Abstract
Background/Objectives:
To evaluate the effect of a 4.1-year (range 3–6 years) lifestyle intervention according to general public health recommendations on glucose tolerance and dropout in a Dutch population with impaired glucose tolerance (IGT).
Subjects/Methods:
In the Study on Lifestyle intervention and Impaired glucose tolerance Maastricht, 147 Caucasian IGT subjects were randomized to an intervention group (INT: n=74; 38 male, 36 female) and control group (CON: n=73; 37 male, 36 female). Annually, subjects underwent measurements of body weight, anthropometry, glucose tolerance (oral glucose tolerance test), insulin resistance (homeostasis model assessment-insulin resistance), maximal aerobic capacity (VO2 max), blood lipids and blood pressure. INT received individual advice regarding a healthy diet and physical activity.
Results:
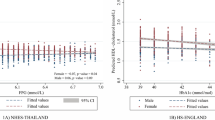
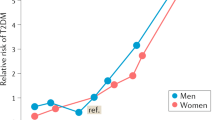
INT decreased their saturated fat intake, increased their carbohydrate intake (P<0.05) and VO2 max (P=0.04) compared with CON. Body weight did not change significantly (P=0.20) between the groups. After an initial decrease, 2-h glucose levels overall increased in INT (+0.11 mmol/l), but significantly less than CON (+1.18 mmol/l; P=0.04). Diabetes incidence was lower in INT versus CON (30 versus 56%, P=0.04). Change in body weight was associated with change in 2-h glucose levels (β=0.399 mmol/l per kg, P=0.02). Dropouts had a lower aerobic fitness and socioeconomic status, and a higher body mass index (BMI) and 2-h glucose compared with non-dropouts.
Conclusions:
Prolonged feasible changes in diet and physical activity prevent deterioration of glucose tolerance and reduce diabetes risk. Low socioeconomic status, low aerobic fitness and high BMI and 2-h glucose are indicative of dropout to the program.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Agardh E, Ahlbom A, Andersson T, Efendic S, Grill V, Hallqvist J et al. (2007). Socio-economic position at three points in life in association with type 2 diabetes and impaired glucose tolerance in middle-aged Swedish men and women. Int J Epidemiol 36, 84–92.
Ainsworth BE, Haskell WL, Leon AS, Jacobs Jr DR, Montoye HJ, Sallis JF et al. (1993). Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc 25, 71–80.
Ball K, Crawford D (2005). Socioeconomic status and weight change in adults: a review. Soc Sci Med 60, 1987–2010.
Eriksson J, Lindstrom J, Valle T, Aunola S, Hamalainen H, Ilanne-Parikka P et al. (1999). Prevention of type II diabetes in subjects with impaired glucose tolerance: the Diabetes Prevention Study (DPS) in Finland. Study design and 1-year interim report on the feasibility of the lifestyle intervention programme. Diabetologia 42, 793–801.
Gerstein HC, Yusuf S, Bosch J, Pogue J, Sheridan P, Dinccag N et al. (2006). Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: a randomised controlled trial. Lancet 368, 1096–1105.
Gillies CL, Abrams KR, Lambert PC, Cooper NJ, Sutton AJ, Hsu RT et al. (2007). Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. BMJ 334, 299.
Hamman RF, Wing RR, Edelstein SL, Lachin JM, Bray GA, Delahanty L et al. (2006). Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care 29, 2102–2107.
Ilanne-Parikka P, Eriksson JG, Lindstrom J, Peltonen M, Aunola S, Hamalainen H et al. (2008). Effect of lifestyle intervention on the occurrence of metabolic syndrome and its components in the Finnish Diabetes Prevention Study. Diabetes Care 31, 805–807.
Jacobs-van der Bruggen MA, Bos G, Bemelmans WJ, Hoogenveen RT, Vijgen SM, Baan CA (2007). Lifestyle interventions are cost-effective in people with different levels of diabetes risk: results from a modeling study. Diabetes Care 30, 128–134.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA et al. (2002). Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346, 393–403.
Lindstrom J, Ilanne-Parikka P, Peltonen M, Aunola S, Eriksson JG, Hemio K et al. (2006). Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet 368, 1673–1679.
