Abstract
Background:
The objective of this study is to evaluate the safety of fertility-sparing surgery (FSS) for early-stage epithelial ovarian cancer (EOC).
Methods:
A retrospective analysis was performed to identify patients treated for early-stage EOC and to compare the clinical outcomes of patients treated with FSS and radical surgery (RS).
Results:
A total of 1031 patients were treated at two Institutions, 242 with FSS (group A) and 789 with RS (group B). Median duration of follow-up was 11.9 years. At univariate analyses, FSS was associated with decreased risk of relapse (P=0.002) and of tumour-related death (P=0.001). Multivariate analysis did not confirm the independent positive role of FSS neither on relapse-free interval (RFI) nor on cancer-specific survival (CSS). Tumour grade was associated with shorter RFI (P<0.001) and shorter CSS (P=0.001). The type of treatment did not influence CSS or RFI in any grade group. We also found a significant association between low-grade tumours and younger age.
Conclusions:
Fertility-sparing surgery is an adequate treatment for patients with stage I EOC. The clinical outcome of patients with G3 tumours, which is confirmed to be the most important prognostic factor, is not determined by the type of treatment received.
Similar content being viewed by others
Main
Epithelial ovarian cancer (EOC) is a disease typical of postmenopausal age. However, around 10% of EOCs is diagnosed in patients younger than 40 years of age (Duska et al, 1999). The preservation of fertility in these young women has always been a challenging issue for physicians, and because of a constant increase of maternal age at first birth in developed countries during the past 20 years (Mathews and Hamilton, 2009), the request for a conservative treatment by patients is becoming more frequent.
There is a general consensus about the fact that fertility-sparing surgery (FSS) might be offered to patients with borderline, germ cell and stromal ovarian tumours. The recently published ESGO guidelines (Morice et al, 2011) suggested that FSS could be safely offered to patients with FIGO stage IA G1, and that such treatment should be avoided in patients with G3 tumour and with aggressive histological subtypes (as clear cell, anaplastic and small cell) even if it is acknowledged that it is unclear if the worse prognosis of these patients might be related to the ‘natural history’ of the tumour rather than to the conservation of the ovary itself.
The lack of randomised clinical trials has led to the heterogeneity of recommendations of each author about the selection criteria to consider a patient eligible for FSS (Table 1). However, Kajiyama (Kajiyama et al, 2011) recently published the first comparison between radical surgery (RS) and FSS in 572 patients with FIGO stage I EOC, without finding any difference in terms of oncological outcome. He was not conclusive on patients with G3 tumours, but suggested that FSS can be safely proposed to all patients. The same conclusion, regardless FIGO stage and grade, was reported by another retrospective analysis published in 2015 by Ditto (Ditto et al, 2015).
To confirm these findings we compared the relapse-free interval (RFI) and cancer-specific survival (CSS) of patients treated with RS and FSS in patients with stage I EOC. In particular, we investigated whether there are some clinical or tumour-related factors that might influence the prognosis of patients.
Patients and Methods
Women with EOC confined to the ovaries treated at San Gerardo Hospital (Monza) and at the European Institute of Oncology (IEO, Milan, Italy) or referred to one of these centres after primary surgery elsewhere were included in this retrospective analysis. All patients in child-bearing age with a strong desire to retain fertility were proposed a fertility-sparing treatment. Patients who refused to be treated with this approach for any reason or who were in postmenopausal status underwent radical treatment. The two centres share the same approach for these patients. Patients with borderline EOC, ovarian germ cell tumours or stromal tumours were excluded.
The protocol of this analysis has been notified to the local ethics committee.
Patients were staged according to the International Federation of Gynecology and Obstetrics criteria (FIGO, 2003), using macroscopic findings and histological analysis of specimens obtained during initial and restaging surgery. Pathology slides were reviewed by one pathologist from each institution and a centralised pathological review has not been performed. Histological cell type and tumour differentiation were assessed according to the WHO (World Health Organization) criteria.
In the RS group, surgery was considered adequate when hysterectomy, bilateral salpingo-oophorectomy with peritoneal staging (peritoneal washing, omentectomy and multiple peritoneal biopsies) with retroperitoneal lymphadenectomy or sampling was performed. In the FSS group, surgery was considered adequate if cystectomy or unilateral adnexectomy was done, with peritoneal washing, omentectomy, careful inspection of the abdominal cavity with at least eight peritoneal biopsies, endometrial biopsy and evaluation of pelvic and para-aortic lymph nodes (meant as inspection and palpation with removal of any suspicious node, systematic lymphadenectomy or node sampling with at least 10 nodes).
