Abstract
Purpose
To compare the accuracy in measurement of the anterior chamber (AC) angle by anterior segment optical coherence tomography (AS-OCT) and ultrasound biomicroscopy (UBM) in European patients with suspected primary angle closure (PACS), primary angle closure (PAC), or primary angle-closure glaucoma (PACG).
Design
Cross-sectional study.
Methods
In all, 55 eyes of 33 consecutive patients presenting with PACS, PAC, or PACG were examined with AS-OCT, followed by UBM. The trabecular-iris angle (TIA) was measured in all four quadrants. The angle-opening distance (AOD) was measured at 500 μm from the scleral spur. The Bland–Altman method was used for assessing agreement between the two methods.
Results
The mean (±SD) superior TIA was 19.3±15.8° in AS-OCT and 15.7±15.0° in UBM (P=0.50) and inferior TIA was 17.9±12.9° (AS-OCT) and 16.7±14.1° (UBM) (P=0.71). The superior AOD500 was 0.17±0.16 mm in UBM and 0.21±0.16 mm in AS-OCT (P=0.06). Bland–Altman analysis showed a mean SD of±9.4° for superior and inferior TIA and a mean SD of ±0.10 mm for superior and inferior AOD500.
Conclusions
This comparative study shows that AS-OCT measurements are significantly correlated with UBM measurements but show poor agreement with each other. We do not believe that AS-OCT can replace UBM for the quantitative assessment of the AC angle.
Similar content being viewed by others
Introduction
Primary angle closure (PAC) and primary angle-closure glaucoma (PACG) are considered to be relatively uncommon entities in the Caucasian populations.1 PACG is a major form of glaucoma and a significant cause of blindness in the East and the South Asia.1, 2, 3 It is an aggressive form of glaucoma and may be associated with higher rates of blindness than primary open-angle glaucoma (POAG).4
The choice of the ideal diagnostic tool for detection of angle closure has been the subject of much debate and numerous studies. Traditionally, gonioscopy has been the reference standard of clinical assessment of the anterior chamber (AC) angle.5 This method requires a skilled clinician and is prone to significant inter-observer bias.5 Furthermore, it is not an ideal research-tool because of its semi-quantitative and subjective nature. Ultrasound biomicroscopy (UBM) has greatly enhanced the possibility of objective quantitative measurements of the anterior segment and has allowed reproducible imaging of the cross-sectional AC anatomy.6, 7, 8 It provides a 4 × 4-mm image of the anterior segment to a depth of 4 mm with a 50-μm resolution.
Anterior segment optical coherence tomography (AS-OCT) has recently been introduced as an alternative imaging modality to UBM.9, 10 It has a potential advantage over UBM in that it does not require a water bath. This renders the examination process more comfortable for the patient and reduces the examination time. Image acquisition can be performed by a technician with minimal experience. Several studies have evaluated quantitative measurement of the AC angle using AS-OCT.10, 11
A pilot study comparing the AS-OCT prototype to UBM in 17 normal and 14 narrow angle eyes showed good reproducibility between the two devices but found a tendency of UBM to give smaller measures when a statistical significance was present.11 Another trial that only looked at nasal and temporal iridocorneal angles of 63 normal eyes found good correlation for these parameters.12 The legitimation and aim of this study was to comprehensively compare the quantitative assessment of the anterior segment anatomy by UBM and the commercially available AS-OCT (Visante OCT) in European patients with primary angle-closure suspicion (PACS), PAC, and PACG as defined by Foster et al.13
Materials and methods
This was a prospective, non-randomized cross-sectional observational study. Fifty-five eyes of 33 consecutive patients diagnosed on gonioscopy to have suspected PAC (appositional contact between the peripheral iris and posterior trabecular meshwork on indentation gonioscopy, without raised IOP or peripheral anterior synechiae (PAS)), presenting as PAC (glaukomflecken, iris whorling, excessive pigment deposition on the trabeculum, and/or raised IOP) or PACG (with signs of glaucomatous optic neuropathy) at our clinic, were examined with AS-OCT followed by UBM at presentation. The diagnosis was further based on clinical history, slit lamp biomicroscopy, and visual field testing. The diagnosis was confirmed by a second glaucoma specialist (TS) using the same predetermined criteria. An individual was classified with angle-closure if one or more quadrants with iridotrabecular contact were found in either eye. Patients with evidence of PAS over 90° were excluded. Baseline measurements were made in constant darkness conditions. Measurement of the angle was made using AS-OCT software provided with the device by the manufacturer and UBM software (C 1, 1999) (Figure 1). The study was conducted in accordance with the tenets of the Declaration of Helsinki and informed patient consent was obtained before study inclusion.
