated with increased ovarian carcinoma risk. Further, the increased risk related to oestrogen plus progestin use was not reduced by increasing days per month of progestin nor was there a difference in risk comparing sequential and continuous regimen usage, suggesting that the relationship between estrogens and ovarian cancer risk is not attenuated by the addition of progestins, even when prescribed continuously.
The increased risks we observed for long duration unopposed oestrogen and oestrogen plus progestin therapy are consistent with results from a previous investigation within the NIH-AARP Diet and Health study (Lacey et al, 2002). In contrast to the prior study, the current analysis reports similar magnitude increased risk of ovarian cancer for both sequential and continuous regimen oestrogen plus progestin. In the prior analysis, ovarian cancer risk was greater for sequential than continuous oestrogen plus progestin users, but given the shorter follow-up period the risk estimate for continuous regimen oestrogen plus progestin did not attain statistical significance.
Cohort studies have consistently reported an increased risk of ovarian cancer with unopposed oestrogen use (Lacey et al, 2002; Danforth et al, 2007; Beral et al, 2007; Morch et al, 2009; Hildebrand et al, 2010; Tsilidis et al, 2011). An association with oestrogen plus progestin use has been less consistent; however, a meta-analysis of population-based case–control, cohort and clinical trial data published through 2007 reported an increased risk of ovarian cancer per 5 years of use for both unopposed oestrogen and oestrogen plus progestin therapies (Pearce et al, 2009). Further, the authors reported higher risk estimate for unopposed oestrogen use than oestrogen plus progestin use (Pearce et al, 2009). Three additional cohort studies have been published since the meta-analysis (Morch et al, 2009; Hildebrand et al, 2010; Tsilidis et al, 2011); the largest of which, the Danish Sex Hormone Register Study, included 2681 ovarian cancers and reported an increased risk of ovarian cancer with current use of oestrogen plus progestin (Morch et al, 2009). Our finding of an increased risk of ovarian cancer with oestrogen plus progestin use is consistent with the results from the Danish Sex Hormone Register Study (Morch et al, 2009) and the meta-analysis (Pearce et al, 2009) and provides evidence that progestins do not mitigate the ovarian cancer risk associated with post-menopausal exposure to unopposed estrogens. Further supporting the notion that ovarian cancer risk does not depend on whether progestins were prescribed sequentially or continuously, the current analysis and the Danish Sex Hormone Register Study also reported increased risk for continuous oestrogen plus progestin use, which was not significantly different than the risk observed for sequential oestrogen plus progestin use (Morch et al, 2009).
A number of case–control (Purdie et al, 1995; Risch et al, 1996; Pike and Spicer, 2000; Riman et al, 2002; Moorman et al, 2005; Rossing et al, 2007) and cohort (Lacey et al, 2002; Danforth et al, 2007; Hildebrand et al, 2010; Tsilidis et al, 2011) studies have reported null associations for oestrogen plus progestin use and ovarian cancer risk. The inconsistency in reports may partly be explained by the small number of menopausal hormone users in some studies, differences in the categorisation of days per month on progestin, type of progestin prescribed in the United States vs Europe, evaluation of current vs ever users of oestrogen plus progestin, or lack of adjustment for or stratification by hysterectomy status.
Consistent with previous investigations (Lacey et al, 2002; Beral et al, 2007), we found that the menopausal hormone therapy-ovarian cancer associations did not vary significantly according to the presence or absence of ovarian cancer risk factors. The analyses evaluating the association between menopausal hormone use and ovarian cancer across categories of prior oral contraception use were based on small numbers and should be interpreted with caution.
Few cohort studies have reported analyses by histologic type (Beral et al, 2007; Danforth et al, 2007; Tsilidis et al, 2011; Morch et al, 2012). The current use of menopausal hormones was associated with serous tumours in the Million Women Study (Beral et al, 2007); however, current use of any menopausal hormone was not associated with any histologic type in the European Prospective Investigation into Cancer and Nutrition (Tsilidis et al, 2011). Unopposed oestrogen use was associated with serous and endometrioid tumours in the Nurse’s Health Study and the Danish Sex Hormone Register Study (Danforth et al, 2007; Morch et al, 2012). Oestrogen plus progestins use was not associated with serous or endometrioid tumours in the Nurse’s Health Study, but it was associated with increased serous and endometrioid tumours in the Danish Sex Hormone Register Study (Danforth et al, 2007; Morch et al, 2012). Other prospective studies have not reported risk estimates by subtype (Lacey et al, 2002; Hildebrand et al, 2010). We report increased risk of serous tumours associated with both unopposed oestrogen and oestrogen plus progestin menopausal hormone therapy, regardless of whether progestins were prescribed sequentially or continuously—a finding that is consistent with results from the Danish Sex Hormone Register Study (Morch et al, 2012).