The treatment plan for each patient was based on the adequacy of staging at first surgery.
In both groups patients with adequate staging surgery received six cycles of single-agent cisplatin or carboplatin if they had a grades 2 and 3 tumour or a FIGO stage IC.
Patients who underwent an inadequate initial staging surgery and were referred to our centres within 3 months underwent a restaging surgery (conservative in the FSS group, radical in the RS) and received chemotherapy according to risk factors cited above. Patients who came to our attention after more than 3 months but within 6 months received platinum-based chemotherapy and underwent a second surgery after completion of six cycles of therapy. Patients who were referred after more than 6 months were closely monitored and were considered eligible for a follow-up surgery according to clinical and histopathological risk factors.
Patients with inadequate initial staging surgery received six cycles of mono-chemotherapy with carboplatin if considered at high risk (FIGO stage IC-II or G2-G3) and at the end of the cycles underwent second-look surgery or were closely monitored; they were considered eligible for follow-up surgery only according to clinical and histopathological risk factors if they were considered at low risk (FIGO stage IA-B, G1). Since our centres participated in both ICON1 (Colombo et al, 2003) and ACTION (Trimbos et al, 2003) trials some patients received chemotherapy according to randomisation.
Statistical analysis
Aim of this analysis was to compare the clinical outcome in terms of CSS and RFI of patients with stage I EOC who received FSS with those who underwent RS. Furthermore, we investigated the prognostic role on survival outcomes of several clinical factors, irrespective of surgery performed.
CSS was defined as the time from surgery to the date of death from ovarian cancer. Patients known to be alive at the time of analysis were censored at their last available contact date. Deaths from other causes were regarded as competitive events.
RFI was defined as the time from surgery to the first appearance of relapse. Patients known to be alive and free of relapse at the time of analysis were censored at their last available follow-up. Deaths from any causes occurred before relapse were regarded as competitive events.
To take into account the wide period of observation, analyses were stratified by year of surgery (before 1993, 1993–2002, after 2002). Furthermore, a propensity score analysis was performed to avoid potential bias caused by the non-randomised allocation to one of the two surgeries. Propensity score was estimated using a multivariate logistic regression model having type of surgery as dependent variable and age as independent variables and entered into the corresponding treatment effect model as a covariate to adjust for baseline differences in addition to clinical factors.
Continuous variable summaries included mean and range, whereas for categorical variables the frequency and percentage of subjects who were in the particular treatment arm were used; the denominator for the percentage calculation was based on the total number of subjects in the relevant analysis group.
χ2, Wilcoxon and Kruskal–Wallis test were used to compare categorical and continuous variable, respectively. Cumulative incidence curves were estimated and compared with the Gray method. The stratified Fine–Gray proportional hazard model for the sub-distribution of a competing risk proposed by Zhou (Zhou et al, 2011) for univariate and multivariate analyses was used to test sparing and RS and possibly prognostic factors for their associations with CSS and RFI.
Results are expressed as point estimates and their confidence intervals at 95% (95% CIs).
Statistical significance was set at P<0.05 for a bilateral test. Analysis was carried out using the SAS (Statistical Analysis System, SAS Institute, Version 9.2, Cary, NC, USA) software and the R (The CRAN Project, Version 3.0) software (R Core Team, 2013).
Results
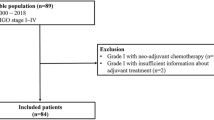
From 1981 to 2012 a total of 1031 patients with EOC apparently confined to the ovaries were treated at San Gerardo Hospital, Monza (830 patients, 80.5%) and at the European Institute of Oncology, Milan, Italy (201 patients, 19.5%). Two hundred and forty-two patients were treated with FSS (group A) and 789 with RS (group B).
Clinical and tumour characteristics of patients are listed in Table 2. Mean age was 31 and 53 years in groups A and B, respectively. FIGO stage distribution was similar in the two groups, even if patients in group A had a slightly yet significantly more favourable profile (Stage IA: 53% in group A and 43% in group B; and stage IC: 46% in group A and 49% in group B, P<0.001). The grade of nuclear differentiation was unevenly distributed among groups; in fact, grade 1 was predominant in group A (60% of patients), while grades 2 and 3 were both more frequent in group B (71%). Patients were defined as high and low risk in 64% and 36% and in 81% and 19% in groups A and B, respectively. The most represented histotype in group A was mucinous (42%), while in group B serous and endometrioid tumours accounted for 56%. Clear cell histotype was reported in 7% of patients in group A and in 17% in group B.