Anterior segment optical coherence tomography
The AS-OCT device used in this study is the recently introduced commercial model (Zeiss Visante OCT Model 1000, Carl Zeiss Meditec, Dublin, CA, USA). The AS-OCT is a tomographical and biomicroscopical device with a resolution of 18 μm. The principle is based on low coherence interferometry using a 1.3 μm superluminescent light-emitting diode. The technology has been described earlier in more detail.9 With the patients in the sitting position, two images were acquired of each of the four quadrants. A single observer (KM) performed imaging on all subjects before UBM examination.
Ultrasound biomicroscopy
With the patient in supine position, UBM examinations were performed with the UBM Model 840 machine (Paradigm Medical Industries Inc., Salt Lake City, UT, USA) with a 50-MHz transducer probe. After topical anaesthesia with 0.4% oxybuprocaine in both eyes, a 22 or 24 mm eyecup was applied and filled with 2% methylcellulose as a coupling agent. A single observer (KM) performed and graded all examinations, which were subsequently reassessed by a second observer (TS).
Data analysis
The data were recorded prospectively. One of the two images of each quadrant was selected on the basis of centration, quality of the image, and visibility of the angle structures. The below mentioned parameters were measured twice and the average was used for the analysis. The trabecular-iris angle (TIA) was measured with the apex at the iris recess and the arms passing through the point on the meshwork 500 microns from the scleral spur and the point on the iris perpendicularly opposite. The angle-opening distance (AOD) as the distance between the corneal endothelium and the anterior iris surface was measured on a line perpendicular to the trabecular meshwork at 500 μm from the scleral spur (AOD500). (Figure 2) Data analysis was performed by the same examiner (KM) in an unmasked manner and was confirmed by another expert (TS) who was masked to image acquisition and patient history. The Bland–Altman method was used to measure agreement between the two devices.14
Results
All measurements were made in the superior (12 o'clock position), nasal, inferior (6 o'clock position), and temporal quadrants at each examination and under constant darkness conditions. A total of 55 eyes of 33 patients with PACS (29 eyes), PAC (16), or PACG (10) were enrolled consecutively in the study. Four patients (four eyes) had undergone earlier laser peripheral iridotomies (LPI) that had failed to relieve the appositional closure. The average age of the patients was 56.8±15.6 years (range: 19–83 years). Twenty-one (63%) patients were female. No patient experienced any undesired effects during the study period.
The mean superior TIA was 19.3±15.8° in AS-OCT and 15.7±15.0° in UBM (P=0.50) and inferior TIA was 17.9±12.9° (AS-OCT) and 16.7±14.1° (UBM) (P=0.17). Table 1 gives an overview of angle parameters measured by UBM and AS-OCT. Figures 3, 4, 5 and 6 show the images acquired. Another parameter, the AOD500 as the distance between the corneal endothelium and the anterior iris surface, was measured on a line perpendicular to the trabecular meshwork at 500 μm from the scleral spur and evaluated at the 12 o'clock and 6 o'clock positions. The superior AOD500 was 0.21±0.16 mm in AS-OCT and 0.17±0.16 mm in UBM (P=0.06). The inferior AOD500 was 0.20±0.15 mm (AS-OCT) vs 0.17±0.14 mm (UBM) (P=0.07).
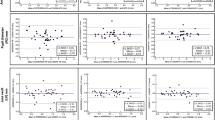
The statistical analysis using the Bland–Altman method is shown in Figure 7. Mean differences between TIA measures of the two methods were relatively small—between 0.2° (temporal quadrant) and 2.7° (superior quadrant), indicating a relatively small systematic offset between the two methods. The differences between the two TIA measures were, however, spread out over a range of about±20°, which means that large differences between the values measured by the two methods (up to 20°) were frequent, thus indicating poor agreement between the two methods for individual measurements. The analysis of AOD500 measures shows a similar picture. In addition, the systematic offset between the two methods seems to enlarge with increasing AOD values for the superior quadrant.
Discussion
The visualization and measurement of the AC angle is essential for the assessment of glaucoma patients and for the diagnosis and management of individuals with narrow and occludable angles. With LPI and argon laser iridoplasty, two efficient interventions against the development of angle closure glaucoma are available. AS-OCT is a new non-contact imaging technique with potential applications in glaucoma and refractive surgery. This trial aimed to assess its comparability to UBM for angle measurements in patients with PACS, PAC, and PAG.
