Abstract
Background
To evaluate the outcomes of combined viscotrabeculotomy–trabeculectomy in patients with refractory developmental glaucoma and to compare the success and complication rates with classical trabeculotomy–trabeculectomy procedure.
Patients and Methods
Patients who were selected for this study had cloudy corneas with a diameter of 13 mm or greater and with an initial intraocular pressure (IOP) of 27 mmHg or more, and they were divided into two groups. Group 1 consisted of 40 eyes of 24 patients who had undergone combined viscotrabeculotomy–trabeculectomy with a mean follow-up time of 55.6±18.4 months, and group 2 consisted of 35 eyes of 20 patients who had undergone classical trabeculotomy–trabeculectomy with a mean follow-up time of 57.2±19.0 months. Pre- and postoperative IOPs, mean antiglaucoma medication, mean corneal diameter, success rates, intra- and postoperative complications were compared between two groups.
Results
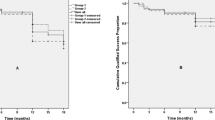
Mean IOP reduced from a preoperative level of 33.2±5.3 and 32.8 mmHg to 14.2±3.1 and 15.3±3.3 in group 1 and group 2, respectively (P<0.001). The mean number of antiglaucoma medications used after surgery was significantly lower in group 1 (P<0.05). Kaplan–Meier survival analysis showed that the success probability at the last visits was 90 and 71.4% in group 1 and group 2, respectively, and the difference was statistically significant (P=0.01). The most common early postoperative complication was transient IOP elevation in group 1 and hyphema in group 2 (for each, P<0.001).
Conclusion
Use of viscoelastic materials during trabeculotomy–trabeculectomy may increase the success rate of the procedure by prevention of postoperative hemorrhage, anterior chamber shallowing, adhesion of the incision lips or fibroblastic proliferation.
Similar content being viewed by others
Introduction
Congenital glaucoma is an uncommon, inherited abnormality of the trabecular meshwork that manifests itself during the first years of life with intraocular pressure (IOP) elevation, edema and enlargement of the cornea, and optic nerve damage. Management of the disease is surgical, and goniotomy or trabeculotomy ab externo are the classic procedures. Both surgical techniques are approximately equally effective with more than a 77% success rate.1, 2, 3, 4, 5 Goniotomy requires a transparent cornea for angle visibility and considerable surgical experience.5, 6 In contrast, trabeculectomy has also been shown to achieve adequate control of IOP in congenital glaucoma and several published reports have documented successful results following primary trabeculectomy for congenital glaucoma that are comparable to or are higher than the most reported series on goniotomy or trabeculotomy. The problems of goniotomy in children with hazy corneas, the advantages of trabeculotomy over goniotomy and encouraging reports of primary trabeculectomy in congenital glaucoma7, 8, 9, 10, 11, 12 prompted us to combine trabeculotomy ab externo with trabeculectomy during the initial surgery. In recent years, viscoelastic materials are used as multipurpose in ocular surgery. As viscoelastic materials separate or stabilize tissues, stop bleeding and protect the tissues against undesired damage, we considered that use of viscoelastics during combined trabeculotomy–trabeculectomy might increase the success rate by prevention of postoperative hemorrhage and fibroblastic proliferation, and adhesion of the incision lips, and we named this modified technique as combined viscotrabeculotomy–trabeculectomy.
This study evaluated the long-term results of combined viscotrabeculotomy–trabeculectomy and classical trabeculotomy–trabeculectomy, and compared the outcomes of these two techniques.
Patients and methods
Patient selection
The charts of 44 patients with refractory developmental glaucoma who underwent either combined viscotrabeculotomy–trabeculectomy (group 1) or classical combined trabeculotomy–trabeculectomy (group 2) between March 1993 and July 2005 were retrospectively reviewed. All patients were of Caucasian origin and had at least 3 years of follow-up. All procedures were performed at Istanbul University Cerrahpasa Medical Faculty, Department of Ophthalmology, and the local Ethics Committee of Cerrahpasa Medical Faculty approved the study. Informed written consent was obtained for all patients before operation. All parents were fully informed of the relative advantages and disadvantages of these two techniques, and selection of technique to be used in this series was determined by the preference of the patient's parents.
