Abstract
At least half of all cancer patients will receive radiation therapy. Tumour radioresistance, or the failure to control certain tumours with this treatment, can result in locoregional recurrence; thus there is great interest in understanding the underlying biology and developing strategies to overcome this problem. The expanding investigation of microRNA in cancer suggests that these regulatory factors can influence the DNA damage response, the microenvironment and survival pathways, among other processes, and thereby may affect tumour radioresistance. As microRNA are readily detectable in tumours and biofluids, they hold promise as predictive biomarkers for therapy response and prognosis. This review highlights the current insights on the major ways that microRNA may contribute to tumour radiation response and whether their levels reflect treatment success. We conclude by applying the potential framework of future roles of miR in personalised radiotherapy using prostate cancer clinical management as an example.
Similar content being viewed by others
Introduction
Cancer radiotherapy and tumour radioresistance
The treatment of solid tumours using radiotherapy (RT) is a cornerstone of cancer treatment. This treatment modality is predicated on the idea that cancerous lesions can be destroyed by targeted irradiation, or ionising radiation (IR) exposure, while the surrounding, normal tissue can withstand and recover from IR exposure. Central to this is the ‘therapeutic ratio’, wherein an optimal dose of radiation will provide maximal tumour kill while minimising the risk of significant late toxicity to the patient. However, biological heterogeneity complicates this issue, as certain patient tumours may be inherently more insensitive to a given dose of IR. Failure to control a tumour with a seemingly curative dose would suggest that the tumour is ‘radioresistant’ (i.e., resists radiation treatment), whereas a ‘radiosensitive’ tumour would be controlled. Radioresistance may arise from microenvironmental hypoxia, abnormal intrinsic DNA damage response (DDR) activity, deregulated survival pathway engagement (e.g., ERK or AKT) through constitutive activation of growth factor receptors, or mutations of oncogenes (e.g., KRas) or tumour suppressors (e.g., PTEN) (comprehensively reviewed by Begg et al (2011)). In addition, certain patients have a greater predilection to develop late radiation toxicity. Predictive strategies to determine the radiosensitivity of patient tumours and normal tissue a priori are required to facilitate the future delivery of personalised cancer RT.
Endogenous microRNA (miR) are short non-coding ribonucleic acid molecules whose functions are only recently being appreciated for the important role that they have in radiation response processes through regulation of gene expression. MiRs are emerging as a promising class of biologics pursued for their biomarker and future therapeutic potential in RT. At present, the uses of miR for these purposes are still in their infancy and remain to be rigorously validated in clinical studies. To speculate about the potential clinical implications of miR to RT, we discuss these hypothetical uses in the management of prostate cancer (PCa).
MiR biogenesis
The biological processing and negative transcript regulatory function of miR have been well characterised and reviewed (Ameres and Zamore, 2013). Initially, miR originates in the nucleus as a primary or pri-miR that is transcribed directly from a promoter or from gene introns. The polyadenylated and capped pri-miR is processed by the RNAse III enzyme Drosha into pre-miR, exported to the cytosol and further processed by the RNAse III enzyme Dicer into mature miR. The 19–23-nucleotide RNA duplex is then bound by the RNA-induced silencing complex (RISC) and dissociates into a single-stranded species upon interaction with RISC. The nucleotide sequence of the single-stranded mature miR forms the basis for the recognition of target mRNA transcripts. The RISC subunit Argonaute catalyses the cleavage of mRNA molecules that are perfectly complimentary to the RISC:miR complex, leading to transcript degradation. If the complimentarity of the miR to an mRNA transcript is imperfect, translation is repressed through a variety of mechanisms. As there are about 2000 unique human miR (miRBase.org), with up to hundreds of predicted targets per miR, their role in cellular regulation is widespread.
Review
MiR involvement in the tumour radioresponse
MiR levels are associated with cancer radioresistance, and the topic has been recently reviewed (Metheetrairut and Slack, 2013). Knockdown experiments of the miR biogenesis machinery are used to evaluate a potential role of miR in the cellular response to radiation (or the ‘radioresponse’). For example, Francia et al (2012) discovered that Drosha and Dicer knockdown in cells reduced DDR foci in response to IR, although cell survival beyond impaired cell cycle checkpoints and proliferation was not assessed. Likewise, two other groups have demonstrated that Dicer levels affect the DDR and cell radiosensitivity (Kraemer et al, 2011; Surova et al, 2012). We are now beginning to understand how different miR species downstream of their biogenesis machinery contribute to the observed radiobiological effects. Accordingly, the following sections briefly outline how miR dysregulation in vitro and in vivo contributes to several radiobiological mechanisms. Notwithstanding, endogenous miR dysregulation may be reflective of underlying genetic alterations rather than the driving force behind observed effects. Also, clinical validation for the effects of this dysregulation on RT is currently lacking and will need to be an important focus for translational research. In addition, and even more fundamentally, it should be noted that the causal link between the often quantified outcomes in vitro and in vivo (e.g., apoptosis, proliferation), and human tumour radioresponse has yet to be shown; these outcomes may not truly reflect patient tumour radiosensitivity.
