Abstract
Background:
The aim of this study was to compare mitotic count (MC) and Ki-67 proliferation index as prognostic markers in pancreatic and midgut neuroendocrine neoplasms (NENs).
Methods:
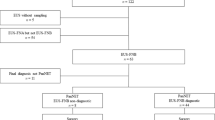
Two hundred eighty-five patients with metastatic NENs were recruited. Concordance between histological grade according to either Ki-67 or MC as defined by the European Neuroendocrine Tumour Society guidelines was assessed and the prognostic significance of Ki-67 or MC were evaluated.
Results:
There was a discrepancy of 44 and 38% in grade assignment when using Ki-67 or MC in pancreatic and midgut NENs, respectively. In multivariate analysis, grade using Ki-67, but not MC, was a significant prognostic factor in determining overall survival (hazard ratios: midgut G2 2.34, G3 15.1, pancreas G2 2.08, G3 11.3). The prognostic value of Ki-67 was improved using a modified classification (hazard ratios: midgut G2 3.02, for G3 22.1, pancreas G2 5.97, G3 33.8).
Conclusion:
There is a lack of concordance between Ki-67 and MC in assigning tumour grade. Grade according to Ki-67 was a better prognostic marker than MC for metastatic pancreatic and midgut NENs. We suggest that Ki-67 alone should be used for grading pancreatic and midgut NENs and that the current threshold for classifying G1/G2 tumours should be revised from 2 to 5%.
Similar content being viewed by others
Main
Neuroendocrine neoplasms (NENs) are uncommon, heterogeneous tumours with an increasing incidence and prevalence. Most commonly arising from the gastrointestinal tract, gastroenteropancreatic NENs (GEP-NENs) have a variable prognosis, with survival ranging from 6 months to more than 20 years (Yao et al, 2008). As the therapeutic options continue to expand it is increasingly important to define robust prognostic markers to inform clinical decision making (Khan and Caplin, 2011). The Ki-67 proliferation index and mitotic count (MC) have proved to be the most useful prognostic histological markers, and have been incorporated into international grading systems (Ramage et al, 2012). However, there is a lack of consensus regarding the best marker and the most appropriate cutoff to define grade. Although some groups have used Ki-67 proliferation index, identifying a cutoff of 2% to define low and intermediate groups in midgut and pancreatic NENs (Furlan et al, 2004; Panzuto et al, 2005; Rorstad, 2005; Tomassetti et al, 2005), other groups have subdivided well-differentiated NENs into low and intermediate-grade based on MC (Hochwald et al, 2002; Van Eeden et al, 2002).
The European Neuroendocrine Tumour Society (ENETS) has proposed a three-tiered grading system for foregut, midgut and hindgut NENs using either Ki-67 proliferation index or MC, based on findings by Rindi et al (2006, 2007). This system has recently been adopted by the WHO (World Health Organisation) classification of 2010 as well as the AJCC/UICC (American Joint Committee on Cancer/Union for International Cancer Control) classification. Although the ENETS grading system has been validated (Pape et al, 2008b; Jann et al, 2011), and adopted into routine practice, definitive data do not exist to determine whether the cutoff values used to distinguish the three grades are optimal and some authors still question the use of Ki-67 proliferation index as an independent prognostic indicator (Durante et al, 2009).
The histopathological grading of GEP-NENs according to ENETs proposal suggests equivalence between grade according to Ki-67 index and grade according to MC, but in our experience, the two indices may provide conflicting information about grade. To date, there has been no study systematically investigating the concordance between Ki-67 index and MC when using the ENETS grading system. We therefore investigated the agreement between grade according to Ki-67 index and grade according to MC in midgut and pancreatic NENs. Additionally, we explored the prognostic value of each in terms of overall survival (OS) in order to assess the validity of the three-tiered classification.