The major strengths of the current study include the use of a large prospective cohort of primarily post-menopausal women with extensive data on menopausal hormone therapy use and long duration of follow-up. The detailed questionnaire provided information on potential confounders and effect modifiers, which allowed for a thorough assessment of the independence of menopausal hormone use from other related factors and the evaluation of potential joint effects between menopausal hormones and known ovarian cancer risk factors.
As participants of the NIH-AARP study represent mainly white, post-menopausal women who consented to participate, the results of the current study may not apply to all women. Another limitation of this study is that menopausal hormone usage patterns were only collected as part of second questionnaire administered in 1996–1997. We therefore could not evaluate whether cessation of or changes in menopausal hormone usage patterns after exposure assessment differed by ovarian cancer status. Hormone usage patterns among our cohort participants likely changed during follow-up given increases in hormone use in the United States leading up to the early termination of the WHI trial in 2002 and subsequent changes in prescribing patterns. However, a sensitivity analysis truncating follow-up at June 30th 2002 did not materially attenuate our results. Further, the reported duration of use at baseline would have systematically underestimated the true total duration of menopausal hormone therapy use in the population during the study period. We did not have information on gynaecologic surgery after baseline; therefore the inability to censor women who had an oophorectomy during follow-up was also a study limitation. Hysterectomy prevalence during the study period increased, with bilateral oophorectomy accompanying approximately half of those hysterectomy procedures. However, hysterectomy rates decline markedly after menopause (Merrill, 2001); therefore the expected number of women in the NIH-AARP Diet and Health Study who received an oophorectomy after baseline is small.
Menopausal hormone therapy is the most effective treatment available for vasomotor symptoms associated with oestrogen deficiency during the menopausal transition. Current guidelines recommend use of the lowest effective dose of menopausal hormone therapy for the shortest possible duration. Chronic disease associations with short duration, low dose use have not been thoroughly evaluated. When risks are resolved they will need to be weighed in relation to a number of benefits (Santen et al, 2010).
In conclusion, our results suggest that long duration use of both unopposed estrogens and oestrogen plus progestins are associated with increased risks of ovarian cancer, and that risk associated with oestrogen plus progestin use does not vary by regimen (sequential or continuous). Although there has been previous uncertainty regarding whether oestrogen plus progestin hormone therapy has a substantial impact on ovarian cancer risk, there appears to be growing evidence that long-term oestrogen plus progestin confers increased risk. Larger studies are still needed to evaluate ovarian cancer risk with short-duration oestrogen plus progestin use according to different regimens, as well as evaluate effect modification with known risk factors of ovarian cancer (e.g., oral contraception use, smoking, BMI, parity, etc.).
Change history
10 September 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Anderson GL, Judd HL, Kaunitz AM, Barad DH, Beresford SA, Pettinger M, Liu J, McNeeley SG, Lopez AM (2003) Effects of estrogen plus progestin on gynecologic cancers and associated diagnostic procedures: the Women's Health Initiative randomized trial. JAMA 290 (13): 1739–1748
Beral V, Bull D, Green J, Reeves G (2007) Ovarian cancer and hormone replacement therapy in the Million Women Study. Lancet 369 (9574): 1703–1710
Danforth KN, Tworoger SS, Hecht JL, Rosner BA, Colditz GA, Hankinson SE (2007) A prospective study of postmenopausal hormone use and ovarian cancer risk. Br J Cancer 96 (1): 151–156
Greiser CM, Greiser EM, Doren M (2007) Menopausal hormone therapy and risk of ovarian cancer: systematic review and meta-analysis. Hum Reprod Update 13 (5): 453–463
