Abstract
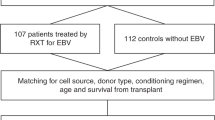
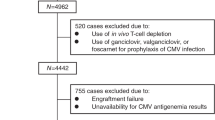
EBV viremia and post-transplantation lymphoproliferative disorders (PTLDs) have been associated with high mortality rates after allogeneic hematopoietic SCT (allo-HSCT). Few retrospective studies, without EBV load monitoring postulated that umbilical cord blood transplantation (UCBT) might be associated with high incidence of EBV events. We retrospectively studied 175 UCBT recipients for whom RQ–PCR was used to monitor EBV blood load at least once a week during the first 3 months after UCBT. Median age was 23 years, 74% had leukemia. Conditioning was myeloablative in 54% and reduced intensity conditioning (RIC) was used in 46%. A total of 24 patients presented an EBV reactivation. For 15 patients, the reactivation occurred during the first 100 days (cumulative incidence: 8%) and included 4 EBV-PTLD. Rituximab as preemptive treatment was used in 12 of these 15 patients. In univariate analysis, the increased risk of early EBV reactivation was associated with RIC in combination with antithymocyte globulin (P=0.03) and previous history of auto-HSCT (P=0.01). Multivariate analysis did not find any independent risk factor. EBV reactivation as time-dependent covariate was not statistically associated with survival. Therefore, EBV events were not major complications after UCBT when EBV load is weekly monitored and preemptive treatment started.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Cohen JI . Epstein-Barr virus infection. N Engl J Med 2000; 343: 481–492.
Sundin M, Le Blanc K, Ringden O, Barkholt L, Omazic B, Lergin C et al. The role of HLA mismatch, splenectomy and recipient Epstein-Barr virus seronegativity as risk factors in post-transplant lymphoproliferative disorder following allogeneic hematopoietic stem cell transplantation. Haematologica 2006; 91: 1059–1067.
Curtis RE, Travis LB, Rowlings PA, Socie G, Kingma DW, Banks PM et al. Risk of lymphoproliferative disorders after bone marrow transplantation: a multi-institutional study. Blood 1999; 94: 2208–2216.
Landgren O, Gilbert ES, Rizzo JD, Socie G, Banks PM, Sobocinski KA et al. Risk factors for lymphoproliferative disorders after allogeneic hematopoietic cell transplantation. Blood 2009; 113: 4992–5001.
Seggewiss R, Einsele H . Immune reconstitution after allogeneic transplantation and expanding options for immunomodulation: an update. Blood 2010; 115: 3861–3868.
Barker JN, Martin PL, Coad JE, DeFor T, Trigg ME, Kurtzberg J et al. Low incidence of Epstein-Barr virus-associated posttransplantation lymphoproliferative disorders in 272 unrelated-donor umbilical cord blood transplant recipients. Biol Blood Marrow Transplant 2001; 7: 395–399.
Brunstein CG, Weisdorf DJ, DeFor T, Barker JN, Tolar J, van Burik JA et al. Marked increased risk of Epstein-Barr virus-related complications with the addition of antithymocyte globulin to a nonmyeloablative conditioning prior to unrelated umbilical cord blood transplantation. Blood 2006; 108: 2874–2880.
Peric Z, Cahu X, Chevallier P, Brissot E, Malard F, Guillaume T et al. Features of EBV reactivation after reduced intensity conditioning unrelated umbilical cord blood transplantation. Bone Marrow Transplant 2012; 47: 251–257.
Styczynski J, Reusser P, Einsele H, de la Camara R, Cordonnier C, Ward KN et al. Management of HSV, VZV and EBV infections in patients with hematological malignancies and after SCT: guidelines from the Second European Conference on Infections in Leukemia. Bone Marrow Transplant 2009; 43: 757–770.
Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation 1974; 18: 295–304.
Cohen J, Gandhi M, Naik P, Cubitt D, Rao K, Thaker U et al. Increased incidence of EBV-related disease following paediatric stem cell transplantation with reduced-intensity conditioning. Br J Haematol 2005; 129: 229–239.
van Esser JW, Niesters HG, van der Holt B, Meijer E, Osterhaus AD, Gratama JW et al. Prevention of Epstein-Barr virus-lymphoproliferative disease by molecular monitoring and preemptive rituximab in high-risk patients after allogeneic stem cell transplantation. Blood 2002; 99: 4364–4369.
van Esser JW, van der Holt B, Meijer E, Niesters HG, Trenschel R, Thijsen SF et al. Epstein-Barr virus (EBV) reactivation is a frequent event after allogeneic stem cell transplantation (SCT) and quantitatively predicts EBV-lymphoproliferative disease following T-cell—depleted SCT. Blood 2001; 98: 972–978.
Chevallier P, Hebia-Fellah I, Planche L, Guillaume T, Bressolette-Bodin C, Coste-Burel M et al. Human herpes virus 6 infection is a hallmark of cord blood transplant in adults and may participate to delayed engraftment: a comparison with matched unrelated donors as stem cell source. Bone Marrow Transplant 2010; 45: 1204–1211.
Robin M, Marque-Juillet S, Scieux C, Peffault de Latour R, Ferry C, Rocha V et al. Disseminated adenovirus infections after allogeneic hematopoietic stem cell transplantation: incidence, risk factors and outcome. Haematologica 2007; 92: 1254–1257.
Vandenbosch K, Ovetchkine P, Champagne MA, Haddad E, Alexandrov L, Duval M . Varicella-zoster virus disease is more frequent after cord blood than after bone marrow transplantation. Biol Blood Marrow Transplant 2008; 14: 867–871.
Acknowledgements
We would like to thank Mazar Tassadit and Pr Dominique Bordessoule, University Hospital, Limoges, France; Pr Marie-Edith Lafon, University Hospital and University Bordeaux 2, Bordeaux, France; and Chantal Kenzey, EUROCORD, Paris, France.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Dumas, PY., Ruggeri, A., Robin, M. et al. Incidence and risk factors of EBV reactivation after unrelated cord blood transplantation: a Eurocord and Société Française de Greffe de Moelle-Therapie Cellulaire collaborative study. Bone Marrow Transplant 48, 253–256 (2013). https://doi.org/10.1038/bmt.2012.117
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2012.117
Keywords
This article is cited by
-
Effects of HLA mismatch on cytomegalovirus reactivation in cord blood transplantation
Bone Marrow Transplantation (2019)
-
Epstein–Barr virus–associated post-transplant lymphoproliferative disorder among long-term survivors of adults after single cord blood transplantation without antithymocyte globulin
Annals of Hematology (2019)
-
Haploidentical transplantation is associated with better overall survival when compared to single cord blood transplantation: an EBMT-Eurocord study of acute leukemia patients conditioned with thiotepa, busulfan, and fludarabine
Journal of Hematology & Oncology (2018)
-
EBV-associated post-transplant lymphoproliferative disorder after umbilical cord blood transplantation in adults with hematological diseases
Bone Marrow Transplantation (2014)