Group 1 consisted of 40 eyes of 24 patients who had undergone combined viscotrabeculotomy–trabeculectomy, and group 2 consisted of 35 eyes of 20 patients who had undergone classical trabeculotomy–trabeculectomy. Patients with a history of previous surgery or with secondary glaucoma were excluded from the study.
Diagnosis of congenital glaucoma was established by an examination under inhalation anesthesia using 1% halothane. Age, sex, family history, main presenting features, antiglaucoma medications, time of surgery, follow-up time, intra- and postoperative complications and success rates were all recorded. Pre- and postoperative examinations included measurement of IOP, biomicroscopy, determination of horizontal corneal diameters and funduscopy. IOP measurements were assessed with Perkins hand-held applanation tonometer in the early phase of inhalation anesthesia using 1% halothane.
Surgical technique
All surgeries were performed by the same surgeon (NT). Classical trabeculotomy–trabeculectomy was performed using a standardized technique similar to that described before.12 In viscotrabeculotomy–trabeculectomy, Schlemm's canal was cannulated with Grieshaber viscocanalostomy cannula on either side after performing radial incision and high viscosity sodium hyaluronate (Healon GV, Pfizer, NY, USA) was injected into the Schlemm's canal. An angled Harms trabeculotome was passed into the canal; the tip of the probe was gently rotated into the anterior chamber, and pulled back toward the incision. The probe was removed and the procedure was repeated in the opposite direction with the paired trabeculotome. Then, a little amount of high viscosity sodium hyaluronate was injected to prevent adhesion of incision lips and shallowing of anterior chamber. After the viscotrabeculotomy was completed, trabeculectomy was completed by removing the deeper block marked previously. A peripheral iridectomy was performed, and a little amount of sodium hyaluronate was injected into the anterior chamber. The triangular scleral flap was sutured with one 10/0 nylon suture; the conjunctiva was closed with absorbable suture. At the end of the procedure, one drop of antibiotic-corticosteroid preparation was instilled into the lower conjunctival sac, and a patch was applied on the eye.
Postoperatively, topical corticosteroids and cycloplegics were administered until there was a complete resolution of postoperative inflammation. Topical antibiotics were administered five times a day, tapered gradually over a 4-week period. In group 1, β-blockers were used two times for 4 days to control transient IOP elevation. The patients were examined two times during the first week, weekly during the first month, monthly during the first year, and then every 3 months.
Complete surgical success was determined by an IOP <18 mmHg under general anesthesia without medication or resurgery, with no progression of disc cupping or corneal diameter, and no devastating visual complications. Qualified success was defined as an IOP <18 mmHg with antiglaucomatous medication or transient ocular hypotony without visual loss. Failure was defined as IOP ⩾18 mmHg in patients with medication, resurgery, or sight-threatening complications. Transient hypotony was not considered a failure, but hypotony-related maculopathy was defined as a failure.
Statistical analysis
Results were presented as means ± SD and were analyzed statistically by using the Student t-test, two-way ANOVA, Kaplan–Meier survival plots and χ2 test as indicated. A P value <0.05 was considered statistically significant. Statistical analysis was performed with Statistical Package for the Social Sciences for Windows (SPSS/PC+ Inc., Release 10.0, Chicago, IL, USA).
Results
The characteristics of the patients are given in Table 1. All the patients were of Caucasian origin and had cloudy corneas with a diameter of 13 mm or greater and with an initial IOP of 27 mmHg or more. Axenfeld–Rieger syndrome was present in 9/40 eyes (22.5%) in group 1 and 7/35 eyes (20%) in group 2. The percentage of aniridia in group 1 was 12.5% (5 eyes) and 17.1% (6 eyes) in group 2. Seventeen patients (70.8%) in group 1 and 13 patients (65%) in group 2 underwent bilateral glaucoma surgery but in separate operative sessions.