Materials and Methods
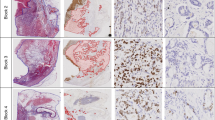
Patients with metastatic pancreatic and midgut NENs diagnosed between January 1989 and October 2009 were identified from a database at the Neuroendocrine Tumour Unit, Royal Free Hospital. Patients had both a diagnosis of NEN (based on morphology and immunohistochemistry) and had stage IV disease according to the TNM ENETS criteria based on the presence of distant metastatic disease measurable by RECIST 1.1 (Eisenhauer et al, 2009). Diagnostic tissue from biopsy or surgical specimens before commencement of treatment were fixed in formalin and embedded in paraffin. Sections were reviewed by a pathologist with expertise in NENs to establish diagnosis, degree of differentiation (well or poorly differentiated) and MC according to ENETS criteria. On light microscopy, mitotic figures (per 10 high power fields (HPF)) were evaluated in at least 40 fields of highest mitotic activity.
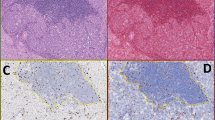
Immunohistochemistry
Sections from tumours were submitted for immunohistochemical examination to evaluate Ki-67 proliferation index. Three micron sections of tumour tissue were deparaffinised in xylene, rehydrated in graded alcohols with endogenous peroxidase blocked with 0.5% H2O2 in methanol for 10 min. Thereafter, sections were subjected to 3-min heat-mediated antigen retrieval. Immunohistochemical staining was performed with the NovoLink Polymer detection system (Novocastra, Newcastle-upon-Tyne, UK). Sections were incubated with MIB-1 antibody detecting Ki-67 (DAKO, Cambridgeshire, UK) at a dilution of 1 : 200 for 1 h at room temperature, post-primary block for 30 min, followed by Novolink polymer for 30 min. Reaction products were visualised with application of diaminobenzidine substrate chromogen solution. Slides were counterstained in haematoxylin and mounted. The Ki-67 proliferation index was determined by assessing the percentage of positively staining tumour cell nuclei in 2000 neoplastic cells in areas with highest degree of nuclear labelling where possible (Rindi et al, 2006, 2007). Positive non-tumour cells (e.g., endothelial cells, intratumoural lymphocytes) were excluded from analysis. Histopathological grading was assigned to each case according to the classification proposed by the European Neuroendocrine Tumours Society (ENETS) (Rindi et al, 2006, 2007) as in Table 1. Each case was assigned two grades, one grade according to Ki-67 proliferation index and one grade according to MC. Cases were also classified into grades with according to the parameters described by Scarpa et al (2010); G1: Ki-67 ⩽5%, G2: Ki-67>5% and ⩽20%, G3: Ki-67>20%.
Inter-observer error
To assess inter-observer error, 44 H&E stained sections (for MC) and 44 sections stained for Ki-67 were independently reviewed by a second expert pathologist blind to initial assessments. Sections were chosen to distribute low- and intermediate-grades evenly, with a small proportion of high-grade sections, reflecting clinical practice. MC and Ki-67 were assessed as above with grade assigned using both indices.
Clinical data
Pre-treatment biochemical data obtained at the time of diagnosis included plasma Chromogranin A (CgA), and for midgut NENs, 24-h urinary 5-hydroxy-indoleacetic acid (5-HIAA). Overall survival was recorded as the time from diagnosis to the patient’s death.
Statistical analyses
Statistical analyses were performed using SPSS for Windows (SPSS Inc., Chicago, IL, USA) where P-values of <0.05 were considered significant. Pancreatic and midgut NENs were analysed separately. Correlation between grades assigned by Ki-67 and MC was assessed using non-parametric correlation. Agreement between grades and inter-observer agreement was assessed with weighted kappas (κW). Survival was estimated using Kaplan–Meier methodology, stratified by both grading systems, with differences in survival between groups analysed by log-rank testing. Potential biomarkers were analysed for prognostic significance. Grading assigned by either Ki-67 and MC were analysed as categorical variables. As CgA was not normally distributed, even when log transformed, it was analysed in two groups: >and ⩽2 times the upper limit of normal (120 pmol l−1)(Oberg et al, 2011). Urinary 5-HIAA was analysed in two groups: >and ⩽ the median (Formica et al, 2007). Cox-proportional hazards regression analysis was used to obtain univariate and multivariate hazard ratios for OS. Those variables found to be significant on univariate analyses were incorporated into the multivariate models with a significance level of P<0.05.
Results
Patient characteristics
A total of 285 cases of NENs, 144 (51%) of pancreatic origin and 141 (49%) of midgut origin were identified. Of these, 131 and 136, respectively, had complete data and were included in the analysis. Patient characteristics and therapy administered are shown in Table 2. Tumour tissue was obtained from biopsy material in 84 (64%) of those with pancreatic NENs and 95 (70%) of those with midgut primary NENs. The remainder had tissue available from surgical resections.