In this study, AS-OCT measurements were significantly correlated with UBM measurements but showed poor agreement with high differences in quantifying AC angle in individuals with narrow or closed angles. Our findings are partially consistent with two other recently published papers comparing UBM with AS-OCT. These showed good reproducibility of angle measurements with both modalities. Dada et al12 only looked at two angles (nasal and temporal) of 63 normal eyes with AS-OCT and UBM and found a correlation coefficient of r=0.84 for the nasal and r=0.86 for the temporal angles. When we used the same analysis (Pearson's correlations), we obtained similar values of r=0.85 and r=0.84, respectively, in our study. Radhakrishnan et al11 compared an AS-OCT prototype to the UBM in a small group of seven subjects with narrow angles and found similar mean values, reproducibility, and sensitivity profiles between the devices. Their results, however, are not directly comparable to those of Dada et al and ours as they used different statistical methods and angle parameters, such as the trabecular-iris surface, angle recess area, and trabecular-iris contact length. However, the use of correlation coefficients in this setting is inappropriate and potentially misleading. Bland and Altman14 proposed an alternative approach based on geographical techniques and simple calculations, which has since been widely accepted as the appropriate method to estimate agreement of a new measurement technique with an established one.
In this study, the mean of the four angle measurements was slightly higher in the AS-OCT group (19.72 vs 17.43° with UBM). Analysis of the superior AOD500 showed that AS-OCT had a tendency to overestimate values with increasing AOD, which was not found for the inferior AOD500 (Figure 7). This finding was in contrast with our expectation that the supine position in UBM as well as inadvertent posterior pressure of the eyecup and immersion would produce a backward movement of the iris-ciliary diaphragm with a consecutive artificial widening of the angle.15 Radhakrishnan et al11 also observed that UBM tended to give smaller measurements than AS-OCT. They, however, hypothesized that the pressure of the eyecup may cause a narrowing of the angle. The literature does not provide a clear answer on the role of the pressure exercised by the eyecup.
Several authors have compared AS-OCT with gonioscopy as the reference standard and shown a higher correlation than gonioscopy in narrow angles with sensitivities of up to 98%.10, 16, 17, 18 However, as Nolan et al10 argue, gonioscopy may not be the right reference standard for assessing the performance of AS-OCT (and UBM). When they reversed the order, and used AS-OCT as the reference standard, Goldmann lens gonioscopy had a low sensitivity of only 68%.
High reproducibility of AS-OCT was confirmed by different researchers.19 Mueller et al showed low intra-observer and inter-observer variability in nine healthy volunteers.20 The intraclass correlation coefficient (ICC) was 0.94 and 0.91 for two observers measuring the AC angle. Another study evaluated the short- and long-term reproducibility of AC measurements of 43 patients for a single observer using the prototype AS-OCT.21 Their results showed excellent reproducibility for AC depth measurements (ICC 0.93–1.00) and for nasal and temporal angles (ICC 0.93) but only poor to good reproducibility for inferior angle measurements (ICC 0.56).
Ultrasound biomicroscopy has been commercially available since 1990 but has not become part of routine clinical practice. This is most likely because of the time-consuming nature, contact with the globe, and difficulty in manipulation. As a result, intra- and interobserver reproducibility varies considerably.22, 23 Another limitation of UBM seems to be its inability to distinguish clearly between iris-cornea apposition and iris-cornea adhesion or locate the posterior trabecular meshwork.24 Similar to UBM, the AS-OCT can visualize the scan position in real time and the fast scan speed (8 frames/s) allows the study of the dynamic dark–light changes of the AC angle configuration in detail and in a comparable field of view.25 Being a light-based system, its higher resolution (18 μm in Visante AS-OCT vs 25 μm in 50 MHz UBM) may be an advantage over UBM in very narrow or closed angles. It is, however, an optical technique in which refraction phenomena may distort the images and negatively influence the results.26 A major shortcoming of the AS-OCT in comparison with the UBM is its low tissue penetration. The UBM scans the AC through opaque corneas to a depth of about 4 mm, providing images of structures behind the iris and the ciliary body. With the AS-OCT, on the other hand, the pigmented posterior layer of the iris prevents infrared light transmission beyond this structure and the ciliary body and suprachoroidal space are not visualized.
