Abstract
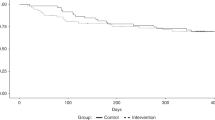
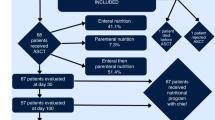
There are few longitudinal data on nutritional status and body composition of patients undergoing allogeneic hematopoietic cell transplantation (alloHCT). We assessed nutritional status of 105 patients before alloHCT and its course during the early post-transplant period to day +30 and day +100 via weight history, body mass index (BMI) normalized for gender and age, Subjective Global Assessment, phase angle normalized for gender, age, and BMI, and fat-free and body fat masses. Furthermore, we present a multivariate regression model investigating the impact of factors on body weight. At admission, 23.8% reported significant weight losses (>5%) in the previous 6 months, and we noted 31.5% with abnormal age- and sex-adjusted BMI values (⩽10th, ⩾90th percentiles). BMI decreased significantly (P<0.0001) in both periods by 11% in total, meaning a weight loss of 8.6±5.7 kg. Simultaneously, the patients experienced significant losses (P<0.0001) of both fat-free and body fat masses. Multivariate regression model revealed clinically relevant acute GVHD (parameter estimate 1.43; P=0.02) and moderate/severe anorexia (parameter estimate 1.07; P=0.058) as independent factors influencing early weight loss. In conclusion, our results show a significant deterioration in nutritional status during the early post-transplant period. Predominant alloHCT-associated complications such as anorexia and acute GVHD became evident as significant factors influencing nutritional status.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Tabbara IA, Zimmerman K, Morgan C, Nahleh Z . Allogeneic hematopoietic stem cell transplantation: complications and results. Arch Intern Med 2002; 162: 1558–1566.
Bearman SI, Appelbaum FR, Back A, Petersen FB, Buckner CD, Sullivan KM et al. Regimen-related toxicity and early posttransplant survival in patients undergoing marrow transplantation for lymphoma. J Clin Oncol 1989; 7: 1288–1294.
Bertz H, Illerhaus G, Veelken H, Finke J . Allogeneic hematopoetic stem-cell transplantation for patients with relapsed or refractory lymphomas: comparison of high-dose conventional conditioning versus fludarabine-based reduced-intensity regimens. Ann Oncol 2002; 13: 135–139.
Urbain P, Raynor A, Bertz H, Lambert C, Biesalski HK . Role of antioxidants in buccal mucosa cells and plasma on the incidence and severity of oral mucositis after allogeneic haematopoietic cell transplantation. Support Care Cancer 2012; 20: 1831–1838.
Hickson RC, Marone JR . Exercise and inhibition of glucocorticoid-induced muscle atrophy. Exerc Sport Sci Rev 1993; 21: 135–167.
LaPier TK . Glucocorticoid-induced muscle atrophy. The role of exercise in treatment and prevention. J Cardiopulm Rehabil 1997; 17: 76–84.
Fleming DR, Rayens MK, Garrison J . Impact of obesity on allogeneic stem cell transplant patients: a matched case-controlled study. Am J Med 1997; 102: 265–268.
Le Blanc K, Ringden O, Remberger M . A low body mass index is correlated with poor survival after allogeneic stem cell transplantation. Haematologica 2003; 88: 1044–1052.
Lenssen P, Sherry ME, Cheney CL, Nims JW, Sullivan KM, Stern JM et al. Prevalence of nutrition-related problems among long-term survivors of allogeneic marrow transplantation. J Am Diet Assoc 1990; 90: 835–842.
Nikolousis E, Nagra S, Paneesha S, Delgado J, Holder K, Bratby L et al. Allogeneic transplant outcomes are not affected by body mass index (BMI) in patients with haematological malignancies. Ann Hematol 2010; 89: 1141–1145.
Kyle UG, Chalandon Y, Miralbell R, Karsegard VL, Hans D, Trombetti A et al. Longitudinal follow-up of body composition in hematopoietic stem cell transplant patients. Bone Marrow Transplant 2005; 35: 1171–1177.