Inter-observer error
Inter-observer error was assessed between grade assigned according to MCs or Ki-67 index. The matrices of this agreement are shown in Table 3. The κW for agreement on grade assigned by MC was 0.83 (95% CI: 0.68–0.99) and for grade assigned by Ki-67 was 0.87 (95% CI: 0.74–1.00). The four discrepancies were between G1 and G2.
Comparison of grade assigned by MC and Ki-67 proliferation index
Of 267 cases, 242 were well-differentiated and 25 poorly differentiated NENs. Of the 21 pancreatic NENs that were poorly differentiated, one was G2 and 20 G3 according to Ki-67; one G1, 11 G2 and 9 G3 according to MC. Four midgut NENs were poorly differentiated, all designated as G3 according to Ki-67 and all G2 according to MC.
There was a moderate correlation between absolute Ki-67 index and MCs (ρ=0.65 P<0.001 for pancreatic and ρ=0.59 P<0.001 for midgut NENs) (Figure 1). There was agreement between grade assigned by Ki-67 and grade assigned by MC in 74 of 131 (56%) pancreatic NENs; and in 84 of 136 (62%) of midgut NENs (Table 4). This corresponds to a discordance of 44% and 38%, respectively, with a κW of 0.41 (95% CI: 0.30–0.53) and 0.35 (95% CI: 0.22–0.48), respectively. This equates to moderate and fair agreement, when assigning grade with these indices. When surgical and biopsy specimens were compared for agreement between grade using Ki-67 and MC, there was little difference with κW 0.42 (0.26–0.59) and κW 0.39 (0.29–0.49), respectively.
Survival
Patients were followed up for a median of 46 months (pancreatic) and 42 months (midgut). Survival data are shown in Table 5. Kaplan–Meier survival curves for pancreatic and midgut NENs are shown in Figure 2. The three-tiered grading systems with either Ki-67 or MCs were able to distinguish significantly different prognostic groups in pancreatic NENs. When analysing midgut NENs, however, only grade according to Ki-67 was able to distinguish the three-tiered prognostically different groups in terms OS. Grading using MC was not able to distinguish G1 from G2 tumours.
Univariate and multivariate analyses are shown in Table 6. Higher grade according to Ki-67 was an independent prognostic indicator of OS in both pancreatic and midgut NENs, whereas grade using MC was not. The only other significant variables were CgA >120 pmol l−1, which was associated with shorter OS; and age in pancreatic NENs.
Alternative thresholds for grade classification
Tumour grades were reassigned with alternative cutoffs for Ki-67 suggested by Scarpa et al (2010) for Ki-67. In this classification grades are defined as follows: G1: Ki-67⩽5%, G2: Ki-67>5% and ⩽20%, G3: Ki-67>20%. Univariate analyses with survival curves for this alternative grading classification are shown in Figure 3, which demonstrates that that this grading system was able to distinguish three prognostically different groups. Multivariate analyses confirmed that grade according to ki-67 was an independent prognostic factor (Table 7). The hazard ratios using the alternative threshold were higher than those using the ENETS thresholds suggesting that the alternative thresholds may be more discriminatory than those of ENETS. Chromogranin A >120 pmol l−1 was also prognostic.
Survival curves demonstrating OS in (A) pancreatic NENs and (B) midgut NENs with grade (G1, G2 and G3) according to Ki-67 classifications according to Scarpa et al (2010).
Discussion
We found a correlation between absolute Ki-67 index and MC, which is to be expected as both are markers of cell division and measure proliferation. However, we demonstrate when using these indices to assign grade, there was 44 and 38% discordance in pancreatic and midgut NENs; moderate and poor agreement defined by κW. Using ENETS guidelines, either MC or Ki-67 can be used to assign grade but the lack of concordance may result in different classification of the same tumour depending on which parameter is used. This could result in different patient management as G3 tumours are usually treated with chemotherapy first line.