Magliano DJ, Barr EL, Zimmet PZ, Cameron AJ, Dunstan DW, Colagiuri S et al. (2008). Glucose indices, health behaviors, and incidence of diabetes in Australia: the Australian Diabetes, Obesity and Lifestyle Study. Diabetes Care 31, 267–272.
Mensink M, Blaak EE, Corpeleijn E, Saris WH, de Bruin TW, Feskens EJ (2003a). Lifestyle intervention according to general recommendations improves glucose tolerance. Obes Res 11, 1588–1596.
Mensink M, Corpeleijn E, Feskens EJ, Kruijshoop M, Saris WH, de Bruin TW et al. (2003b). Study on lifestyle-intervention and impaired glucose tolerance Maastricht (SLIM): design and screening results. Diabetes Res Clin Pract 61, 49–58.
Morrato EH, Hill JO, Wyatt HR, Ghushchyan V, Sullivan PW (2007). Physical activity in US. Adults with diabetes and at risk for developing diabetes, 2003. Diabetes Care 30, 203–209.
Oldroyd JC, Unwin NC, White M, Mathers JC, Alberti KG (2006). Randomised controlled trial evaluating lifestyle interventions in people with impaired glucose tolerance. Diabetes Res Clin Pract 72, 117–127.
Roumen C, Corpeleijn E, Feskens EJ, Mensink M, Saris WH, Blaak EE (2008). Impact of 3-year lifestyle intervention on postprandial glucose metabolism: the SLIM study. Diabet Med 25, 597–605.
Simmons RK, Harding AH, Jakes RW, Welch A, Wareham NJ, Griffin SJ (2006). How much might achievement of diabetes prevention behaviour goals reduce the incidence of diabetes if implemented at the population level? Diabetologia 49, 905–911.
Swinburn BA, Metcalf PA, Ley SJ (2001). Long-term (5-year) effects of a reduced-fat diet intervention in individuals with glucose intolerance. Diabetes Care 24, 619–624.
Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P et al. (2001). Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344, 1343–1350.
Wendel-Vos GC, Schuit AJ, SarisWH, Kromhout D (2003). Reproducibility and relative validity of the short questionnaire to assess health-enhancing physical activity. J Clin Epidemiol 56, 1163–1169.
World Health Organization (1999). Report of a WHO consultation. Part 1: Diagnosis and Classification of Diabetes Mellitus. Definition, diagnosis and classification of diabetes mellitus. Geneva, Switzerland. Publication WHO/NCD/NCS/99.2.
Acknowledgements
We thank Jos Stegen, Tanja Hermans-Limpens and Marja Ockeloen-van der Hulst for their help during the oral glucose tolerance tests and with the dietary intervention. This work was supported by grants from the Dutch Diabetes Research Foundation (DFN 98.901 and 2000.00.020), the Netherlands Organization for Scientific Research (940-35-034 and 2200.0139).
Clinical trial on ClinicalTrials.gov: NCT00381186, submitted on September 25 2006.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Roumen, C., Feskens, E., Corpeleijn, E. et al. Predictors of lifestyle intervention outcome and dropout: the SLIM study. Eur J Clin Nutr 65, 1141–1147 (2011). https://doi.org/10.1038/ejcn.2011.74
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2011.74
Keywords
This article is cited by
-
Nutritional Aspects to Cardiovascular Diseases and Type 2 Diabetes Mellitus
Current Cardiology Reports (2024)
-
Socio-economic factors, mood, primary care utilization, and quality of life as predictors of intervention cessation and chronic stress in a type 2 diabetes prevention intervention (PREVIEW Study)
BMC Public Health (2023)
-
Digital health interventions to improve eating behaviour of people with a lower socioeconomic position: a scoping review of behaviour change techniques
BMC Nutrition (2022)
-
Effective elements of a combined lifestyle intervention for people with low socioeconomic status. A concept mapping case study
TSG - Tijdschrift voor gezondheidswetenschappen (2022)
-
Retention in group-based diabetes care programs: a multiple-case study design
Journal of Public Health (2022)