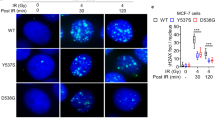
DNA damage response (DDR)
IR induces double-stranded DNA (dsDNA) breaks in genomic DNA. These are sensed and transduced by factors (e.g., ataxia telangiectasia mutated (ATM), histone H2AX phosphorylation) that recruit DNA repair machinery effector protein complexes (e.g., DNA-dependent protein kinases (DNA-PKcs), BRCA1). Failure to restore genomic integrity before mitosis can lead to cell death or malignant transformation.
Several well-studied miRs repress DDR pathway components in cells, which impairs DNA damage sensing or repair and results in increased radiosensitivity. For example, miR-421 and miR-24 downregulate ATM and H2AX, respectively, resulting in increased IR-induced genomic instability and cell death in vitro (Lal et al, 2009; Hu et al, 2010). MiR that target transcripts of fast error-prone (DNA-PKc) or slow error-free (BRCA1) dsDNA break repair genes also radiosensitise cancer cells in vitro and cancer xenografts (Yan et al, 2010; Moskwa et al, 2011). In sum, the underexpression of these miR in cancer cells may enable them to resist radiation damage during RT.
Hypoxic tumour microenvironment
There are several avenues by which the heterogenous hypoxic intratumoural landscapes can protect cancer cells from irradiation. First, the paucity of oxygen impairs the chemical fixation of DNA lesions, leading to the creation of fewer lethal dsDNA breaks. Second, the hypoxic environment can influence radiosensitivity through activation of the hypoxia-inducible factor-1 (HIF-1) pathway and transcription of HIF-1-responsive genes (Meijer et al, 2012). Several hypoxia-induced miR, notably miR-210, can stabilise the HIF-1 complex and enhance radioresistance in vitro (Grosso et al, 2013). Third, it is now recognised that hypoxia can downregulate Dicer in vitro and in vivo, shaping global miR expression to maintain the induction of hypoxia-responsive genes (Ho et al, 2012). Hence, the complex regulatory interface between the hypoxic tumour microenvironment and miR expression may be another source of radioresistance during RT.
Cancer stem cells
Cancer stem cells (CSCs), which reportedly reside in hypoxic niches and possess self-renewal and differentiation potential, may have intrinsic resistance to radiation and chemotherapy (Pajonk et al, 2010). Emerging evidence suggests that miR, such as miR-34a and miR-145, are involved in regulating CSCs. For example, miR-34a negatively regulates human primary tumour-derived CD44+ prostate CSCs, impairing prostate tumour development and metastasis in vivo (Liu et al, 2011). More specifically, miR-145 targets transcription factors (OCT4, SOX2 and KLF4) that are central to maintaining cell stemness (Xu et al, 2009), and is implicated in regulating CSCs in a range of different tumour types, including PCa (Huang et al, 2012). Thus, the involvement of miR in regulating CSC self-renewal capacity is a potential mechanism influencing tumour radioresistance.
Survival pathway alterations
Irradiation-induced DNA damage triggers p53 transcription factor activity that induces the expression of miR-34a (among others) to support cell cycle arrest, senescence or apoptosis (He et al, 2007). However, such miR are often underexpressed in primary human tumours, such as let-7c in PCa (Nadiminty et al, 2012). Several of these also participate in p53 feedback regulatory loops by targeting regulators of p53 or p53 transcripts directly, adding another regulatory layer to the radiation response (Feng et al, 2011).
MiR-dependent alterations in key survival signalling pathways are also common ways cancer cells circumvent irradiation-induced growth arrest and death. For example, miR-21 and miR-95 promote phosphatidylinositol 3 kinase-AKT-pathway-mediated survival by suppressing its direct and indirect negative regulators PTEN and SGPP1, respectively (Meng et al, 2007; Huang et al, 2013). Conversely, miR-9 and let-7 target the NF-κB1 transcript, abrogating the pro-survival effects of NF-κB signalling (Arora et al, 2011). The entanglement of miR in these already well-established tumour survival pathways highlights the opportunity to develop therapeutic strategies aimed at these pathways.
