Abstract
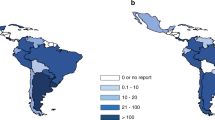
Chemotherapy and irradiation can affect the gonads, leading to impairment of pubertal development and/or infertility. Fertility preservation (FP) is therefore a crucial endeavor in hematopoietic stem cell transplantation (HSCT) because of the severe impact of infertility on the quality of life of long-term survivors. Despite the existence of different international guidelines, FP counseling and procedures are not routinely implemented as part of patient care. We present herein a survey conducted by the Pediatric Working Party of the European Society for Blood and Marrow Transplantation (EBMT), which aims to analyze and compare different FP practices for children and adolescents across EBMT centers in 2013. A total of 177 pediatric centers reporting to the EBMT were contacted; of this number, 38 centers (21%) located in 16 different countries responded. These centers reported 834 patients receiving HSCT in 2013 (73% prepubertal), corresponding to 22% of all children (n=3789) undergoing HSCT in EBMT reporting centers. Overall, 39% of the reported patients received counseling and 29% received an FP procedure. The increased need for FP programs, extended education for patient-care teams, and more personal resources and funding emerged from this survey as pivotal factors necessary to support and implement such programs.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Rovo A, Tichelli A, Passweg JR, Heim D, Meyer-Monard S, Holzgreve W et al. Spermatogenesis in long-term survivors after allogeneic hematopoietic stem cell transplantation is associated with age, time interval since transplantation, and apparently absence of chronic GvHD. Blood 2006; 108: 1100–1105.
Bresters D, Emons JAM, Nuri N, Ball LM, Kollen WJW, Hannema SE et al. Ovarian insufficiency and pubertal development after hematopoietic stem cell transplantation in childhood. Pediatr Blood Cancer 2014; 61: 2048–2053.
Schover LR . Psychosocial aspects of infertility and decisions about reproduction in young cancer survivors: a review. Med Pediatr Oncol 1999; 33: 53–59.
Crawshaw MA, Sloper P . 'Swimming against the tide' - the influence of fertility matters on the transition to adulthood or survivorship following adolescent cancer. Eur J Cancer Care (Engl) 2010; 19: 610–620.
Rovo A, Aljurf M, Chiodi S, Spinelli S, Salooja N, Sucak G et al. Ongoing graft-versus-host disease is a risk factor for azoospermia after allogeneic hematopoietic stem cell transplantation: a survey of the Late Effects Working Party of the European Group for Blood and Marrow Transplantation. Haematologica 2013; 98: 339–345.
Joshi S, Savani BN, Chow EJ, Gilleece MH, Halter J, Jacobsohn DA et al. Clinical guide to fertility preservation in hematopoietic cell transplant recipients. Bone Marrow Transplant 2014; 49: 477–484.
Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 2013; 31: 2500–2510.
Benedict C, Thom B, Kelvin JF . Fertility preservation and cancer: challenges for adolescent and young adult patients. Curr Opin Support Palliat Care 2016; 10: 87–94.
Lambertini M, Del Mastro L, Pescio MC, Andersen CY, Azim HA Jr, Peccatori FA et al. Cancer and fertility preservation: international recommendations from an expert meeting. BMC Med 2016; 14: 1.
Terenziani M, Spinelli M, Jankovic M, Bardi E, Hjorth L, Haupt R et al. Practices of pediatric oncology and hematology providers regarding fertility issues: a European survey. Pediatric Blood Cancer 2014; 61: 2054–2058.
Panagiotopoulou N, Ghuman N, Sandher R, Herbert M, Stewart JA . Barriers and facilitators towards fertility preservation care for cancer patients: a meta-synthesis. Eur J Cancer Care (e-pub ahead of print 17 December 2015; doi: 10.1111/ecc.12428).
Passweg JR, Baldomero H, Bader P, Bonini C, Cesaro S, Dreger P et al. Hematopoietic SCT in Europe 2013: recent trends in the use of alternative donors showing more haploidentical donors but fewer cord blood transplants. Bone Marrow Transplant 2015; 50: 476–482.
Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol 2006; 24: 2917–2931 (Erratum in: J Clin Oncol 2006; 24: 5790.
Multidisciplinary Working Group convened by the British Fertility Society. A strategy for fertility services for survivors of childhood cancer. Hum Fertil (Camb) 2003; 6: A1–A39.
Quinn GP, Knapp CA, Malo TL, McIntyre J, Jacobsen PB, Vadaparampil ST . Physicians' undecided attitudes toward posthumous reproduction: fertility preservation in cancer patients with a poor prognosis. J Support Oncol 2012; 10: 160–165.
Loren AW, Brazauskas R, Chow EJ, Gilleece M, Halter J, Jacobsohn DA et al. Physician perceptions and practice patterns regarding fertility preservation in hematopoietic cell transplant recipients. Bone Marrow Transplant 2013; 48: 1091–1097.
Reynolds KA, Grindler NM, Rhee JS, Cooper AR, Ratts VS, Carson KR et al. Variability in the practice of fertility preservation for patients with cancer. PLoS ONE 2015; 10: e0127335.
Abir R, Ben-Aharon I, Garor R, Yaniv I, Ash S, Stemmer SM et al. Cryopreservation of in vitro matured oocytes in addition to ovarian tissue freezing for fertility preservation in paediatric female cancer patients before and after cancer therapy. Hum Reprod 2016; 31: 750–762.