Our findings conflict with findings by Strosberg et al (2009), who demonstrated complete agreement between grade by Ki-67 and MC. However, they used a two-tiered rather than three-tiered grading system, which is a simplification of the ENETS grading classification. A recent study compared methods of assessing proliferation: ‘hotspot’ Ki-67 assessment in one field; field average over 10 consecutive fields using digital imaging analysis; and MC (Goodell et al, 2012). Although they highlighted discordance in grade assignment in a small sample of pancreatic NENs, comparing those methods did not reflect current clinical practice, and there was no prognostic evaluation or survival data in the study.
We have assessed OS rather than disease specific survival and this is a potential limitation. However, others have shown, in this patient group, that non-cancer related mortality is 2.6% (Scarpa et al, 2010) and our survival data for metastatic pancreatic NENs appears to be comparable to previous series with 5- and 10-year survival rates of 59% and 36%, respectively (median follow-up 54 months). A Swedish series of 324 pancreatic NENs had 5- and 10-year survival of 64 and 44% (median follow-up 54 months), but only 180/324 in that series had metastatic disease (Ekeblad et al, 2008). A more recent series has reported survival rates 35% and 17%, respectively, in a metastatic subgroup (Scarpa et al, 2010).
For our series of metastatic midgut NENS (1989–2009), we report a 5-year OS of 61.3%, which compares with results of the Surveillance, Epidemiology and End Results (SEER) registry data (1992–1999) in which the overall 5-year survival of midgut NENs was 61%, and 50% for those with metastatic disease(Modlin et al, 2003). Although a higher 5-year survival rate was quoted with more recent SEER (2004–2007) data for midgut NENs (68%), a breakdown by stage was not given (Lawrence et al, 2011). A higher 5-year survival rate (83%) was reported in a recent European series but a number of slow growing hindgut NENs were included (Jann et al, 2011).
AS there was a lack of concordance between grade assigned by Ki-67 and MC, we investigated which index was more clinically valuable by analysing the prognostic value of each. In pancreatic NENs, although grade according to MC was prognostic on univariate analyses, it was not an independent prognostic factor on multivariate analyses and was not able to distinguish G1 from G2 in terms of OS. Only grade according to Ki-67, and not MC, was prognostic in multivariate analyses in both pancreatic and midgut NENs. Baseline CgA >120 pmol l−1 was the only other risk factor, apart from age, found to be associated with worse OS on multivariate analysis, and only in metastatic pancreatic NENs. This suggests that grade according Ki-67 is a better prognostic variable than grade according to MC. One of the reasons for this finding may be that MC is affected by pre-analytical or analytical factors such as delay in tissue fixation (Donhuijsen et al, 1990; Bergers et al, 1997), problems in identification of a mitotic figure (Baak et al, 1989), selection of measurement area (Paulus et al, 1984; Verhoeven et al, 1990), or assessment of mitotic cells in relation to tumour tissue in the sample (Woosley, 1991). The discrepancy in grading could also arise from the fact that the mitotic phase represents the smallest portion of the cell cycle and Ki-67, which detects cells from mid-G1 through S and G2 phases, will detect proliferating cells that do not show mitotic figures.
The ENETS guidelines stipulate that Ki-67 is assessed in areas of highest proliferative activity (hot spots), whereas mitoses are expressed by 10 separate HPF over an average of 40 HPF and many fields may not have any proliferative activity, contributing to the discrepancy. Also, in NENs, Ki-67 assessment has been standardised to 2000 cells with highest activity, whereas the consensus in breast cancer is 500–1000 cells and assessment of ‘hot spots’ being less consistent (Dowsett et al, 2011).
According to ENETS grading criteria, when the amount of tumour tissue is limited such as in a core biopsy, it is not possible to perform an accurate MC as it does not contain the recommended 40 microscopic fields of tumour. In these cases, Ki-67 may provide a more accurate proliferative index, although the MC can be readily performed on the routine H&E slides and the Ki-67 index requires the performance of an immunostain.
It is recognised that the proliferative rate with Ki-67 is not always uniform throughout a given NEN. Whether the Ki-67 index obtained from a core biopsy, which may contain the recommended 2000 cells, represents the whole tumour has been investigated by Yang et al (2011). Despite the intratumoural heterogeneity in Ki-67 labelling found in nearly half of metastatic well-differentiated NENs to the liver, Yang demonstrated that Ki-67 grading based on virtual biopsies had significant prognostic value similar to that using whole slides. Thus, Yang’s data support Ki-67 staining of core biopsies as an adequately reliable method of proliferation assessment for prognosis.