Surgery was considered adequate in a significantly higher percentage of patients in the RS group (73% vs 55%, P<0.001). Detailed surgical procedures performed in both group are listed in Supplementary Table 1. Adjuvant platinum-based chemotherapy was administered according to clinical and pathological risk factors to a significantly higher percentage of patients in group B (63%) compared with group A (43%), reflecting the different distribution of risk factors among the two groups.
After a median follow-up of 11.9 years relapse proportion was 12% and 21% in groups A and B (Supplementary Table 2), respectively. Deaths occurred in 15 patients (6%) in group A and in 185 patients (23%) in group B. In group A, three women died from another cause than ovarian cancer; in particular, one patient with stage IAG1 serous tumour had an intestinal cancer more than 5 years after ovarian cancer diagnosis and died 2 years later; one patient with IAG1 mucinous tumour died for acute myocardial infarction at the age of 58 years; and the last patient with stage ICG3 endometrioid tumour died 12 years after the diagnosis for an intestinal cancer.
At univariate analyses, FSS was significantly associated with decreased risk of disease relapse (sub-distribution hazard ratio (SHR), 0.53; 95% CI: 0.36–0.79; P=0.002) and of tumour-related death (SHR, 0.36; 95% CI: 0.20–0.67; P=0.001). Tumour grade was significantly associated with a shorter RFI (SHR, 1.84; 95% CI: 1.54–2.20; P<0.001) and CSS (SHR, 1.88; 95% CI: 1.48–2.38; P<0.001). Stage IC2/3 conferred shorter RFI (SHR, 1.51; 95% CI: 1.13–2.01; P=0.005) and a not clear cells histotype conferred longer CSS (SHR, 0.61; 95% CI: 0.38–0.99; P=0.043). Chemotherapy significantly shortened both RFI (SHR, 1.62; 95% CI: 1.20–2.19; P=0.002) and CSS (SHR, 1.64; 95% CI: 1.12–2.41; P=0.012).
Multivariate analysis did not confirm the independent positive role of FSS neither on RFI nor on CSS. Tumour grade was confirmed to be associated with shorter RFI (SHR, 2.07; 95% CI: 1.60–2.69; P<0.001) and shorter CSS (SHR, 1.80; 95% CI: 1.30–2.48; P<0.001). Risk of disease relapse increased significantly also in women with IC2/3 stage (SHR, 1.52; 95% CI: 1.10–2.10; P=0.011) and without a clear cells histotype (SHR, 1.68; 95% CI: 1.05–2.67; P=0.030) (Table 3).
Cumulative incidence curves for tumour-related mortality and relapse are shown in Figure 1A and in Figure 2A, respectively. Statistically significant differences were detected both on RFI and CSS. To investigate the role of surgery type according to tumour grade on the two endpoints, test for interaction was done and curves by grade were also provided. The two different surgeries showed a similar effect irrespective by tumour grade on RFI (P-value for interaction=0.570). Considering tumour-related mortality, the interaction between surgery type and tumour grade was statistically significant (P=0.031) and statistically significant differences between surgery type were detected in grade 1 patients (Figure 1B, Gray-test P-value=0.011). Nevertheless, multivariate analyses by tumour grade showed no effect of FSS on mortality (grade 1: SHR, 1.75; 95% CI: 0.11–28.40, P=0.690; grade 2: SHR, 0.37; 95% CI: 0.07–1.90, P=0.230; grade 3: SHR, 2.00; 95% CI: 0.49–8.10, P=0.330).
Discussion
The treatment of young women with ovarian cancer apparently confined to the ovary is always a challenging issue for physicians. The fear to worsen the prognosis with FSS leads most gynaecologists to propose a radical treatment, even in women who have not started or completed their child-bearing desire.
The majority of published studies on FSS were not enough to determine the impact of ovarian preservation on the oncological outcome of patients because comparison of this treatment with the standard RS was not done in these. Since patients with IC and G3 tumours have a higher risk of relapse and death, the recommendation for considering patients eligible to FSS has been, for the majority of authors, to exclude patients with such unfavourable characteristics. However, the recent large-scale retrospective analysis of Wright (Wright et al, 2009) and the remarkable retrospective analyses by Kajiyama (Kajiyama et al, 2011) and Ditto (Ditto et al, 2015) showed that there is not a clear evidence that removing the genital tract in patients with stage I EOC improves their oncological outcome.