Dolmans MM, Luyckx V, Donnez J, Andersen CY, Greve T . Risk of transferring malignant cells with transplanted frozen-thawed ovarian tissue. Fertil Steril 2013; 99: 1514–1522.
Rosendahl M, Greve T, Andersen CY . The safety of transplanting cryopreserved ovarian tissue in cancer patients: a review of the literature. J Assist Reprod Genet 2013; 30: 11–24.
Wallace WH, Smith AG, Kelsey TW, Edgar AE, Anderson RA . Fertility preservation for girls and young women with cancer: population-based validation of criteria for ovarian tissue cryopreservation. Lancet Oncol 2014; 15: 1129–1136.
Bedaiwy MA, Abou-Setta AM, Desai N, Hurd W, Starks D, El-Nashar SA et al. Gonadotropin-releasing hormone analog cotreatment for preservation of ovarian function during gonadotoxic chemotherapy: a systematic review and meta-analysis. Fertili Steril 2011; 95: 906–914 e1-e4.
Bildik G, Akin N, Senbabaoglu F, Sahin GN, Karahuseyinoglu S, Ince U et al. GnRH agonist leuprolide acetate does not confer any protection against ovarian damage induced by chemotherapy and radiation in vitro. Hum Reprod 2015; 30: 2912–2925.
Nangia AK, Krieg SA, Kim SS . Clinical guidelines for sperm cryopreservation in cancer patients. Fertil Steril 2013; 100: 1203–1209.
Caponecchia L, Cimino G, Sacchetto R, Fiori C, Sebastianelli A, Salacone P et al. Do malignant diseases affect semen quality? Sperm parameters of men with cancers. Andrologia 2016; 48: 333–340.
Paoli D, Rizzo F, Fiore G, Pallotti F, Pulsoni A, Annechini G et al. Spermatogenesis in Hodgkin's lymphoma patients: a retrospective study of semen quality before and after different chemotherapy regimens. Hum Reprod 2016; 31: 263–272.
Hallak J, Mahran AM, Agarwal A . Characteristics of cryopreserved semen from men with lymphoma. J Assist Reprod Genet 2000; 17: 591–595.
Berookhim BM, Palermo GD, Zaninovic N, Rosenwaks Z, Schlegel PN . Microdissection testicular sperm extraction in men with Sertoli cell-only testicular histology. Fertil Steril 2014; 102: 1282–1286.
Kharizinejad E, Minaee Zanganeh B, Khanlarkhani N, Mortezaee K, Rastegar T, Baazm M et al. Role of spermatogonial stem cells extract in transdifferentiation of 5-Aza-2'-deoxycytidine-treated bone marrow mesenchymal stem cells into germ-like cells. Microsc Res Tech 2016; 79: 365–373.
Picton HM, Wyns C, Anderson RA, Goossens E, Jahnukainen K, Kliesch S et al. A European perspective on testicular tissue cryopreservation for fertility preservation in prepubertal and adolescent boysdagger. Hum Reprod 2015; 30: 2463–2475.
Sherman JK . Synopsis of the use of frozen human semen since 1964: state of the art of human semen banking. Fertil Steril 1973; 24: 397–412.
Acknowledgements
We thank all of the centers that participated in this survey. We also thank Andres M, Ansari M, Arola M, Arvidson J, Balduzzi A, Biasin E, Blecke M, Brester D, Burkhardt B, Cesaro S, Diaz M, Diaz de Heredia C, Dalle JH, Ferster A, Foell J, Hazar V, Jahnukainen K, Jarisch A, Kepak T, Keplova P, Kersting S, Kroiss S, Lätheenmäki P, Leversen M, Matthes S, Menconi M, Paillard C, Paolucci P, Pascual A, Plantaz D, Renard M, Schulz A, Stutz-Grunder E, Tinner E, Trigoso E, Vaitkeviciene G, Vettenranta J, Vettenranta K, Vora AJ, Williams J, and Yilmaz S for their substantial contributions to this research. This project was supported by the Susy Rückert Gedächtnisstiftung (Basel, Switzerland) and the Stiftung für Krebskranke Kinder, Regio Basiliensis (Basel, Switzerland).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Diesch, T., Rovo, A., von der Weid, N. et al. Fertility preservation practices in pediatric and adolescent cancer patients undergoing HSCT in Europe: a population-based survey. Bone Marrow Transplant 52, 1022–1028 (2017). https://doi.org/10.1038/bmt.2016.363
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2016.363
This article is cited by
-
Ethical, legal, social, and policy issues of ovarian tissue cryopreservation in prepubertal girls: a critical interpretive review
Journal of Assisted Reproduction and Genetics (2024)
-
Fertilitätserhalt bei Tumoren im Kindes- und Jugendalter
Der Onkologe (2021)
-
How can fertility counseling be implemented for every newly diagnosed pediatric patient facing gonadotoxic treatment?-A single-center experience
Annals of Hematology (2021)
-
Impact of legislation and public funding on oncofertility: a survey of Canadian, French and Moroccan pediatric hematologists/oncologists
BMC Medical Ethics (2020)
-
Fertility preservation from the point of view of hematopoietic cell transplant specialists—a worldwide-web-based survey analysis
Bone Marrow Transplantation (2019)