The mean pre- and postoperative IOPs at 3, 12, 24, 36 months, and at the last visit with antiglaucoma medications, mean follow-up time, the success rates and the percentage of IOP reduction are shown in Table 2. There was no significant difference between two groups when preoperative mean IOPs, antiglaucoma medications and corneal diameters were compared (for each, P>0.05). Postoperatively, mean IOPs and antiglaucoma medications were significantly lower in group 1 (for each, P<0.05). Mean postoperative corneal diameter was significantly lower in both groups (for each, P<0.001), but there was no statistically significant difference between two groups (P>0.05). The percentage of mean reduction in IOP pressure from baseline to the last follow-up was 57.2% in group 1 and 53.3% in group 2. The success rates assessed by Kaplan–Meier survival analysis in group 1 at 3, 12, 24, 36 months and at the last visit were 92.5, 92.5, 90, 90 and 90%, respectively. In group 2, they were 77.1, 74.2, 71.4, 71.4 and 71.4%, respectively. At the last visits, the success rate of group 1 was statistically higher when compared with group 2 (P=0.01), and 9 eyes in group 1 and 12 eyes in group 2 required antiglaucoma medications to control IOP. As antiglaucoma medications, β-blockers, topical carbonic anhydrase inhibitors and prostaglandin analogs were used to control IOP. Additional surgery was performed in 4 eyes in group 1 and 10 eyes in group 2.
Complications encountered during surgery and in the postoperative period are listed in Table 3. The most common complication in the early postoperative period was hyphema in group 2 and transient IOP elevation in group 1, which was treated with antiglaucoma medications a few days (Table 4).
Discussion
IOP in congenital glaucoma is raised by developmental anomalies in the trabecular meshwork. The management is surgical and the outflow is enhanced by incising or cleaving the abnormal trabecular meshwork. The primary surgical procedures in congenital glaucoma are goniotomy or trabeculotomy. Goniotomy and trabeculotomy are approximately equally effective at controlling IOP.1, 2, 3, 4, 5, 6 The success rate of goniotomy and trabeculotomy is related with the age of the patient at the onset of glaucoma and types of abnormalities.13 When the signs and symptoms of glaucoma were present at birth or over 24 months, the success rate was close to 30%.6 It has been reported that the surgical results are more favorable if the operation is performed within the first 2 to 12 months of life.14, 15, 16 However, up to 50% of the population are reported to have varying degrees of corneal edema, rendering goniotomy technically impossible.17 Trabeculotomy ab externo is an alternative surgical technique that is possible even in the presence of severe corneal edema. The only disadvantage of trabeculotomy is that Schlemm's canal may not be found in 11–15% of procedures. This may be caused by surgical inexperience, abnormal anatomy, or hypoplasia of the canal.18, 19, 20 However, if the IOP is already elevated at birth or soon after, irreparable damage may have been done to the developing trabecular meshwork and Schlemm's canal, which cannot be reversed by trabeculotomy alone. Trabeculectomy then provides an additional pathway for outflow. A combined procedure of trabeculotomy–trabeculectomy might then be indicated for difficult cases. Compared with the European population, a large number of children in our country present with a severe cloudy cornea at birth. Poor socioeconomic status can lead these patients to present late and an advanced stage of the disease.