MiR involvement in the normal tissue radioresponse
In contrast to the role of miRs in cancer cells exposed to irradiation, there are few reports detailing how miRs contribute to normal tissue radiation responses. MiRs may be involved in the development of radiation-induced late-onset tissue fibrosis, which can have serious ramifications on cancer patients’ quality of life (Weigel et al, 2014). For example, miR-34a expression was associated with the pathology of irradiation-induced fibrosis in a murine model, and found to target an anti-fibrotic protein transcript (Simone et al, 2014). The most headway has been made characterising the miR landscape of irradiated endothelial cells, where some species show substantial dysregulation following IR exposure, and exert influence over several cellular processes, particularly inflammatory ones (Palayoor et al, 2014). Indeed, the responses of the normal tissue endothelial cell compartment affect the development of acute and late normal tissue toxicities (Stewart et al, 2013; Korpela et al, 2014). In summary, miRs that contribute and correlate with normal tissue radiation toxicity development remain to be better characterised in preclinical models and validated in human subjects.
MiRs as predictive biomarkers of tumour radioresponse
Despite our molecular knowledge of tumour radioresponse, personalised clinical indicators of tumour radioresistance are poorly defined. Positron emission tomography molecular imaging with [18F]-fluorodeoxyglucose or fluoromisonidazole tracers to non-invasively visualise tumour metabolism or hypoxia is a promising approach being evaluated for adaptive RT planning (Bussink et al, 2011). In addition, genetic approaches are being investigated as biomarkers to predict RT treatment outcome. Copy-number alterations of PTEN and c-MYC, or haploinsufficiency of NKX3.1 are prognostic for relapse after PCa RT (Bristow et al, 2014). Recently, a combined tumour hypoxia, genomic instability and genomic subtype signature has demonstrated prognostic significance in men with PCa treated with external beam RT (Lalonde et al, 2014).
The rapidly expanding field of miRs as biomarkers may provide a versatile method of tumour radioresponse prediction and monitoring. In fact, Schwarzenbach et al (2014) review how and why hundreds of circulating miRs have been proposed as biomarkers for human cancer diagnosis and prognostication. The practical utility of miR arises mainly from their relative stability in tissues and their release in stable form into a range of biofluids (e.g., blood, urine). Although individual miR species are subject to decay by newly emerging mechanisms and the purpose of their release remains unknown, they resist decay in biofluids due to their association with Argonaute proteins or encapsulation by vesicles. Even after routine sample tissue processing (e.g., formalin-fixed paraffin-embedded sections) or years of sample storage at −20 °C, miR levels remain readily detectable (Hall et al, 2012). A signature of miR species is amenable to rapid quantification by reverse transcriptase-PCR, whereas a global profile can be quantified by microarray or next-generation sequencing platforms. Although these techniques have high sensitivity and specificity, consensus has not been reached regarding best normalisation protocols or controls to address heterogeneity, let alone biofluid choice or standardised sample-processing methods.
Despite the immense potential clinical utility of miRs, very few studies have investigated this avenue specifically in the context of patients receiving RT. The few available clinical studies offer correlative data and are often statistically underpowered and confounded by other treatments (e.g., concurrent chemotherapy). For example, among a hundred inoperable non-small cell lung cancer (NSCLC) samples from an ongoing trial (NCT01190527), miR-885 and miR-7 were identified as potential serum biomarkers of better overall survival following chemoRT (Bi et al, 2013). In forty advanced rectal cancers, low intratumoural miR-145 expression post chemoRT correlated with poor neoadjuvant chemoRT response (Drebber et al, 2011). In a study not confounded by chemotherapy treatment, Wang et al reported on 15 postoperative RT-resistant and 15 postoperative RT-sensitive patient NSCLC samples. The RT-resistant cases were associated with low intratumoural miR-126 and let-7a levels (among 10 other dysregulated miRs), as well as higher recurrence rates and poorer overall survival when compared with the RT-sensitive cases. Correspondingly, miR-126 overexpression in a lung cancer cell line sensitised them to irradiation-induced apoptosis (Wang et al, 2011). Ke et al found that out of 18 human cervical carcinoma biopsies, the seven that were resistant to RT had high miR-181a expression levels. Likewise, miR-181 overexpression in cell lines and tumour xenografts conferred resistance to IR treatment (Ke et al, 2013).
Indeed, these preliminary studies demonstrate that evaluation of miRs as potential predictors of tumour response to RT are underway, but more non-confounded studies are needed. Statistically rigorous independent validation studies are also critical to confirm the prognostic or predictive value of these emerging findings. Future implementation of miR biomarkers might combine additional genomic and non-invasive imaging approaches (i.e., radiogenomics) to optimise personalised clinical management decisions (Aerts et al, 2014).
MiR-based treatments to increase tumour radiosensitivity
Inoperable melanomas or sarcomas and locally advanced carcinomas are relatively radioresistant when compared with other solid tumours, and are associated with poor patient outcomes. Against the backdrop of chemotherapy or small-molecule tumour radiosensitizers that can exacerbate the side effects of RT in patients, miR-based biologics may be a novel way to combat this resistant phenotype.