The distinction between G1 and G2 NENs is based on a very subtle difference in the proliferative rate, which may not be optimal grading threshold and hence accountable for the discrepancy in grading and prognostic value. The 2% threshold for Ki-67 was derived from previous data (Furlan et al, 2004; Panzuto et al, 2005; Rorstad, 2005; Tomassetti et al, 2005). However, the thresholds may not apply to all populations of NENs studied, as there is heterogeneity in terms of primary tumour, stage of disease and subsequent treatments among studies. We have separated midgut and pancreatic NENs in the analysis and have also focussed on cases with metastatic disease as this population constitutes the majority of clinical practice.
The identification and definition of optimal cut-points to distinguish the three grades remains the subject of debate. The three-tiered ENETS grading system has been validated in retrospective series in foregut (Pape et al, 2008b), midgut and hindgut NENs (Jann et al, 2011) with most using Ki-67. More recently, Scarpa et al (2010) found the Ki-67 cutoff of 2% was unable to distinguish G1 and G2 prognostically in a multivariate analysis of 237 pancreatic NENs . However a cut of 5%, as originally suggested Pelosi et al (1996), was found to be more discriminatory. Pape et al (2008a) also reported that cutoffs of 5 and 10% were prognostic in a heterogeneous series of 239 NENs.
Here, we also investigated thresholds of 5 and 20% for Ki-67 as used by Scarpa et al (2010) for both midgut and pancreatic NENs. In both midgut and pancreatic NENs, on univariate and multivariate analyses, Ki-67 was again confirmed as an independent prognostic indicator. Raising the cutoff between G1 and G2 to 5% resulted in better differentiation of G1 from G2 NENs in terms of OS with hazard ratios higher than with ENETS thresholds, suggesting that these alternative thresholds may be more optimal when prognosticating.
The guidelines for the management of NENs continue to evolve with some discrepancy between the ENETS and AJCC/UICC staging systems. In Europe, the TNM staging system suggested by ENETS has been adopted, whereas the recent 2010 WHO guidelines suggest the AJCC/UICC system should be used; however, it also mentions the ENETS TNM system and proposes a grading system resembling that of ENETS, based on Ki-67 or MC (Bosman et al, 2010). In 2009, the AJCC/UICC introduced TNM staging of gastrointestinal and pancreatic NENs, which differ in several aspects from the ENETS guidelines but do concede that Ki-67 is a useful prognostic marker (Sobin et al, 2009). In 2010, the NANETS provided guidelines for clinical management and refer to diagnosis by either ENETS and AJCC/UICC systems, but states that it should be indicated which is used (Klimstra et al, 2010; Kulke et al, 2010; Strosberg et al, 2010; Vinik et al, 2010a, 2010b).
Here, we have validated the grading system proposed by ENETS guidelines in patients with NENs with metastatic disease, a more homogenous group than the large published pathology data sets. As the majority of patients present with metastatic NENs at the time of diagnosis, this is a clinically relevant population. Our data suggest that despite the ENETS grading guidelines, one should not assume agreement between Ki-67 and MC, which can impact on therapeutic decisions. We also conclude that grade according to Ki-67 is better in predicting prognosis than MC. Furthermore, the alternate grading strata suggested by Scarpa et al (2010) were found to be prognostic in both metastatic pancreatic and midgut NENs and more optimal than ENETS guidelines. In conclusion, as both MC and Ki-67 measure proliferation and MC provides no additional information, future clinical guidelines should define grade in NENs solely with Ki-67.