In this study, combined trabeculotomy–trabeculectomy was undertaken as the surgical procedure of primary choice because all of the patients are unsuitable for goniotomy. The technique of combined trabeculotomy–trabeculectomy offers many theoretical and practical advantages. It is less dependent on corneal clarity than goniotomy, provides an additional pathway for the outflow of aqueous through the trabeculectomy bleb site and trabeculotomy creates a direct continuity between the anterior chamber, Schlemm's canal and episcleral veins. Therefore, the combined procedure is superior to trabeculectomy alone in controlling the IOP even if one or the other pathway has failed to function. Technically, this procedure requires minimal extra surgical time over just trabeculotomy or just trabeculectomy and the complication rates are no different from either procedure on its own.10, 21
In recent years, viscoelastic materials have become a predominant element in the performance of ocular surgery. Viscoelastic materials are indispensable in the prevention of damage to ocular tissue and are also used as multipurpose tools in all surgical phases.22, 23 The term of viscosurgery was first introduced by Balazs and Denlinger,24 and one of the aims of this procedure is to accomplish the procedures and maneuvers during the surgery. In addition, viscoelastics separate or stabilize tissues, stop bleeding and protect the tissues against undesired damage.25, 26 The disadvantage of viscoelastic materials is that they not metabolized in the eye and will leave the anterior chamber through the trabeculum. Clearance of viscoelastic materials depends on the volume injected, the concentration and viscosity of the material and the amount left in the anterior chamber. When left in the anterior chamber or partly removed at the end of surgery, they can cause a temporary IOP elevation.27 In our study, a little amount of high viscosity sodium hyaluronate was injected into the Schlemm's canal on either side to prevent late bleeding and adhesion of the incision lips. Viscoelastic materials remain in the canal for 4 to 6 days, prevent collapse of the Schlemm's canal, and create a barrier to the migration of fibrinogen released by the ciliary body during surgery.28 As a result, polymerization of the fibrin to fibrinogen in the lake and Schlemm's canal was almost eliminated and remove the stimulus for fibroblastic proliferation. Moreover, prevention of adhesion of the incision lips or anterior chamber shallowing with sodium hyaluronate may decrease postoperative inflammation, limit the wound healing process and cicatrisation. Otherwise, the meshwork tissues may gradually overgrow the trabeculotomy site and this may explain some of the declining success with time. The only disadvantage of using viscoelastics may be transient IOP elevation that can be controlled with antiglaucoma medications in a few days.
The results of combined trabeculotomy–trabeculectomy procedures have been reported by several authors. Turut et al29 have used this procedure for infantile glaucoma with a similar success rate of 70%. Elder et al11 reported the success rate of combined trabeculotomy–trabeculectomy 93.5% after 24 months of follow-up. In another study by Mullaney et al,10 the success rate of combined trabeculotomy and trabeculectomy as an initial procedure in uncomplicated congenital glaucoma was found to be 78% after a mean follow-up period of 304 days. The success rates of this procedure reported by Mandal et al21 were 94.4, 90.9 and 81% in congenital, infantile and juvenile glaucoma, respectively. Campos-Mollo et al30 reported that cumulative probabilities of success, after performing combined trabeculotomy–trabeculectomy as the initial operative procedure, were 95.5% after 12 months and 78.2% after 24 months. To the best of our knowledge, this study is the first evaluating the long-term results of combined viscotrabeculotomy–trabeculectomy and classical trabeculotomy–trabeculectomy, and comparing the outcomes of these two techniques. In this study, the success rate of classical trabeculotomy–trabeculectomy at the last visits was 71.4 and 90% of viscotrabeculotomy–trabeculectomy, and the difference between the two groups was statistically significant. This may be explained by prevention of postoperative hemorrhage or fibroblastic proliferation, nontraumatic cannulation of Schlemm's canal after dilation with viscoelastic material, keeping away the lips of trabeculotomy incision, and prevention of anterior chamber shallowing, which has important functions in decreasing anterior chamber inflammation and retarding wound healing process.