Numerous studies have identified endogenous miR species which when expressed, radiosensitise cancer cells in vitro (see the section ‘MiR involvement in the tumour radioresponse’). Some reports further demonstrate radiosensitisation in vivo using cell line xenografts that overexpress particular miR. More clinically relevant investigations would test the delivery of synthetic miR made of oligonucleotides (called miR mimics or morpholinos) as tumour suppressor replacement therapies. For example, one group treated lung cancer xenografts using liposomal nanoparticles loaded with miR-200c mimics, and showed that this sensitised tumours to irradiation by regulating the cell oxidative stress response (Cortez et al, 2014).
Conversely, endogenous miR species that cause radioresistance when expressed could be silenced using synthetic antisense oligonucleotides that bind them (called antagomiR or antimiR). The design of delivery systems that ensure the stability of synthetic miR in the circulation and provide tumour-specific targeting and delivery is integral to translating miR therapy to the clinic (Babar et al, 2012; Cortez et al, 2014). Frank Slack’s group has recently demonstrated the specific targeting of miR-155 in a mouse model of lymphoma using a novel construct that is selective for the acidic tumour microenvironment, highlighting the progress made in this field (Cheng et al, 2014). The feasibility of an antimiR treatment has recently been demonstrated in phase II clinical trials for chronic hepatitis C viral infection in humans (Janssen et al, 2013).
Future clinical implementation of miR for personalised RT
It is becoming clear that miRs are involved in the radiation response, and early data suggest that they may serve as promising predictive and prognostic biomarkers. Thus, miRs may serve as valuable clinical tools in the future to aid clinicians in RT management decisions; here we use localised PCa management to highlight general concepts of potential clinical integration (Figure 1).
The potential utility for miR-predictive signatures in personalising the management of cancer and radiotherapy treatment. Using prostate cancer as an example, validated miR signatures could assist in determining which patients undergoing active surveillance should proceed to definitive treatment. In addition, they could aid in identifying those patients who potentially require additional radiotherapy dose escalation due to a cancer radioresistant signature, or are at increased risk of developing significant normal tissue radiotoxicity.
PCa is the most common cancer diagnosed in men, with the majority of men presenting with localised, low-grade PCa. This group consists of excellent candidates for active surveillance, which carefully follows men to pick up early signs of disease progression prior to proceeding with curative treatment (Klotz et al, 2014). The lack of robust biomarkers that identify the presence of, or the potential to develop, higher-risk disease remains a barrier to widespread adoption of active surveillance (Vesprini et al, 2013). The identification of a miR signature obtained from biofluids that independently predicts the presence of high-grade PCa would therefore enable proper stratification of patients who require upfront treatment. Indeed, one group recently demonstrated that a three-member miR signature present in pre-radical prostatectomy sera showed an AUC of 0.94 in predicting poorer pathological disease compared with the biopsy result, suggesting promise in this approach (Wang et al, 2014).
For men with localised PCa who are not candidates for, or who are adverse to active surveillance, the standard treatment options are radical prostatectomy or RT. Although the RT dose is standardised among patients, isolated local recurrences can occur; even in the modern era of dose escalation, post-treatment biopsies show a 15–20% residual disease rate (Zelefsky et al, 2008). This indicates that the current dose is not optimal for all patients, and implies the failure of RT in eliminating all PCa clonogens in those patients. A miR signature predictive of RT treatment response (i.e., radiosensitivity in the tumour phenotype) a priori would be invaluable in personalising the RT treatment approach. For example, a PCa patient with a radioresistant tumour signature could be treated with a radical prostatectomy, or treated with more ablative doses of radiation using brachytherapy or stereotactic body RT in order to overcome the radioresistance seen with standard RT doses. Biological modifiers of radioresponse could be employed to biologically dose-escalate the tumour (e.g., androgen deprivation therapy, poly (ADP-ribose) polymerase inhibitors to suppress DNA repair, chemotherapy or synthetic miR/antagomirs).