High KP, Legault C, Sinclair JA, Cruz J, Hill K, Hurd DD . Low plasma concentrations of retinol and alpha-tocopherol in hematopoietic stem cell transplant recipients: the effect of mucositis and the risk of infection. Am J Clin Nutr 2002; 76: 1358–1366.
Kreutz M, Eissner G, Hahn J, Andreesen R, Drobnik W, Holler E . Variations in 1 alpha,25-dihydroxyvitamin D3 and 25-hydroxyvitamin D3 serum levels during allogeneic bone marrow transplantation. Bone Marrow Transplant 2004; 33: 871–873.
Urbain P, Ihorst G, Biesalski HK, Bertz H . Course of serum 25-hydroxyvitamin D(3) status and its influencing factors in adults undergoing allogeneic hematopoietic cell transplantation. Ann Hematol 2012; 91: 759–766.
Barbosa-Silva MC, Barros AJ . Bioelectrical impedance analysis in clinical practice: a new perspective on its use beyond body composition equations. Curr Opin Clin Nutr Metab Care 2005; 8: 311–317.
Norman K, Stobaus N, Zocher D, Bosy-Westphal A, Szramek A, Scheufele R et al. Cutoff percentiles of bioelectrical phase angle predict functionality, quality of life, and mortality in patients with cancer. Am J Clin Nutr 2010; 92: 612–619.
Faisy C, Rabbat A, Kouchakji B, Laaban JP . Bioelectrical impedance analysis in estimating nutritional status and outcome of patients with chronic obstructive pulmonary disease and acute respiratory failure. Intensive Care Med 2000; 26: 518–525.
Gupta D, Lammersfeld CA, Burrows JL, Dahlk SL, Vashi PG, Grutsch JF et al. Bioelectrical impedance phase angle in clinical practice: implications for prognosis in advanced colorectal cancer. Am J Clin Nutr 2004; 80: 1634–1638.
Gupta D, Lammersfeld CA, Vashi PG, King J, Dahlk SL, Grutsch JF et al. Bioelectrical impedance phase angle as a prognostic indicator in breast cancer. BMC Cancer 2008; 8: 249.
Gupta D, Lis CG, Dahlk SL, Vashi PG, Grutsch JF, Lammersfeld CA . Bioelectrical impedance phase angle as a prognostic indicator in advanced pancreatic cancer. Br J Nutr 2004; 92: 957–962.
Toso S, Piccoli A, Gusella M, Menon D, Bononi A, Crepaldi G et al. Altered tissue electric properties in lung cancer patients as detected by bioelectric impedance vector analysis. Nutrition 2000; 16: 120–124.
Detsky AS, McLaughlin JR, Baker JP, Johnston N, Whittaker S, Mendelson RA et al. What is subjective global assessment of nutritional status? JPEN J Parenter Enteral Nutr 1987; 11: 8–13.
Detsky AS, Baker JP, Mendelson RA, Wolman SL, Wesson DE, Jeejeebhoy KN . Evaluating the accuracy of nutritional assessment techniques applied to hospitalized patients: methodology and comparisons. JPEN J Parenter Enteral Nutr 1984; 8: 153–159.
Isenring E, Cross G, Daniels L, Kellett E, Koczwara B . Validity of the malnutrition screening tool as an effective predictor of nutritional risk in oncology outpatients receiving chemotherapy. Support Care Cancer 2006; 14: 1152–1156.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood 2005; 106: 2912–2919.
WHO. World Health Organization Handbook for Reporting Results of Cancer Treatment. World Health Organization: Geneva, 1979.
Hemmelmann C, Brose S, Vens M, Hebebrand J, Ziegler A . [Percentiles of body mass index of 18-80-year-old German adults based on data from the Second National Nutrition Survey]. Dtsch Med Wochenschr 2010; 135: 848–852.
Lim SL, Ong KC, Chan YH, Loke WC, Ferguson M, Daniels L . Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clin Nutr 2012; 31: 345–350.
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gomez JM et al. Bioelectrical impedance analysis-part I: review of principles and methods. Clin Nutr 2004; 23: 1226–1243.