Change history
14 May 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Baak JP, van Diest PJ, Ariens AT, van Beek MW, Bellot SM, Fijnheer J, van Gorp LH, Kwee WS, Los J, Peterse HC, Ruitenberg HM, Schapers RFM, Schipper MEI, Somsen JG (1989) The Multicenter Morphometric Mammary Carcinoma Project (MMMCP). A nationwide prospective study on reproducibility and prognostic power of routine quantitative assessments in The Netherlands. Pathol Res Pract 185 (5): 664–670
Bergers E, Jannink I, van Diest PI, Cuesta MA, Meyer S, van Mourik JC, Baak JP (1997) The influence of fixation delay on mitotic activity and flow cytometric cell cycle variables. Human Pathol 28 (1): 95–100
Bosman FT, Carneiro F, Hruban RH, Theise ND (2010) WHO Classification of Tumours of the Digestive System. IARC: Lyon
Donhuijsen K, Schmidt U, Hirche H, van Beuningen D, Budach V (1990) Changes in mitotic rate and cell cycle fractions caused by delayed fixation. Human Pathol 21 (7): 709–714
Dowsett M, Nielsen TO, A’Hern R, Bartlett J, Coombes RC, Cuzick J, Ellis M, Henry NL, Hugh JC, Lively T, McShane L, Paik S, Penault-Llorca F, Prudkin L, Regan M, Salter J, Sotiriou C, Smith IE, Viale G, Zujewski JA, Hayes DF (2011) Assessment of ki67 in breast cancer: recommendations from the international ki67 in breast cancer working group. J Natl Cancer Institute 103 (22): 1656–1664
Durante C, Boukheris H, Dromain C, Duvillard P, Leboulleux S, Elias D, de Baere T, Malka D, Lumbroso J, Guigay J, Schlumberger M, Ducreux M, Baudin E (2009) Prognostic factors influencing survival from metastatic (stage IV) gastroenteropancreatic well-differentiated endocrine carcinoma. Endocr Relat Cancer 16 (2): 585–597
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45 (2): 228–247
Ekeblad S, Skogseid B, Dunder K, Oberg K, Eriksson B (2008) Prognostic factors and survival in 324 patients with pancreatic endocrine tumor treated at a single institution. Clin Cancer Res 14 (23): 7798–7803
Formica V, Wotherspoon A, Cunningham D, Norman AR, Sirohi B, Oates J, Chong G (2007) The prognostic role of WHO classification, urinary 5-hydroxyindoleacetic acid and liver function tests in metastatic neuroendocrine carcinomas of the gastroenteropancreatic tract. Br J cancer 96 (8): 1178–1182
Furlan D, Cerutti R, Uccella S, La Rosa S, Rigoli E, Genasetti A, Capella C (2004) Different molecular profiles characterize well-differentiated endocrine tumors and poorly differentiated endocrine carcinomas of the gastroenteropancreatic tract. Clin Cancer Res 10 (3): 947–957
Goodell PP, Krasinskas AM, Davison JM, Hartman DJ (2012) Comparison of methods for proliferative index analysis for grading pancreatic well-differentiated neuroendocrine tumors. Am J Clin Pathol 137 (4): 576–582
Hochwald SN, Zee S, Conlon KC, Colleoni R, Louie O, Brennan MF, Klimstra DS (2002) Prognostic factors in pancreatic endocrine neoplasms: an analysis of 136 cases with a proposal for low-grade and intermediate-grade groups. J Clin Oncol 20 (11): 2633–2642
Jann H, Roll S, Couvelard A, Hentic O, Pavel M, Muller-Nordhorn J, Koch M, Rocken C, Rindi G, Ruszniewski P, Wiedenmann B, Pape UF (2011) Neuroendocrine tumors of midgut and hindgut origin: tumor-node-metastasis classification determines clinical outcome. Cancer 117 (15): 3332–3341
Khan MS, Caplin ME (2011) Therapeutic management of patients with gastroenteropancreatic neuroendocrine tumours. Endocr Relat Cancer 18 (Suppl 1): S53–S74
Klimstra DS, Modlin IR, Coppola D, Lloyd RV, Suster S (2010) The pathologic classification of neuroendocrine tumors: a review of nomenclature, grading, and staging systems. Pancreas 39 (6): 707–712