The consequence of escalating RT dose to treat PCa is the increased risk to develop both acute and late toxicity in adjacent normal organs. To potentially predict which patients are at increased risk for normal tissue toxicity, researchers have investigated the use of the patient’s normal cells in functional in vitro assays and performed genomic analyses for single-nucleotide polymorphisms. However, to date, none of these biomarkers have demonstrated highly significant results that would be clinically useful (Barnett et al, 2009). This may be partly due to a lack of a distinct subpopulation of patients at risk of developing significant radiotoxicity, and also the need to account for radiation dose-volume metrics (Bentzen et al, 2010). The expression of serum miRs are rapidly altered in response to IR, and can serve as biomarkers for radiation exposure (Jacob et al, 2013) and potentially for radiotoxicity. Indeed, it was recently reported that miR-210 expression is increased in patients with radiation enteropathy, and repressed by anti-fibrotic therapy (Hamama et al, 2014). However, investigation into miRs as predictors for normal tissue radiotoxicity is still in its infancy; it remains to be determined whether a miR signature can be discovered and validated for prediction of acute or late radiation toxicity in normal tissue. Such a finding could revolutionise the development of personalised RT (e.g., utilising very stringent dose constraints for surrounding normal tissue or avoidance of RT if feasible for patients predicted to be at higher risk for developing radiotoxicity).
The future challenges to adopting miR-based diagnostic, predictive and therapeutic applications for clinical use involve further technical and scientific developments. First, standardised protocols for sample processing, data normalisation and clinical result interpretation require further investigation. Similarly, the optimal biofluid and the choice of an acceptably sensitive and specific detection method remain unidentified. Second, there are great variations in the global expression patterns of miR among different human cancer types, and imperfect overlap of identified signatures even among studies of the same tumour types (Calin and Croce, 2006). Third, genetic and microenvironmental tumour heterogeneity may confound miR expression pattern identification. Proposed miR signatures require rigorous biological and statistical validation in addition to clear definitions of applicable target populations. Future clinical research designs should consider prospectively incorporating pre-treatment tumour biopsies and biofluid collection during and after the RT course to track miR biomarkers in a temporal manner. Molecular elucidation of the radiobiological mechanisms and targets of miR are also critical for the future implementation of synthetic miR or antagomir therapy. Addressing these development and knowledge gap areas will facilitate the development of predictive and prognostic miR biomarkers that will lead us towards personalised RT.
Conclusion
The study of miRs in regulating essential cellular processes is deepening our understanding of the intricacies of tumour radioresistance, and may lead to novel therapeutic strategies employing miR mimics or antagomirs. The expanding interest in miRs as disease biomarkers extends to the realm of personalised RT, where the investigation of miRs in tumours or more readily obtainable biofluid samples is just starting to unfold. We envision that in the clinical setting of low-risk PCa diagnosis and treatment, miR signatures may have the potential to find occult diseases not suitable for surveillance, and identifying patients that are more or less likely to respond to RT, thereby facilitating personalised treatment choices.
References
Aerts HJ, Velazquez ER, Leijenaar RT, Parmar C, Grossmann P, Cavalho S, Bussink J, Monshouwer R, Haibe-Kains B, Rietveld D, Hoebers F, Rietbergen MM, Leemans CR, Dekker A, Quackenbush J, Gillies RJ, Lambin P (2014) Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nat Commun 5: 4006.
Ameres SL, Zamore PD (2013) Diversifying microRNA sequence and function. Nat Rev Mol Cell Biol 14 (8): 475–488.
Arora H, Qureshi R, Jin S, Park A-K, Park W-Y (2011) miR-9 and let-7 g enhance the sensitivity to ionizing radiation by suppression of NF[kappa]B1. Exp Mol Med 43: 298–304.
Babar IA, Cheng CJ, Booth CJ, Liang X, Weidhaas JB, Saltzman WM, Slack FJ (2012) Nanoparticle-based therapy in an in vivo microRNA-155 (miR-155)-dependent mouse model of lymphoma. Proc Natl Acad Sci USA 109 (26): E1695–E1704.
Barnett GC, West CM, Dunning AM, Elliott RM, Coles CE, Pharoah PD, Burnet NG (2009) Normal tissue reactions to radiotherapy: towards tailoring treatment dose by genotype. Nat Rev Cancer 9 (2): 134–142.
Begg AC, Stewart FA, Vens C (2011) Strategies to improve radiotherapy with targeted drugs. Nat Rev Cancer 11 (4): 239–253.
Bentzen SM, Parliament M, Deasy JO, Dicker A, Curran WJ, Williams JP, Rosenstein BS (2010) Biomarkers and surrogate endpoints for normal-tissue effects of radiation therapy: the importance of dose-volume effects. Int J Radiat Oncol Biol Phys 76 (3 Suppl): S145–S150.
Bi N, Schipper MJ, Stanton P, Wang W, Kong F-M (2013) Serum miRNA signature to identify a patient’s resistance to high-dose radiation therapy for unresectable non-small cell lung cancer. J Clin Oncol 31 (Suppl): abstr 7580.
Bristow RG, Berlin A, Dal Pra A (2014) An arranged marriage for precision medicine: hypoxia and genomic assays in localized prostate cancer radiotherapy. Br J Radiol 87 (1035): 20130753.