The most common early postoperative complication was transient IOP elevation in group 1 (32.5%). The incidence of hyphema in group 1 was only 5% in the early postoperative period. These low rates of hyphema may only be explained by using viscoelastic materials in group 1. Viscoelastic materials may prevent bleeding because they form a physical barrier and concentrate coagulation factors at the site of bleeding to achieve hemostasis. Prevention of bleeding from incision lips may, therefore, decrease the inflammation and risk of adhesion of incision lips, and also may increase the success rate. In addition, viscomaterials may facilitate cannulation of Schlemm's canal by maintaining a stable and larger canal, provide a safe and convenient tissue incision and stable anterior chamber.
This study has several limitations. First, it is a non-randomized retrospective study with a rather limited number of patients. Second, a non-masked examiner performed clinical examinations. Therefore, this study may serve as a pilot study reporting the clinical outcome of the patients undergoing combined viscotrabeculotomy–trabeculectomy surgery. However, the follow-up time was relatively long that allowing conclusions on the final outcome of both procedures, and anatomical and functional results were apparent during the follow-up time.
In conclusion, we think that viscotrabeculotomy–trabeculectomy is safer and more effective than classical trabeculotomy–trabeculectomy. Dilation of the possibly narrow Schlemm's canal, keeping away the lips of trabeculotomy incision, possibly prevention of the postoperative hemorrhage, fibroblastic proliferation prevention and anterior chamber shallowing by means of high viscosity sodium hyaluronate are the possible factors that have important functions in overall success of this procedure. However, studies with larger numbers and longer follow-up are required to determine the role of this procedure in congenital glaucoma.
Conflict of interest
The authors declare no conflict of interest.
References
Dickens CJ, Hoskin HD . Diagnosis and treatment of congenital glaucoma. In: Ritch R, Shields MB, Krupin T (eds) The Glaucomas. ST Louis: CV Mosby, 1996, pp 739–749.
Khaw PT, Freedman S, Gandolfi S . Management of congenital glaucoma. J Glaucoma 1999; 8: 81–85.
Papadopoulos M, Khaw PT . Advances in the management of paediatric glaucoma. Eye 2007; 21: 1319–1325.
Ozkiris A, Tamcelik N . Long-term results of trabeculectomy with different concentrations of mitomycin C in refractory developmental glaucoma. J Pediatr Ophthalmol Strabismus 2005; 42: 97–102.
Tamcelik N, Ozkiris A . A comparison of viscogoniotomy with classical goniotomy in Turkish patients. Jpn J Ophthalmol 2004; 48: 404–407.
Shaffer RN . Prognosis of goniotomy in primary infantile glaucoma. Trans Am Ophthalmol Soc 1982; 80: 321–325.
Rao KV, Sai CM, Babu BVN . Trabeculectomy in congenital glaucoma. Indian J Ophthalmol 1984; 32: 439–440.
Burke JP, Bowell R, Grehn F . Primary trabeculectomy in congenital glaucoma. Br J Ophthalmol 1989; 73: 186–190.
Mandal AK, Prasad K, Naduvilath TJ . Surgical results and complications of mitomycin C-augmented trabeculectomy in refractory developmental glaucoma. Ophthalmic Surg Lasers 1999; 30: 473–480.
Mullaney PB, Selleck C, Al-Awad A, Al-Mesfer S, Zwaan J . Combined trabeculotomy and trabeculectomy as an initial procedure in uncomplicated congenital glaucoma. Arch Ophthalmol 1999; 117: 457–460.
Elder MJ . Combined trabeculotomy-trabeculectomy compared with primary trabeculectomy for congenital glaucoma. Br J Ophthalmol 1994; 78: 745–748.
Tamcelik N, Ozkiris A . Long-term results of viscotrabeculotomy in congenital glaucoma: comparison to classical trabeculotomy. Br J Ophthalmol 2008; 92: 36–39.
Elder MJ . Congenital glaucoma in the West Bank and Gaza Strip. Br J Ophthalmol 1993; 77: 413–416.
Alsheikheh A, Klink J, Klink T, Steffen H, Grehn F . Long-term results of surgery in childhood glaucoma. Graefes Arch Clin Exp Ophthalmol 2007; 245: 195–203.