The results of our analysis confirm the findings of the authors. However, there are some remarks that should be underlined. The first one concerns the characteristics of the two groups of patients. Beside age, which is obviously lower in the FSS group, the characteristics of tumours are very different. In fact, the predominant histological subtype in patients treated with FSS was mucinous (42%), while in patients treated with RS there was a significantly higher proportion of serous carcinoma (30%) and clear cell carcinoma (17%). Moreover, grade of nuclear differentiation was 1 in the majority of patients treated with FSS (60%) and 3 in patients treated with RS (42%). Finally, also FIGO stage distribution was different among the two groups, being IA predominant in the FSS group (53%) and IC in the RS group (49%). Taken together these observations could lead to two hypotheses: either women with unfavourable characteristics are treated preferentially with RS, or younger patients tend to have less aggressive and disseminated tumours.
Trying to find an answer to this question we observed that, regardless the treatment received, there is a direct significant association between age at diagnosis and grade of nuclear differentiation (G1: 40.4 years; G2: 48.6 years; G3: 52.3 years, Kruskal–Wallis test P-value<0.001).
Moreover, dividing patients in three groups based on age (<30 years, 30–45 years and >45 years), regardless the surgical treatment received, we observed a statistically significant distribution of grade of nuclear differentiation; in particular, grade 1 frequency decreases with age, grade 2 tends to remain stable and grade 3 frequency increases with age (Table 4). A similar trend exists also for stage and histological subtypes. These data support the hypothesis that there is an age-related distribution of risk factors in patients with stage I EOC. Therefore, to limit age differences in the two treatment group, an analyses were performed considering only patients younger than 45 years as control group (mean age: 38.7 years). Furthermore, propensity score was not included and age was evaluated as risk factor. Similar results have been obtained and summarised in Supplementary Table 3.
The hypothesis that lower age could be a positive prognostic factor for patients with EOC and the existence of biological differences in the behaviour of EOC in women of reproductive age compared with older women has already been reported by several authors (Lee et al, 1999; Bozas et al, 2006; Wimberger et al, 2006). However, all published series considered patients with advanced stage EOC; moreover, younger patients are usually treated with a more aggressive approach, and the doubt that the improved outcome was related to the physicians’ attitude could not be completely ruled out.
The type of treatment did not influence CSS (Figure 1C and D) in grades 2 and 3 patients or RFI (Figure 2B–D) in any grade group. The protective effect of FSS in grade 1 patients (Figure 1B) is probably because of the small number of events and to the favourable characteristics, beside grade, of patients undergoing FSS. Indeed in our study, multivariate analysis showed that FSS does not affect neither RFI nor CSS of our patients. The only factor determining a lower CSS is, as already mentioned in our previous report, the grade of nuclear differentiation.
This observations lead to our second hypothesis that the oncological outcome is determined by intrinsic tumour factors, which has the grade as a histological yet not exhaustive marker. This is also indirectly confirmed by reports indicating that, within the FIGO stage IC, patients with capsule infiltration, which is a sign of tumour aggressiveness, have a worse prognosis compared with patients with intraoperative rupture of the capsule (Kajiyama et al, 2014). This is confirmed in our population, as patients with IC2/3 stage disease have a significantly lower RFI and a lower (although not significant) CSS.
In the series of Kajiyama, he showed that patients with FIGO stage IC for positive cytology or preoperative rupture of the capsule, which is usually a contraindication for FSS, had the same relapse-free survival and overall survival in the two groups; he hypothesised that, in this group of patients, if occult metastases are present at the time of first surgery, they are more likely to be in the peritoneal cavity rather than on the contralateral ovary, and therefore standard RS would not be able to improve the survival. This is the same conclusion of our previous report on patients treated with FSS regarding G3 tumours. In these patients we observed a significantly higher frequency of distant relapse, which would probably not be cured by removing the contralateral ovary and the uterus at the time of first surgery. The observation has been confirmed by the recently published multi-institutional study on recurrences after FSS (Bentivegna et al, 2015).