Bussink J, Kaanders JH, van der Graaf WT, Oyen WJ (2011) PET-CT for radiotherapy treatment planning and response monitoring in solid tumors. Nat Rev Clin Oncol 8 (4): 233–242.
Calin GA, Croce CM (2006) MicroRNA signatures in human cancers. Nat Rev Cancer 6 (11): 857–866.
Cheng CJ, Bahal R, Babar IA, Pincus Z, Barrera F, Liu C, Svoronos A, Braddock DT, Glazer PM, Engelman DM, Saltzman WM, Slack FJ (2014) MicroRNA silencing for cancer therapy targeted to the tumour microenvironment. Nature e-pub ahead of print 17 November 2014; doi:10.1038/nature13905.
Cortez MA, Valdecanas D, Zhang X, Zhan Y, Bhardwaj V, Calin GA, Komaki R, Giri DK, Quini CC, Wolfe T, Peltier HJ, Bader AG, Heymach JV, Meyn RE, Welsh JW (2014) Therapeutic delivery of miR-200c enhances radiosensitivity in lung cancer. Mol Ther 22 (8): 1494–1503.
Drebber U, Lay M, Wedemeyer I, Vallbohmer D, Bollschweiler E, Brabender J, Monig SP, Holscher AH, Dienes HP, Odenthal M (2011) Altered levels of the onco-microRNA 21 and the tumor-supressor microRNAs 143 and 145 in advanced rectal cancer indicate successful neoadjuvant chemoradiotherapy. Int J Oncol 39 (2): 409–415.
Feng Z, Zhang C, Wu R, Hu W (2011) Tumor suppressor p53 meets microRNAs. J Mol Cell Biol 3 (1): 44–50.
Francia S, Michelini F, Saxena A, Tang D, de Hoon M, Anelli V, Mione M, Carninci P, d/'Adda di Fagagna F (2012) Site-specific DICER and DROSHA RNA products control the DNA-damage response. Nature 488 (7410): 231–235.
Grosso S, Doyen J, Parks SK, Bertero T, Paye A, Cardinaud B, Gounon P, Lacas-Gervais S, Noel A, Pouyssegur J, Barbry P, Mazure NM, Mari B (2013) MiR-210 promotes a hypoxic phenotype and increases radioresistance in human lung cancer cell lines. Cell Death Dis 4: e544.
Hall JS, Taylor J, Valentine HR, Irlam JJ, Eustace A, Hoskin PJ, Miller CJ, West CM (2012) Enhanced stability of microRNA expression facilitates classification of FFPE tumour samples exhibiting near total mRNA degradation. Br J Cancer 107 (4): 684–694.
Hamama S, Noman MZ, Gervaz P, Delanian S, Vozenin MC (2014) MiR-210: A potential therapeutic target against radiation-induced enteropathy. Radiother Oncol 111 (2): 219–221.
He L, He X, Lim LP, de Stanchina E, Xuan Z, Liang Y, Xue W, Zender L, Magnus J, Ridzon D, Jackson AL, Linsley PS, Chen C, Lowe SW, Cleary MA, Hannon GJ (2007) A microRNA component of the p53 tumour suppressor network. Nature 447 (7148): 1130–1134.
Ho JJ, Metcalf JL, Yan MS, Turgeon PJ, Wang JJ, Chalsev M, Petruzziello-Pellegrini TN, Tsui AK, He JZ, Dhamko H, Man HS, Robb GB, Teh BT, Ohh M, Marsden PA (2012) Functional importance of Dicer protein in the adaptive cellular response to hypoxia. J Biol Chem 287 (34): 29003–29020.
Hu H, Du L, Nagabayashi G, Seeger RC, Gatti RA (2010) ATM is down-regulated by N-Myc-regulated microRNA-421. Proc Natl Acad Sci USA 107 (4): 1506–1511.
Huang S, Guo W, Tang Y, Ren D, Zou X, Peng X (2012) miR-143 and miR-145 inhibit stem cell characteristics of PC-3 prostate cancer cells. Oncol Rep 28 (5): 1831–1837.
Huang X, Taeb S, Jahangiri S, Emmenegger U, Tran E, Bruce J, Mesci A, Korpela E, Vesprini D, Wong CS, Bristow RG, Liu FF, Liu SK (2013) miRNA-95 mediates radioresistance in tumors by targeting the sphingolipid phosphatase SGPP1. Cancer Res 73 (23): 6972–6986.
Jacob NK, Cooley JV, Yee TN, Jacob J, Alder H, Wickramasinghe P, Maclean KH, Chakravarti A (2013) Identification of sensitive serum microRNA biomarkers for radiation biodosimetry. PLoS One 8 (2): e57603.