Kulke MH, Anthony LB, Bushnell DL, de Herder WW, Goldsmith SJ, Klimstra DS, Marx SJ, Pasieka JL, Pommier RF, Yao JC, Jensen RT (2010) NANETS treatment guidelines: well-differentiated neuroendocrine tumors of the stomach and pancreas. Pancreas 39 (6): 735–752
Lawrence B, Gustafsson BI, Chan A, Svejda B, Kidd M, Modlin IM (2011) The epidemiology of gastroenteropancreatic neuroendocrine tumors. Endocrinol Metab Clin North Am 40 (1): 1–18, vii
Modlin IM, Lye KD, Kidd M (2003) A 5-decade analysis of 13 715 carcinoid tumors. Cancer 97 (4): 934–959
Oberg K, Anthony L, Sideris L, Chen LT, Cherfi A, Tsuchihashi Z, Winkler R, de Vries EG (2011) Role of Chromograning A and Neuron-Specific Enolase Biomarkers in Progression-Free Survival (PFS) with Everolimus (EVE) v. Placebo (PC) in Patients with Advanced Neuroendocrine Tumors (pNET): Phase III RADIANT-3 Results. In 8th Annual European Neuroendocrine Tumour Society (ENETS) Conference for the Diagnosis and Management of Neuroendocrine Tumour Disease p C81. Lisbon
Panzuto F, Nasoni S, Falconi M, Corleto VD, Capurso G, Cassetta S, Di Fonzo M, Tornatore V, Milione M, Angeletti S, Cattaruzza MS, Ziparo V, Bordi C, Pederzoli P, Delle Fave G (2005) Prognostic factors and survival in endocrine tumor patients: comparison between gastrointestinal and pancreatic localization. Endocr Relat Cancer 12 (4): 1083–1092
Pape UF, Berndt U, Muller-Nordhorn J, Bohmig M, Roll S, Koch M, Willich SN, Wiedenmann B (2008a) Prognostic factors of long-term outcome in gastroenteropancreatic neuroendocrine tumours. Endocr Relat Cancer 15 (4): 1083–1097
Pape UF, Jann H, Muller-Nordhorn J, Bockelbrink A, Berndt U, Willich SN, Koch M, Rocken C, Rindi G, Wiedenmann B (2008b) Prognostic relevance of a novel TNM classification system for upper gastroenteropancreatic neuroendocrine tumors. Cancer 113 (2): 256–265
Paulus G, Hong LX, Atassi G, Buyssens N (1984) Regional variations in proliferation rate and degree of differentiation in B16 melanomas. Virchows Arch B Cell Pathol Incl Mol Pathol 46 (1–2): 43–52
Pelosi G, Bresaola E, Bogina G, Pasini F, Rodella S, Castelli P, Iacono C, Serio G, Zamboni G (1996) Endocrine tumors of the pancreas: Ki-67 immunoreactivity on paraffin sections is an independent predictor for malignancy: a comparative study with proliferating-cell nuclear antigen and progesterone receptor protein immunostaining, mitotic index, and other clinicopathologic variables. Human Pathol 27 (11): 1124–1134
Ramage JK, Ahmed A, Ardill J, Bax N, Breen DJ, Caplin ME, Corrie P, Davar J, Davies AH, Lewington V, Meyer T, Newell-Price J, Poston G, Reed N, Rockall A, Steward W, Thakker RV, Toubanakis C, Valle J, Verbeke C, Grossman AB (2012) Guidelines for the management of gastroenteropancreatic neuroendocrine (including carcinoid) tumours (NETs). Gut 61 (1): 6–32
Rindi G, Kloppel G, Alhman H, Caplin M, Couvelard A, de Herder WW, Erikssson B, Falchetti A, Falconi M, Komminoth P, Korner M, Lopes JM, McNicol AM, Nilsson O, Perren A, Scarpa A, Scoazec JY, Wiedenmann B (2006) TNM staging of foregut (neuro)endocrine tumors: a consensus proposal including a grading system. Virchows Arch 449 (4): 395–401
Rindi G, Kloppel G, Couvelard A, Komminoth P, Korner M, Lopes JM, McNicol AM, Nilsson O, Perren A, Scarpa A, Scoazec JY, Wiedenmann B (2007) TNM staging of midgut and hindgut (neuro) endocrine tumors: a consensus proposal including a grading system. Virchows Arch 451 (4): 757–762
Rorstad O (2005) Prognostic indicators for carcinoid neuroendocrine tumors of the gastrointestinal tract. J Surg Oncol 89 (3): 151–160
Scarpa A, Mantovani W, Capelli P, Beghelli S, Boninsegna L, Bettini R, Panzuto F, Pederzoli P, delle Fave G, Falconi M (2010) Pancreatic endocrine tumors: improved TNM staging and histopathological grading permit a clinically efficient prognostic stratification of patients. Mod Pathol 23 (6): 824–833