Hildebrand JS, Gapstur SM, Feigelson HS, Teras LR, Thun MJ, Patel AV (2010) Postmenopausal hormone use and incident ovarian cancer: Associations differ by regimen. Int J Cancer 127 (12): 2928–2935
Lacey JV, Brinton LA, Leitzmann MF, Mouw T, Hollenbeck A, Schatzkin A, Hartge P (2006) Menopausal hormone therapy and ovarian cancer risk in the National Institutes of Health-AARP Diet and Health Study Cohort. J Natl Cancer Inst 98 (19): 1397–1405
Lacey JV, Mink PJ, Lubin JH, Sherman ME, Troisi R, Hartge P, Schatzkin A, Schairer C (2002) Menopausal hormone replacement therapy and risk of ovarian cancer. JAMA 288 (3): 334–341
Merrill RM (2001) Prevalence corrected hysterectomy rates and probabilities in Utah. Ann Epidemiol 11 (2): 127–135
Michaud DS, Midthune D, Hermansen S, Leitzmann M, Harlan LC, Kipnis V, Schatzkin A (2005) Comparison of cancer registry case ascertainment with SEER estimates and self-reporting in a subset of the NIH-AARP Diet and Health Study. J Reg Manag 32: 70–75
Moorman PG, Schildkraut JM, Calingaert B, Halabi S, Berchuck A (2005) Menopausal hormones and risk of ovarian cancer. Am J Obstet Gynecol 193 (1): 76–82
Morch LS, Lokkegaard E, Andreasen AH, Kjaer SK, Lidegaard O (2012) Hormone Therapy and Different Ovarian Cancers: a National Cohort Study. Am J Epidemiol 175 (12): 1234–1242
Morch LS, Lokkegaard E, Andreasen AH, Kruger-Kjaer S, Lidegaard O (2009) Hormone therapy and ovarian cancer. JAMA 302 (3): 298–305
Pearce CL, Chung K, Pike MC, Wu AH (2009) Increased ovarian cancer risk associated with menopausal estrogen therapy is reduced by adding a progestin. Cancer 115 (3): 531–539
Pike MC, Spicer DV (2000) Hormonal contraception and chemoprevention of female cancers. Endocr Relat Cancer 7 (2): 73–83
Purdie D, Green A, Bain C, Siskind V, Ward B, Hacker N, Quinn M, Wright G, Russell P, Susil B (1995) Reproductive and other factors and risk of epithelial ovarian cancer: an Australian case-control study. Survey of Women's Health Study Group. Int J Cancer 62 (6): 678–684
Riman T, Dickman PW, Nilsson S, Correia N, Nordlinder H, Magnusson CM, Weiderpass E, Persson IR (2002) Hormone replacement therapy and the risk of invasive epithelial ovarian cancer in Swedish women. J Natl Cancer Inst 94 (7): 497–504
Risch HA, Marrett LD, Jain M, Howe GR (1996) Differences in risk factors for epithelial ovarian cancer by histologic type. Results of a case-control study. Am J Epidemiol 144 (4): 363–372
Rodriguez C, Patel AV, Calle EE, Jacob EJ, Thun MJ (2001) Estrogen replacement therapy and ovarian cancer mortality in a large prospective study of US women. JAMA 285 (11): 1460–1465
Rossing MA, Cushing-Haugen KL, Wicklund KG, Doherty JA, Weiss NS (2007) Menopausal hormone therapy and risk of epithelial ovarian cancer. Cancer Epidemiol Biomarkers Prev 16 (12): 2548–2556
Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, Ockene J (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women's Health Initiative randomized controlled trial. JAMA 288 (3): 321–333
Santen RJ, Allred DC, Ardoin SP, Archer DF, Boyd N, Braunstein GD, Burger HG, Colditz GA, Davis SR, Gambacciani M, Gower BA, Henderson VW, Jarjour WN, Karas RH, Kleerekoper M, Lobo RA, Manson JE, Marsden J, Martin KA, Martin L, Pinkerton JV, Rubinow DR, Teede H, Thiboutot DM, Utian WH (2010) Postmenopausal hormone therapy: an Endocrine Society scientific statement. J Clin Endocrinol Metab 95 (7 Suppl 1): s1–s66
Schatzkin A, Subar AF, Thompson FE, Harlan LC, Tangrea J, Hollenbeck AR, Hurwitz PE, Coyle L, Schussler N, Michaud DS, Freedman LS, Brown CC, Midthune D, Kipnis V (2001) Design and serendipity in establishing a large cohort with wide dietary intake distributions: the National Institutes of Health-American Association of Retired Persons Diet and Health Study. Am J Epidemiol 154 (12): 1119–1125
Schildkraut JM, Calingaert B, Marchbanks PA, Moorman PG, Rodriguez GC (2002) Impact of progestin and estrogen potency in oral contraceptives on ovarian cancer risk. J Natl Cancer Inst 94 (1): 32–38
Tsilidis KK, Allen NE, Key TJ, Dossus L, Kaaks R, Bakken K, Lund E, Fournier A, Dahm CC, Overvad K, Hansen L, Tjonneland A, Rinaldi S, Romieu I, Boutron-Ruault MC, Clavel-Chapelon F, Lukanova A, Boeing H, Schutze M, Benetou V, Palli D, Berrino F, Galasso R, Tumino R, Sacerdote C, Bueno-de-Mesquita HB, van Duijnhoven FJ, Braem MG, Onland-Moret NC, Gram IT, Rodriguez L, Duell EJ, Sanchez MJ, Huerta JM, Ardanaz E, Amiano P, Khaw KT, Wareham N, Riboli E (2011) Menopausal hormone therapy and risk of ovarian cancer in the European prospective investigation into cancer and nutrition. Cancer Causes Control 22 (8): 1075–1084