Fredrix EW, Saris WH, Soeters PB, Wouters EF, Kester AD, von Meyenfeldt MF et al. Estimation of body composition by bioelectrical impedance in cancer patients. Eur J Clin Nutr 1990; 44: 749–752.
Paiva SI, Borges LR, Halpern-Silveira D, Assuncao MC, Barros AJ, Gonzalez MC . Standardized phase angle from bioelectrical impedance analysis as prognostic factor for survival in patients with cancer. Support Care Cancer 2011; 19: 187–192.
Schwenk A, Beisenherz A, Romer K, Kremer G, Salzberger B, Elia M . Phase angle from bioelectrical impedance analysis remains an independent predictive marker in HIV-infected patients in the era of highly active antiretroviral treatment. Am J Clin Nutr 2000; 72: 496–501.
Bosy-Westphal A, Danielzik S, Dorhofer RP, Later W, Wiese S, Muller MJ . Phase angle from bioelectrical impedance analysis: population reference values by age, sex, and body mass index. JPEN J Parenter Enteral Nutr 2006; 30: 309–316.
Barbosa-Silva MC, Barros AJ, Wang J, Heymsfield SB, Pierson RN . Bioelectrical impedance analysis: population reference values for phase angle by age and sex. Am J Clin Nutr 2005; 82: 49–52.
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Manuel Gomez J et al. Bioelectrical impedance analysis-part II: utilization in clinical practice. Clin Nutr 2004; 23: 1430–1453.
Segal KR, Gutin B, Presta E, Wang J, Van Itallie TB . Estimation of human body composition by electrical impedance methods: a comparative study. J Appl Physiol 1985; 58: 1565–1571.
VanItallie TB, Yang MU, Heymsfield SB, Funk RC, Boileau RA . Height-normalized indices of the body’s fat-free mass and fat mass: potentially useful indicators of nutritional status. Am J Clin Nutr 1990; 52: 953–959.
Wang ZM, Pierson RN, Heymsfield SB . The five-level model: a new approach to organizing body-composition research. Am J Clin Nutr 1992; 56: 19–28.
Wang Z, Heshka S, Gallagher D, Boozer CN, Kotler DP, Heymsfield SB . Resting energy expenditure-fat-free mass relationship: new insights provided by body composition modeling. Am J Physiol Endocrinol Metab 2000; 279: E539–E545.
Costelli P, Baccino FM . Cancer cachexia: from experimental models to patient management. Curr Opin Clin Nutr Metab Care 2000; 3: 177–181.
Chuang HH, Li WC, Sheu BF, Liao SC, Chen JY, Chang KC et al. Correlation between body composition and risk factors for cardiovascular disease and metabolic syndrome. Biofactors 2012; 38: 284–291.
Marks R, Potthoff K, Hahn J, Ihorst G, Bertz H, Spyridonidis A et al. Reduced-toxicity conditioning with fludarabine, BCNU, and melphalan in allogeneic hematopoietic cell transplantation: particular activity against advanced hematologic malignancies. Blood 2008; 112: 415–425.
WHO. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 2000; 894: 1–253.
Horsley P, Bauer J, Gallagher B . Poor nutritional status prior to peripheral blood stem cell transplantation is associated with increased length of hospital stay. Bone Marrow Transplant 2005; 35: 1113–1116.
Iestra JA, Fibbe WE, Zwinderman AH, Romijn JA, Kromhout D . Parenteral nutrition following intensive cytotoxic therapy: an exploratory study on the need for parenteral nutrition after various treatment approaches for haematological malignancies. Bone Marrow Transplant 1999; 23: 933–939.
Laviano A, Meguid MM . Nutritional issues in cancer management. Nutrition 1996; 12: 358–371.
Engeland A, Bjorge T, Selmer RM, Tverdal A . Height and body mass index in relation to total mortality. Epidemiology 2003; 14: 293–299.
Seccareccia F, Lanti M, Menotti A, Scanga M . Role of body mass index in the prediction of all cause mortality in over 62 000 men and women. The Italian RIFLE Pooling Project. Risk Factor and Life Expectancy. J Epidemiol Community Health 1998; 52: 20–26.