Janssen HL, Reesink HW, Lawitz EJ, Zeuzem S, Rodriguez-Torres M, Patel K, van der Meer AJ, Patick AK, Chen A, Zhou Y, Persson R, King BD, Kauppinen S, Levin AA, Hodges MR (2013) Treatment of HCV infection by targeting microRNA. N Engl J Med 368 (18): 1685–1694.
Ke G, Liang L, Yang JM, Huang X, Han D, Huang S, Zhao Y, Zha R, He X, Wu X (2013) MiR-181a confers resistance of cervical cancer to radiation therapy through targeting the pro-apoptotic PRKCD gene. Oncogene 32 (25): 3019–3027.
Klotz L, Vesprini D, Sethukavalan P, Jethava V, Zhang L, Jain S, Yamamoto T, Mamedov A, Loblaw A (2014) Long-term follow-up of a large active surveillance cohort of patients with prostate cancer. J Clin Oncol e-pub ahead of print 15 December 2014.
Korpela E, Vesprini D, Liu SK (2014) Endothelial perturbations and therapeutic strategies in normal tissue radiation damage. Radiat Oncol 9 (1): 266.
Kraemer A, Anastasov N, Angermeier M, Winkler K, Atkinson MJ, Moertl S (2011) MicroRNA-mediated processes are essential for the cellular radiation response. Radiat Res 176 (5): 575–586.
Lal A, Pan Y, Navarro F, Dykxhoorn DM, Moreau L, Meire E, Bentwich Z, Lieberman J, Chowdhury D (2009) miR-24-mediated downregulation of H2AX suppresses DNA repair in terminally differentiated blood cells. Nat Struct Mol Biol 16 (5): 492–498.
Lalonde E, Ishkanian AS, Sykes J, Fraser M, Ross-Adams H, Erho N, Dunning MJ, Halim S, Lamb AD, Moon NC, Zafarana G, Warren AY, Meng X, Thoms J, Grzadkowski MR, Berlin A, Have CL, Ramnarine VR, Yao CQ, Malloff CA, Lam LL, Xie H, Harding NJ, Mak DY, Chu KC, Chong LC, Sendorek DH, P'ng C, Collins CC, Squire JA, Jurisica I, Cooper C, Eeles R, Pintilie M, Dal Pra A, Davicioni E, Lam WL, Milosevic M, Neal DE, van der Kwast T, Boutros PC, Bristow RG (2014) Tumour genomic and microenvironmental heterogeneity for integrated prediction of 5-year biochemical recurrence of prostate cancer: a retrospective cohort study. Lancet Oncol 15 (13): 1521–1532.
Liu C, Kelnar K, Liu B, Chen X, Calhoun-Davis T, Li H, Patrawala L, Yan H, Jeter C, Honorio S, Wiggins JF, Bader AG, Fagin R, Brown D, Tang DG (2011) The microRNA miR-34a inhibits prostate cancer stem cells and metastasis by directly repressing CD44. Nat Med 17 (2): 211–215.
Meijer TW, Kaanders JH, Span PN, Bussink J (2012) Targeting hypoxia, HIF-1, and tumor glucose metabolism to improve radiotherapy efficacy. Clin Cancer Res 18 (20): 5585–5594.
Meng F, Henson R, Wehbe-Janek H, Ghoshal K, Jacob ST, Patel T (2007) MicroRNA-21 regulates expression of the PTEN tumor suppressor gene in human hepatocellular cancer. Gastroenterology 133 (2): 647–658.
Metheetrairut C, Slack FJ (2013) MicroRNAs in the ionizing radiation response and in radiotherapy. Curr Opin Genet Dev 23 (1): 12–19.
Moskwa P, Buffa FM, Pan Y, Panchakshari R, Gottipati P, Muschel RJ, Beech J, Kulshrestha R, Abdelmohsen K, Weinstock DM, Gorospe M, Harris AL, Helleday T, Chowdhury D (2011) miR-182-mediated downregulation of BRCA1 impacts DNA repair and sensitivity to PARP inhibitors. Mol Cell 41 (2): 210–220.
Nadiminty N, Tummala R, Lou W, Zhu Y, Shi XB, Zou JX, Chen H, Zhang J, Chen X, Luo J, deVere White RW, Kung HJ, Evans CP, Gao AC (2012) MicroRNA let-7c is downregulated in prostate cancer and suppresses prostate cancer growth. PLoS One 7 (3): e32832.
Pajonk F, Vlashi E, McBride WH (2010) Radiation resistance of cancer stem cells: the 4 R's of radiobiology revisited. Stem Cells 28 (4): 639–648.