Yang HP, Trabert B, Murphy MA, Sherman ME, Sampson JN, Brinton LA, Hartge P, Hollenbeck A, Park Y, Wentzensen N (2012) Ovarian cancer risk factors by histologic subtypes in the NIH-AARP diet and health study. Int J Cancer 131 (4): 938–949
Acknowledgements
We are indebted to the participants in the NIH-AARP Diet and Health Study for their outstanding cooperation. We also thank Sigurd Hermansen and Kerry Grace Morrissey from Westat for study outcomes ascertainment and management and Leslie Carroll at Information Management Services for data support and analysis. This research was supported (in part) by the Intramural Research Programme of the NIH, National Cancer Institute. Cancer incidence data from the Atlanta metropolitan area were collected by the Georgia Center for Cancer Statistics, Department of Epidemiology, Rollins School of Public Health, Emory University. Cancer incidence data from California were collected by the California Department of Health Services, Cancer Surveillance Section. Cancer incidence data from the Detroit metropolitan area were collected by the Michigan Cancer Surveillance Programme, Community Health Administration, State of Michigan. The Florida cancer incidence data used in this report were collected by the Florida Cancer Data System (FCDC) under contract with the Florida Department of Health (FDOH). The views expressed herein are solely those of the authors and do not necessarily reflect those of the FCDC or FDOH. Cancer incidence data from Louisiana were collected by the Louisiana Tumour Registry, Louisiana State University Medical Centre in New Orleans. Cancer incidence data from New Jersey were collected by the New Jersey State Cancer Registry, Cancer Epidemiology Services, New Jersey State Department of Health and Senior Services. Cancer incidence data from North Carolina were collected by the North Carolina Central Cancer Registry. Cancer incidence data from Pennsylvania were supplied by the Division of Health Statistics and Research, Pennsylvania Department of Health, Harrisburg, Pennsylvania. The Pennsylvania Department of Health specifically disclaims responsibility for any analyses, interpretations or conclusions. Cancer incidence data from Arizona were collected by the Arizona Cancer Registry, Division of Public Health Services, Arizona Department of Health Services. Cancer incidence data from Texas were collected by the Texas Cancer Registry, Cancer Epidemiology and Surveillance Branch, Texas Department of State Health Services. Cancer incidence data from Nevada were collected by the Nevada Central Cancer Registry, Centre for Health Data and Research, Bureau of Health Planning and Statistics, State Health Division, State of Nevada Department of Health and Human Services.
Author information
Authors and Affiliations
Corresponding author
Additional information
In memory of Dr Arthur Schatzkin, visionary investigator who founded the NIH-AARP Diet and Health Study.
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Trabert, B., Wentzensen, N., Yang, H. et al. Ovarian cancer and menopausal hormone therapy in the NIH-AARP diet and health study. Br J Cancer 107, 1181–1187 (2012). https://doi.org/10.1038/bjc.2012.397
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.397
Keywords
This article is cited by
-
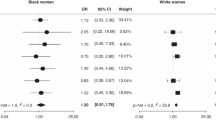
Menopausal hormone therapy use and risk of ovarian cancer by race: the ovarian cancer in women of African ancestry consortium
British Journal of Cancer (2023)
-
Circulating estrogens and postmenopausal ovarian and endometrial cancer risk among current hormone users in the Women’s Health Initiative Observational Study
Cancer Causes & Control (2019)
-
Ovarian Cancer in Women of African Ancestry (OCWAA) consortium: a resource of harmonized data from eight epidemiologic studies of African American and white women
Cancer Causes & Control (2019)
-
Corni fructus ameliorates menopause symptom in 4-vinylcyclohexene diepoxide
Molecular & Cellular Toxicology (2018)
-
Menopausale Hormontherapie und Krebsrisiko
Der Gynäkologe (2017)