Dittmar M . Reliability and variability of bioimpedance measures in normal adults: effects of age, gender, and body mass. Am J Phys Anthropol 2003; 122: 361–370.
White M, Murphy AJ, Hastings Y, Shergold J, Young J, Montgomery C et al. Nutritional status and energy expenditure in children pre-bone-marrow-transplant. Bone Marrow Transplant 2005; 35: 775–779.
Cheney CL, Abson KG, Aker SN, Lenssen P, Cunningham BA, Buergel NS et al. Body composition changes in marrow transplant recipients receiving total parenteral nutrition. Cancer 1987; 59: 1515–1519.
Iestra JA, Fibbe WE, Zwinderman AH, van Staveren WA, Kromhout D . Body weight recovery, eating difficulties and compliance with dietary advice in the first year after stem cell transplantation: a prospective study. Bone Marrow Transplant 2002; 29: 417–424.
Rodgers C, Walsh T . Nutritional issues in adolescents after bone marrow transplant: a literature review. J Pediatr Oncol Nurs 2008; 25: 254–264.
Deschler B, Binek K, Ihorst G, Marks R, Wasch R, Bertz H et al. Prognostic factor and quality of life analysis in 160 patients aged>or =60 years with hematologic neoplasias treated with allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant 2010; 16: 967–975.
Cano NJ, Roth H, Court-Ortune I, Cynober L, Gerard-Boncompain M, Cuvelier A et al. Nutritional depletion in patients on long-term oxygen therapy and/or home mechanical ventilation. Eur Respir J 2002; 20: 30–37.
Heitmann BL, Erikson H, Ellsinger BM, Mikkelsen KL, Larsson B . Mortality associated with body fat, fat-free mass and body mass index among 60-year-old swedish men-a 22-year follow-up. The study of men born in 1913. Int J Obes Relat Metab Disord 2000; 24: 33–37.
Biring MS, Fournier M, Ross DJ, Lewis MI . Cellular adaptations of skeletal muscles to cyclosporine. J Appl Physiol 1998; 84: 1967–1975.
Mercier JG, Hokanson JF, Brooks GA . Effects of cyclosporine A on skeletal muscle mitochondrial respiration and endurance time in rats. Am J Respir Crit Care Med 1995; 151: 1532–1536.
Grullich C, Bertz H, Spyridonidis A, Muller CI, Finke J . A fludarabine, thiotepa reduced toxicity conditioning regimen designed specifically for allogeneic second haematopoietic cell transplantation after failure of previous autologous or allogeneic transplantation. Bone Marrow Transplant 2008; 41: 845–850.
Acknowledgements
We are grateful to Carole Cuerten for proofreading this manuscript, to Gabriele Ihorst from the Institute of Medical Biometry of the Albert-Ludwigs University of Freiburg for the statistical advice. P Urbain was supported by a PhD grant from the National Research Fund, Luxemburg.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Urbain, P., Birlinger, J., Lambert, C. et al. Longitudinal follow-up of nutritional status and its influencing factors in adults undergoing allogeneic hematopoietic cell transplantation. Bone Marrow Transplant 48, 446–451 (2013). https://doi.org/10.1038/bmt.2012.158
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2012.158
Keywords
This article is cited by
-
The European Society for Blood and Marrow Transplantation (EBMT) roadmap and perspectives to improve nutritional care in patients undergoing hematopoietic stem cell transplantation on behalf of the Cellular Therapy and Immunobiology Working Party (CTIWP) and the Nurses Group (NG) of the EBMT
Bone Marrow Transplantation (2023)
-
HCT frailty scale for younger and older adults undergoing allogeneic hematopoietic cell transplantation
Bone Marrow Transplantation (2023)
-
The association between nutritional risk index and ICU outcomes across hematologic malignancy patients with acute respiratory failure
Annals of Hematology (2023)
-
Reliability and validity of ultrasound to measure of muscle mass following allogeneic hematopoietic stem cell transplantation
Scientific Reports (2022)
-
Correlation of nutrition-associated parameters with non-relapse mortality in allogeneic hematopoietic stem cell transplantation
Annals of Hematology (2022)