Ikeda H, Ishigooka H, Muto T, Tanihara H, Nagata M . Long-term outcome of trabeculotomy for the treatment of developmental glaucoma. Arch Ophthalmol 2004; 122: 1122–1128.
Mandal AK, Gothwal VK, Bagga H, Nutheti R, Mansoori T . Outcome of surgery on infants younger than 1 month with congenital glaucoma. Ophthalmology 2003; 110: 1909–1915.
Luntz MH . The advantages of trabeculotomy over goniotomy. J Pediatr Ophthalmol Strabismus 1984; 21: 150–153.
Quigley HA . Childhood glaucoma: results with trabeculotomy and study of reversible cupping. Ophthalmology 1982; 89: 219–226.
McPherson Jr SD, Berry DP . Goniotomy vs external trabeculotomy for developmental glaucoma. Am J Ophthalmol 1983; 95: 427–431.
Harms H, Dannheim R . Epicritical consideration of 300 cases of trabeculotomy ab externo. Trans Ophthalmol Soc UK 1970; 89: 491–449.
Mandal AK, Naduvilath TJ, Jayagandan A . Surgical results of combined trabeculotomy-trabeculectomy for developmental glaucoma. Ophthalmology 1998; 105: 974–982.
Silver FH, LiBrizzi J, Benedetto D . Use of viscoelastic solutions in ophthalmology: a review of physical properties and long-term effects. J Long Term Eff Med Implants 1992; 2: 49–66.
Goa KL, Benfield P . Hyaluronic acid. A review of its pharmacology and use as a surgical aid in ophthalmology, and its therapeutic potential in joint disease and wound healing. Drugs 1994; 47: 536–566.
Balazs EA, Denlinger JL . Clinical uses of hyaluronan. Ciba Found Symp 1989; 143: 265–275.
Maar N, Graebe A, Schild G, Stur M, Amon M . Influence of viscoelastic substances used in cataract surgery on corneal metabolism and endothelial morphology: comparison of Healon and Viscoat. J Cataract Refract Surg 2001; 27: 1756–1761.
Wild GJ, Kent AR, Peng Q . Dilation of Schlemm's canal in viscocanalostomy: comparison of 2 viscoelastic substances. J Cataract Refract Surg 2001; 27: 1294–1297.
Rainer G, Menapace R, Findl O, Georgopoulos M, Kiss B, Petternel V . Intraocular pressure after small incision cataract surgery with Healon5 and Viscoat. J Cataract Refract Surg 2000; 26: 271–276.
Johnson DH, Johnson M . How does nonpenetrating glaucoma surgery work? Aqueous outflow resistance and glaucoma surgery. J Glaucoma 2001; 10: 55–67.
Turut P, Ribstein G, Milazzo S, Madelain J . Combined trabeculotomy and trabeculectomy in primary congenital glaucoma. Bull Soc Ophtalmol Fr 1988; 88: 1021–1024.
Campos-Mollo E, Moral-Cazalla R, Belmonte-Martínez J . Combined trabeculotomy-trabeculectomy as the initial surgical procedure of primary developmental glaucoma. Arch Soc Esp Oftalmol 2008; 83: 479–486.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tamcelik, N., Özkiris, A. & Sarici, A. Long-term results of combined viscotrabeculotomy–trabeculectomy in refractory developmental glaucoma. Eye 24, 613–618 (2010). https://doi.org/10.1038/eye.2009.185
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.185
Keywords
This article is cited by
-
Combined trabeculotomy-trabeculectomy using the modified Safer Surgery System augmented with MMC: its long-term outcomes of glaucoma treatment in Asian children
Graefe's Archive for Clinical and Experimental Ophthalmology (2018)
-
Tenon advancement and duplication technique to prevent postoperative Ahmed valve tube exposure in patients with refractory glaucoma
Japanese Journal of Ophthalmology (2013)