Our study has some limitations that should be clearly acknowledged. First of all, the retrospective nature of the study hampers the possibility to draw definitive conclusions on the impact of FSS on the oncological outcome of patients with stage I EOC. However, due to ethical and practical considerations, a randomised clinical trial is not feasible in this setting of patients; this is the largest series of patients published in literature, and the results confirm the findings of the similar paper published by Kajiyama. Moreover, we were not able to identify how many patients gave up fertility preservation because of abdominal spread of the disease or positive lymph nodes at first surgery.
Another point that should be underlined is that surgery was considered adequate in a significantly lower proportion of patients treated with FSS, and this is due to the fact that these women often undergo surgery for a presumed benign tumour. Patients inadequately staged at first surgery and referred to our centre later than 3 months did not undergo a restaging surgery, and we chose to administer adjuvant chemotherapy to these patients, instead of a second surgery (which might potentially harm their fertility) since the ICON1/ACTION trial showed that the poor prognosis resulting from non-optimal staging could be corrected by chemotherapy (Colombo et al, 2003).
Finally the group of high-risk patients (G3 and IC G2/3) treated with FSS is relatively small. These patients have an higher risk to have a distant relapse, which greatly worsen the oncological outcome. Since this higher risk is maintained in patients treated with RS, its relationship with the preservation of the genital tract is uncertain. However, due to the small number of patients reported in the present study and in the literature, FSS should be considered with caution in this subgroup of women.
Therefore we can conclude that FSS is an adequate treatment for young patients with stage I EOC. When the diagnosis is made preoperatively, as well as in cases where tumour diagnosis is incidental, the decision of preserving the genital tract and fertility should be taken after a thoughtful and complete counselling. Patients should be aware that the prognosis is mainly determined by grade of nuclear differentiation, which cannot be preoperatively defined with the equipment available at the moment (US, CT, MRI and PET). This information is crucial, as we already observed that patients with a greater risk of relapse and death try to conceive less frequently compared with patients with low-grade tumours. This is probably due to an inadequate preoperative counselling, which should clarify that preservation of the genital tract will not, in any case, determine the oncological outcome of patients. Finally, patients should also be informed that younger age is significantly associated with more favourable tumour features (low-grade, mucinous histotype), as this evidence, coupled with a satisfactory pregnancy rate of 80%, might strengthen the decision to choose a fertility-sparing treatment.
Change history
06 September 2016
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Anchezar JP, Sardi J, Soderini A. (2009) Long-term follow-up results of fertility sparing surgery in patients with epithelial ovarian cancer. J Surg Oncol 100 (1): 55–58.
Bentivegna E, Fruscio R, Roussin S, Ceppi L, Satoh T, Kajiyama H, Uzan C, Colombo N, Gouy S, Morice P (2015) Long-term follow-up of patients with an isolated ovarian recurrence after conservative treatment of epithelial ovarian cancer: review of the results of a international multicenter study comprising 545 patients. Fertil Steril 104 (5): 1319–1324.
Borgfeldt C, Iosif C, Måsbäck A (2007) Fertility-sparing surgery and outcome in fertile women with ovarian borderline tumors and epithelial invasive ovarian cancer. Eur J Obstet Gynecol Reprod Biol 134 (1): 110–114.
Bozas G, Dimopoulos MA, Kastritis E, Efstathiou E, Koutsoukou V, Rodolakis A, Vlahos G, Voulgaris Z, Papageorgiou T, Gika D, Papadimitriou C, Bamias A (2006) Young age is associated with favorable characteristics but is not an independent prognostic factor in patients with epithelial ovarian cancer: a single institution experience. Oncology 70 (4): 265–272.
Cheng X, Cheng B, Wan X, Lu W, Xie X (2012) Outcomes of conservative surgery in early epithelial ovarian carcinoma. Eur J Gynaecol Oncol 33 (1): 93–95.
Colombo N, Guthrie D, Chiari S, Parmar M, Qian W, Swart AM, Torri V, Williams C, Lissoni A, Bonazzi C International Collaborative Ovarian Neoplasm (ICON) Collaborators (2003) International Collaborative Ovarian Neoplasm trial 1: a randomized trial of adjuvant chemotherapy in women with early-stage ovarian cancer. J Natl Cancer Inst 95 (2): 125–132.
Ditto A, Martinelli F, Bogani G, Lorusso D, Carcangiu M, Chiappa V, Reato C, Donfrancesco C, De Carrillo KJ, Raspagliesi F (2015) Long-term safety of fertility sparing surgery in early stage ovarian cancer: comparison to standard radical surgical procedures. Gynecol Oncol 138 (1): 78–82.