A limitation of this study is the fact that the physician performing the UBM and AS-OCT was not masked to the patient's examination findings. This can be of some relevance as image processing using the current analysis software of both devices is based on subjective identification of anatomic landmarks. Therefore, the results can vary between different examiners. The scleral spur is a visible structure in UBM and AS-OCT and is used as a reference point for the calculation of various variables of the AC configuration. There is some consensus among published papers that the scleral spur is more easily identifiable with AS-OCT, although in our experience there was no difficulty with either method.12, 27 This fact could potentially signify better accuracy for OCT measurements when compared with UBM.
With the advent of AS-OCT, screening programmes for the diagnoses of angle closure in high prevalence populations may become more feasible. In contrast with UBM and gonioscopy, the new technique requires no contact, is well tolerated, rapid, easily practised by a technician, and data collection and analysis are simple to organize. The only currently available data on screening are from a hospital population in Singapore showing high sensitivity (98%) but low specificity (55.4%).10 The new device has yet to be validated as a reliable screening tool against gonioscopy and UBM in a large population-based survey.
In conclusion, we have shown good correlation of angle width determined by UBM and AS-OCT. However, large differences between UBM and AS-OCT values were frequent. In addition, the importance of visualization of the ciliary body for defining the mechanism of closure in PACS, PAC, and PACG should be emphasized. This can only be done with UBM. Therefore, UBM should be resorted to whenever there is ground for suspicion of a plateau iris configuration or retro-iridal processes. For these reasons, we do not believe that AS-OCT can replace UBM, which remains the gold standard for the quantitative measurement of angle parameters. It seems unlikely that either device would replace gonioscopy, which is still needed to distinguish appositional from synechial closure and to detect morphological angle anomalies such as pigment dispersion or neovascularization.
References
Quigley HA, Broman AT . The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 2006; 90 (3): 262–267.
Seah SK, Foster PJ, Chew PT, Jap A, Oen F, Fam HB et al. Incidence of acute primary angle-closure glaucoma in Singapore. An island-wide survey. Arch Ophthalmol 1997; 115 (11): 1436–1440.
Foster PJ, Baasanhu J, Alsbirk PH, Munkhbayar D, Uranchimeg D, Johnson GJ . Glaucoma in Mongolia. A population-based survey in Hovsgol province, northern Mongolia. Arch Ophthalmol 1996; 114 (10): 1235–1241.
Alsagoff Z, Aung T, Ang LP, Chew PT . Long-term clinical course of primary angle-closure glaucoma in an Asian population. Ophthalmology 2000; 107 (12): 2300–2304.
Makabe R . Comparative studies of the width of the anterior chamber angle using echography and gonioscopy. Klin Monatsbl Augenheilkd 1989; 194 (1): 6–9.
Pavlin CJ, Harasiewicz K, Foster FS . Ultrasound biomicroscopy of anterior segment structures in normal and glaucomatous eyes. Am J Ophthalmol 1992; 113 (4): 381–389.
Ishikawa H, Liebmann JM, Ritch R . Quantitative assessment of the anterior segment using ultrasound biomicroscopy. Curr Opin Ophthalmol 2000; 11 (2): 133–139.
Gazzard G, Friedman DS, Devereux JG, Chew P, Seah SK . A prospective ultrasound biomicroscopy evaluation of changes in anterior segment morphology after laser iridotomy in Asian eyes. Ophthalmology 2003; 110 (3): 630–638.
Radhakrishnan S, Rollins AM, Roth JE, Yazdanfar S, Westphal V, Bardenstein DS et al. Real-time optical coherence tomography of the anterior segment at 1310 nm. Arch Ophthalmol 2001; 119 (8): 1179–1185.
Nolan WP, See JL, Chew PT, Friedman DS, Smith SD, Radhakrishnan S et al. Detection of primary angle closure using anterior segment optical coherence tomography in Asian eyes. Ophthalmology 2007; 114 (1): 33–39.
Radhakrishnan S, Goldsmith J, Huang D, Westphal V, Dueker DK, Rollins AM et al. Comparison of optical coherence tomography and ultrasound biomicroscopy for detection of narrow anterior chamber angles. Arch Ophthalmol 2005; 123 (8): 1053–1059.
Dada T, Sihota R, Gadia R, Aggarwal A, Mandal S, Gupta V . Comparison of anterior segment optical coherence tomography and ultrasound biomicroscopy for assessment of the anterior segment. J Cataract Refract Surg 2007; 33 (5): 837–840.