Palayoor ST, John-Aryankalayil M, Makinde AY, Falduto MT, Magnuson SR, Coleman CN (2014) Differential expression of stress and immune response pathway transcripts and miRNAs in normal human endothelial cells subjected to fractionated or single-dose radiation. Mol Cancer Res 12 (7): 1002–1015.
Schwarzenbach H, Nishida N, Calin GA, Pantel K (2014) Clinical relevance of circulating cell-free microRNAs in cancer. Nat Rev Clin Oncol 11 (3): 145–156.
Simone BA, Ly D, Savage JE, Hewitt SM, Dan TD, Ylaya K, Shankavaram U, Lim M, Jin L, Camphausen K, Mitchell JB, Simone NL (2014) microRNA alterations driving acute and late stages of radiation-induced fibrosis in a murine skin model. Int J Radiat Oncol Biol Phys 90 (1): 44–52.
Stewart FA, Seemann I, Hoving S, Russell NS (2013) Understanding radiation-induced cardiovascular damage and strategies for intervention. Clin Oncol (R Coll Radiol) 25 (10): 617–624.
Surova O, Akbar NS, Zhivotovsky B (2012) Knock-down of core proteins regulating microRNA biogenesis has no effect on sensitivity of lung cancer cells to ionizing radiation. PLoS One 7 (3): e33134.
Vesprini D, Liu S, Nam R (2013) Predicting high risk disease using serum and DNA biomarkers. Curr Opin Urol 23 (3): 252–260.
Wang SY, Shiboski S, Belair CD, Cooperberg MR, Simko JP, Stoppler H, Cowan J, Carroll PR, Blelloch R (2014) miR-19, miR-345, miR-519c-5p serum levels predict adverse pathology in prostate cancer patients eligible for active surveillance. PLoS One 9 (6): e98597.
Wang XC, Du LQ, Tian LL, Wu HL, Jiang XY, Zhang H, Li DG, Wang YY, Wu HY, She Y, Liu QF, Fan FY, Meng AM (2011) Expression and function of miRNA in postoperative radiotherapy sensitive and resistant patients of non-small cell lung cancer. Lung Cancer 72 (1): 92–99.
Weigel C, Schmezer P, Plass C, Popanda O (2014) Epigenetics in radiation-induced fibrosis. Oncogene e-pub ahead of print 9 June 2014; doi:10.1038/onc.2014.145.
Xu N, Papagiannakopoulos T, Pan G, Thomson JA, Kosik KS (2009) MicroRNA-145 regulates OCT4, SOX2, and KLF4 and represses pluripotency in human embryonic stem cells. Cell 137 (4): 647–658.
Yan D, Ng WL, Zhang X, Wang P, Zhang Z, Mo YY, Mao H, Hao C, Olson JJ, Curran WJ, Wang Y (2010) Targeting DNA-PKcs and ATM with miR-101 sensitizes tumors to radiation. PLoS One 5 (7): e11397.
Zelefsky MJ, Yamada Y, Fuks Z, Zhang Z, Hunt M, Cahlon O, Park J, Shippy A (2008) Long-term results of conformal radiotherapy for prostate cancer: impact of dose escalation on biochemical tumor control and distant metastases-free survival outcomes. Int J Radiat Oncol Biol Phys 71 (4): 1028–1033.
Acknowledgements
This work was supported by research grants from Prostate Cancer Canada and the Movember Foundation (Grant No. D2013-24, and RS2014-03: 2014 Movember Rising Star in Prostate Cancer Research), the Canada Foundation for Innovation-MEDI ORF, and the Motorcycle Ride for Dad (Huronia branch). EK was supported by the Canada Graduate Scholarships Master’s Award (CIHR CGS-M), the Scace Graduate Fellowship in Prostate Cancer Research and the Paul Starita Graduate Student Fellowship (in molecular prostate cancer research).
Author information
Authors and Affiliations
Corresponding author
PowerPoint slides
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Korpela, E., Vesprini, D. & Liu, S. MicroRNA in radiotherapy: miRage or miRador?. Br J Cancer 112, 777–782 (2015). https://doi.org/10.1038/bjc.2015.6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2015.6
Keywords
This article is cited by
-
Non-canonical function of DGCR8 in DNA double-strand break repair signaling and tumor radioresistance
Nature Communications (2021)
-
MicroRNA: a novel implication for damage and protection against ionizing radiation
Environmental Science and Pollution Research (2021)
-
microRNAs identified in prostate cancer: Correlative studies on response to ionizing radiation
Molecular Cancer (2020)
-
MicroRNA-107 enhances radiosensitivity by suppressing granulin in PC-3 prostate cancer cells
Scientific Reports (2020)
-
miR-410 induces both epithelial–mesenchymal transition and radioresistance through activation of the PI3K/mTOR pathway in non-small cell lung cancer
Signal Transduction and Targeted Therapy (2020)