Duska LR, Chang YC, Flynn CE, Chen AH, Goodman A, Fuller AF, Nikrui N (1999) Epithelial ovarian carcinoma in the reproductive age group. Cancer 85 (12): 2623–2629.
FIGO (2003) FIGO (International Federation of Gynecology and Obstetrics) annual report on the results of treatment in gynecological cancer. Int J Gynaecol Obstet 83 (Suppl 1): 1–229.
Fruscio R, Corso S, Ceppi L, Garavaglia D, Garbi A, Floriani I, Franchi D, Cantù MG, Bonazzi CM, Milani R, Mangioni C, Colombo N (2013) Conservative management of early-stage epithelial ovarian cancer: results of a large retrospective series. Ann Oncol 24 (1): 138–144.
Hu J, Zhu LR, Liang ZQ, Meng YG, Guo HY, Qu PP, Ma CL, Xu CJ, Yuan BB (2011) Clinical outcomes of fertility-sparing treatments in young patients with epithelial ovarian carcinoma. J Zhejiang Univ Sci B 12 (10): 787–795.
Kajiyama H, Mizuno M, Shibata K, Yamamoto E, Kawai M, Nagasaka T, Kikkawa F (2014) Recurrence-predicting prognostic factors for patients with early-stage epithelial ovarian cancer undergoing fertility-sparing surgery: a multi-institutional study. Eur J Obstet Gynecol Reprod Biol 175: 97–102.
Kajiyama H, Shibata K, Mizuno M, Umezu T, Suzuki S, Nawa A, Kawai M, Nagasaka T, Kikkawa F (2011) Long-term survival of young women receiving fertility-sparing surgery for ovarian cancer in comparison with those undergoing radical surgery. Br J Cancer 105 (9): 1288–1294.
Kajiyama H, Shibata K, Suzuki S, Ino K, Nawa A, Kawai M, Nagasaka T, Kikkawa F (2010) Fertility-sparing surgery in young women with invasive epithelial ovarian cancer. Eur J Surg Oncol 36 (4): 404–408.
Kashima K, Yahata T, Fujita K, Tanaka K (2013) Outcomes of fertility-sparing surgery for women of reproductive age with FIGO stage IC epithelial ovarian cancer. Int J Gynaecol Obstet 121 (1): 53–55.
Kwon YS, Hahn HS, Kim TJ, Lee IH, Lim KT, Lee KH, Shim JU, Mok JE (2009) Fertility preservation in patients with early epithelial ovarian cancer. J Gynecol Oncol. 20 (1): 44–47.
Lee CK, Pires de Miranda M, Ledermann JA, Ruiz de Elvira MC, Nelstrop AE, Lambert HE, Rustin GJ, Trask CW (1999) Outcome of epithelial ovarian cancer in women under 40 years of age treated with platinum-based chemotherapy. Eur J Cancer 35 (5): 727–732.
Lee JY, Jo YR, Kim TH, Kim HS, Kim MA, Kim JW, Park NH, Song YS (2015) Safety of fertility-sparing surgery in primary mucinous carcinoma of the ovary. Cancer Res Treat 47 (2): 290–297.
Mathews TJ, Hamilton BE (2009) Delayed childbearing: more women are having their first child later in life. NCHS Data Brief, no 21. National Center for Health Statistics: Hyattsville, MD.
Morice P, Denschlag D, Rodolakis A, Reed N, Schneider A, Kesic V, Colombo N Fertility Task Force of the European Society of Gynecologic Oncology (2011) Recommendations of the fertility task force of the European society of gynecologic oncology about the conservative management of ovarian malignant tumors. Int J Gynecol Cancer 21 (5): 951–963.
Morice P, Leblanc E, Rey A, Baron M, Querleu D, Blanchot J, Duvillard P, Lhommé C, Castaigne D, Classe JM, Bonnier P GCCLCC and SFOG (2005) Conservative treatment in epithelial ovarian cancer: results of a multicentre study of the GCCLCC (Groupe des Chirurgiens de Centre de Lutte Contre le Cancer) and SFOG (Société Francaise d'Oncologie Gynécologique). Hum Reprod 20 (5): 1379–1385.
Park JY, Kim DY, Suh DS, Kim JH, Kim YM, Kim YT, Nam JH (2008) Outcomes of fertility-sparing surgery for invasive epithelial ovarian cancer: oncologic safety and reproductive outcomes. Gynecol Oncol 110 (3): 345–353.