Foster PJ, Aung T, Nolan WP, Machin D, Baasanhu J, Khaw PT et al. Defining ‘occludable’ angles in population surveys: drainage angle width, peripheral anterior synechiae, and glaucomatous optic neuropathy in east Asian people. Br J Ophthalmol 2004; 88 (4): 486–490.
Bland JM, Altman DG . Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1 (8476): 307–310.
Ishikawa H, Inazumi K, Liebmann JM, Ritch R . Inadvertent corneal indentation may cause artifactitious widening of the iridocorneal angle on ultrasound biomicroscopy. Ophthalmic Surg Lasers 2000; 31: 342–345.
Karandish A, Wirbelauer C, Haberle H, Pham DT . Reproducibility of goniometry with slitlamp-adapted optical coherence tomography. Ophthalmologe 2004; 101 (6): 608–613. German.
Wirbelauer C, Gochmann R, Pham DT . Imaging of the anterior eye chamber with optical coherence tomography. Klin Monatsbl Augenheilkd 2005; 222 (11): 856–862.
See JL, Chew PT, Smith SD, Nolan WP, Chan YH, Huang D et al. Changes in anterior segment morphology in response to illumination and after laser iridotomy in Asian eyes: an anterior segment OCT study. Br J Ophthalmol 2007; 91 (11): 1485–1489.
Leung CK, Cheung CY, Li H, Dorairaj S, Yiu CK, Wong AL et al. Dynamic analysis of dark-light changes of the anterior chamber angle with anterior segment OCT. Invest Ophthalmol Vis Sci 2007; 48 (9): 4116–4122.
Muller M, Dahmen G, Porksen E, Geerling G, Laqua H, Ziegler A et al. Anterior chamber angle measurement with optical coherence tomography: intraobserver and interobserver variability. J Cataract Refract Surg 2006; 32 (11): 1803–1808.
Radhakrishnan S, See J, Smith SD, Nolan WP, Ce Z, Friedman DS et al. Reproducibility of anterior chamber angle measurements obtained with anterior segment optical coherence tomography. Invest Ophthalmol Vis Sci 2007; 48 (8): 3683–3688.
Tello C, Liebmann J, Potash SD, Cohen H, Ritch R . Measurement of ultrasound biomicroscopy images: intraobserver and interobserver reliability. Invest Ophthalmol Vis Sci 1994; 35 (9): 3549–3552.
Urbak SF, Pedersen JK, Thorsen TT . Ultrasound biomicroscopy. II. Intraobserver and interobserver reproducibility of measurements. Acta Ophthalmol Scand 1998; 76 (5): 546–549.
Spaeth GL, Azuara-Blanco A, Araujo SV, Augsburger JJ . Intraobserver and interobserver agreement in evaluating the anterior chamber angle configuration by ultrasound biomicroscopy. J Glaucoma 1997; 6 (1): 13–17.
Ishikawa H . Anterior segment imaging for glaucoma: OCT or UBM? Br J Ophthalmol 2007; 91 (11): 1420–1421.
Koop N, Brinkmann R, Lankenau E, Flache S, Engelhardt R, Birngruber R . Optical coherence tomography of the cornea and the anterior eye segment. Ophthalmologe 1997; 94 (7): 481–486. German.
Sakata K, Sakata LM, Sakata VM, Santini C, Hopker LM, Bernardes R et al. Prevalence of glaucoma in a South Brazilian population: Projeto Glaucoma. Invest Ophthalmol Vis Sci 2007; 48 (11): 4974–4979.
Author information
Authors and Affiliations
Corresponding author
Additional information
The article was presented in part at the Second World Glaucoma Congress, Singapore, July 2007.
This article was partially supported by a special grant from The Sir Jules Thorn Charitable Overseas Trust.
Conflict of interest: None
Rights and permissions
About this article
Cite this article
Mansouri, K., Sommerhalder, J. & Shaarawy, T. Prospective comparison of ultrasound biomicroscopy and anterior segment optical coherence tomography for evaluation of anterior chamber dimensions in European eyes with primary angle closure. Eye 24, 233–239 (2010). https://doi.org/10.1038/eye.2009.103
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.103
Keywords
This article is cited by
-
Winkelblockglaukome
Die Ophthalmologie (2022)
-
Fibrin membrane pupillary-block glaucoma after uneventful cataract surgery treated with intracameral tissue plasminogen activator: a case report
BMC Ophthalmology (2012)
-
Anterior segment optical coherence tomography of acute primary angle closure
Graefe's Archive for Clinical and Experimental Ophthalmology (2010)