Sobin LH, Gospodarowicz MK, Wittekind C (2009) UICC: TNM classification of malignant tumours 7th edn. Wiley-Blackwell: Oxford, UK
Strosberg J, Nasir A, Coppola D, Wick M, Kvols L (2009) Correlation between grade and prognosis in metastatic gastroenteropancreatic neuroendocrine tumors. Human Pathol 40 (9): 1262–1268
Strosberg JR, Coppola D, Klimstra DS, Phan AT, Kulke MH, Wiseman GA, Kvols LK (2010) The NANETS consensus guidelines for the diagnosis and management of poorly differentiated (high-grade) extrapulmonary neuroendocrine carcinomas. Pancreas 39 (6): 799–800
Tomassetti P, Campana D, Piscitelli L, Casadei R, Santini D, Nori F, Morselli-Labate AM, Pezzilli R, Corinaldesi R (2005) Endocrine pancreatic tumors: factors correlated with survival. Ann Oncol 16 (11): 1806–1810
Van Eeden S, Quaedvlieg PF, Taal BG, Offerhaus GJ, Lamers CB, Van Velthuysen ML (2002) Classification of low-grade neuroendocrine tumors of midgut and unknown origin. Human Pathol 33 (11): 1126–1132
Verhoeven D, Bourgeois N, Derde MP, Kaufman L, Buyssens N (1990) Comparison of cell growth in different parts of breast cancers. Histopathology 17 (6): 505–509
Vinik AI, Anthony L, Boudreaux JP, Go VL, O'Dorisio TM, Ruszniewski P, Woltering EA (2010a) Neuroendocrine tumors: a critical appraisal of management strategies. Pancreas 39 (6): 801–818
Vinik AI, Woltering EA, Warner RR, Caplin M, O'Dorisio TM, Wiseman GA, Coppola D, Go VL (2010b) NANETS consensus guidelines for the diagnosis of neuroendocrine tumor. Pancreas 39 (6): 713–734
Woosley JT (1991) Measuring cell proliferation. Arch Pathol Lab Med 115 (6): 555–557
Yang Z, Tang LT, Klimstra DS (2011) Effect of tumor heterogeneity on the assessment of Ki67 labeling index in well-differentiated neuroendocrine tumors metastatic to the liver: implications for prognostic stratification. Am J Surg Pathol 35 (6): 853–860
Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE, Abdalla EK, Fleming JB, Vauthey JN, Rashid A, Evans DB (2008) One hundred years after "carcinoid": epidemiology of and prognostic factors for neuroendocrine tumors in 35 825 cases in the United States. J Clin Oncol 26 (18): 3063–3072
Acknowledgements
Deepika Chilkunda and Amelia Jamieson for help in data collection. This work was funded in part by the ‘Quiet Cancer Appeal’ Royal Free Hospital Special Trustees Grant 311, the Ipsen Fund and the UCLH/UCL Department of Health’s NIHR Biomedical Research Centres funding scheme.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
The results have been presented in part at the Digestive Disease Week, 7-10 May 2011, Chicago IL and the 8th Annual ENETS Conference, 9-11 March 2011, Lisbon, Portugal.
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Khan, M., Luong, T., Watkins, J. et al. A comparison of Ki-67 and mitotic count as prognostic markers for metastatic pancreatic and midgut neuroendocrine neoplasms. Br J Cancer 108, 1838–1845 (2013). https://doi.org/10.1038/bjc.2013.156
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.156
Keywords
This article is cited by
-
Radiomics analysis from magnetic resonance imaging in predicting the grade of nonfunctioning pancreatic neuroendocrine tumors: a multicenter study
European Radiology (2023)
-
Prognostic differences in grading and metastatic lymph node pattern in patients with small bowel neuroendocrine tumors
Langenbeck's Archives of Surgery (2023)
-
The long non-coding RNA SAMMSON is essential for uveal melanoma cell survival
Oncogene (2022)
-
Correlation of 68Ga-DOTATATE uptake on PET/CT with pathologic features of cellular proliferation in neuroendocrine neoplasms
Annals of Nuclear Medicine (2021)
-
Improving the accuracy of gastrointestinal neuroendocrine tumor grading with deep learning
Scientific Reports (2020)