R Core Team (2013) R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria. Available from: http://www.R-project.org/.
Satoh T, Hatae M, Watanabe Y, Yaegashi N, Ishiko O, Kodama S, Yamaguchi S, Ochiai K, Takano M, Yokota H, Kawakami Y, Nishimura S, Ogishima D, Nakagawa S, Kobayashi H, Shiozawa T, Nakanishi T, Kamura T, Konishi I, Yoshikawa H (2010) Outcomes of fertility-sparing surgery for stage I epithelial ovarian cancer: a proposal for patient selection. J Clin Oncol 28 (10): 1727–1732.
Schilder JM, Thompson AM, DePriest PD, Ueland FR, Cibull ML, Kryscio RJ, Modesitt SC, Lu KH, Geisler JP, Higgins RV, Magtibay PM, Cohn DE, Powell MA, Chu C, Stehman FB, van Nagell J (2002) Outcome of reproductive age women with stage IA or IC invasive epithelial ovarian cancer treated with fertility-sparing therapy. Gynecol Oncol 87 (1): 1–7.
Schlaerth AC, Chi DS, Poynor EA, Barakat RR, Brown CL (2009) Long-term survival after fertility-sparing surgery for epithelial ovarian cancer. Int J Gynecol Cancer 19 (7): 1199–1204.
Trimbos JB, Parmar M, Vergote I, Guthrie D, Bolis G, Colombo N, Vermorken JB, Torri V, Mangioni C, Pecorelli S, Lissoni A, Swart AM International Collaborative Ovarian Neoplasm 1; European Organisation for Research and Treatment of Cancer Collaborators-Adjuvant ChemoTherapy un Ovarian Neoplasm (2003) Impact of adjuvant chemotherapy and surgical staging in early-stage ovarian carcinoma: European Organisation for Research and Treatment of Cancer-Adjuvant ChemoTherapy in Ovarian Neoplasm Trial. J Natl Cancer Inst. 95 (2): 113–125.
Wimberger P, Lehmann N, Kimmig R, Burges A, Meier W, Hoppenau B, du Bois A AGO-OVAR (2006) Impact of age on outcome in patients with advanced ovarian cancer treated within a prospectively randomized phase III study of the Arbeitsgemeinschaft Gynaekologische Onkologie Ovarian Cancer Study Group (AGO-OVAR). Gynecol Oncol 100 (2): 300–307.
Wright JD, Shah M, Mathew L, Burke WM, Culhane J, Goldman N, Schiff PB, Herzog TJ (2009) Fertility preservation in young women with epithelial ovarian cancer. Cancer 115 (18): 4118–4126.
Zanetta G, Chiari S, Rota S, Bratina G, Maneo A, Torri V, Mangioni C (1997) Conservative surgery for stage I ovarian carcinoma in women of childbearing age. Br J Obstet Gynaecol 104 (9): 1030–1035.
Zhou B, Latouche A, Rocha V, Fine J (2011) Competing risks regression for stratified data. Biometrics 67 (2): 661–670.
Acknowledgements
This work is dedicated to the memory of Irene Floriani.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Fruscio, R., Ceppi, L., Corso, S. et al. Long-term results of fertility-sparing treatment compared with standard radical surgery for early-stage epithelial ovarian cancer. Br J Cancer 115, 641–648 (2016). https://doi.org/10.1038/bjc.2016.254
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2016.254
Keywords
This article is cited by
-
The pregnancy and oncology outcome of fertility-sparing management for synchronous primary neoplasm of endometrium and ovary
Journal of Ovarian Research (2023)
-
Successful delivery after in vitro fertilization-embryo transfer in a woman with metachronous primary cancer of ovary and endometrium: a case report
BMC Pregnancy and Childbirth (2023)
-
Survival analysis and obstetric outcomes in patients with early stage ovarian cancer undergoing fertility-sparing surgery
Journal of Ovarian Research (2022)
-
Oncologic outcomes of fertility-sparing surgery in early stage epithelial ovarian cancer: a population-based propensity score-matched analysis
Archives of Gynecology and Obstetrics (2022)
-
A Swedish Nationwide prospective study of oncological and reproductive outcome following fertility-sparing surgery for treatment of early stage epithelial ovarian cancer in young women
BMC Cancer (2020)