Abstract
Purpose
To study the relationship between retinal nerve fiber layer (RNFL) thickness measurements from time domain (Stratus) and spectral domain (Cirrus HD) optical coherence tomography (OCT) in subjects with optic neuritis.
Methods
A total of 18 patients who had suffered monocular acute optic neuritis were imaged by a single trained operator using the Stratus-OCT (fast RNFL scan mode) and Cirrus HD-OCT (optic disc cube mode) on the same day. The relationship between RNFL thickness measurements of the two OCTs (overall and by quadrants) were evaluated using intraclass correlation coefficient (ICC) and Bland–Altman plots. Comparisons between eyes having optic neuritis (ON-group) and fellow eyes (fellow-group) were assessed by a generalized estimating equation (GEE) regression model.
Results
For Stratus-OCT, the median average RNFL was 86.3 and 102 μ in the ON-group and in the fellow-group, respectively. For Cirrus-OCT, the corresponding measurements were 81 and 93 μ. Average RNFL thickness as determined by the two OCT devices was well correlated in the ON-group (ρ=0.906, P<0.001) and in the fellow-group (ρ=0.702, P=0.001). The median signal strength was significantly higher with Cirrus-OCT. Bland–Altman plots showed that Stratus RNFL measurements were larger than Cirrus-OCT, but smaller when average RNFL thickness was very thin (≤56 μ).
Conclusions
Although the Cirrus-OCT and Stratus-OCT RNFL thickness measurements are well correlated in patients with optic neuritis, RNFL measurements cannot be directly compared. Clinicians should be aware that measurements are generally higher with Stratus- than with Cirrus-OCT.
Similar content being viewed by others
Introduction
Optical coherence tomography (OCT) is a high-resolution imaging device that applies the principle of interferometry to acquire in vivo measurements of retinal nerve fiber layer (RNFL) thickness.1
The third-generation instrument, Stratus-OCT (Carl-Zeiss Meditec, Inc., Dublin, CA, USA) relies on time-domain technology. Newer versions of OCT use spectral-domain technology, such as the Cirrus HD-OCT (Carl-Zeiss Meditec, Inc.). These OCTs offer faster scan speed and higher image resolution for RNFL imaging than conventional time-domain OCT.2
Several studies have focused on the measurements and reproducibility of RNFL thickness using Stratus-OCT after optic neuritis (ON) and multiple sclerosis (MS).3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13 In fact, lower RNFL values correlate with impaired visual function. OCT is a promising tool for evaluating atrophy in patients with ON and MS, and it could evolve into an important primary or secondary outcome measure for MS clinical trials and patient care.8, 14, 15 In such case, the different measurements provided by these two OCTs devices should be considered.
Recently, some studies have compared the RNFL measurement agreement between Cirrus HD-OCT and Stratus-OCT in glaucoma patients.16, 17, 18, 19, 20, 21, 22 To our knowledge no previous studies have been published comparing the RNFL thickness in patients having ON with Stratus-OCT and Cirrus HD-OCT. The purpose of this study was to compare the RNFL measurements using Stratus-OCT and Cirrus HD-OCT in patients who had a previous episode of monocular ON to identify any differences.
Methods
Participants
Patients with a single previous episode of unilateral ON seen from January 2004 to July 2008 at the Neuro-Ophthalmology Department of Ramon y Cajal Hospital were invited to participate in this study.
The diagnosis of typical ON was on the basis of clinical criteria, including visual loss in the affected eye, presence of a relative afferent pupillary defect, a visual field defect and pain that increased with eye movement. Inclusion criteria were the presence of an acute, unilateral episode of ON at least 6 months before the beginning of the study, no signs or symptoms of a previous episode in either eye and aged between 18 and 45.
Exclusion criteria were presence of an ocular pathology other than ON, intraocular pressure higher than 21 mm Hg and a refractive error greater than 5.0 diopters (D) of spherical equivalent or 3.0 D of astigmatism in either eye.
All participants gave their informed consent to be included in the study according to the declaration of Helsinki. The study was approved by the hospital ethics committee.
All patients who met the study criteria underwent a complete ophthalmological evaluation including snellen visual acuity (VA) testing, biomicroscopy of the anterior and posterior segments, intraocular pressure measurement and visual field testing with Humphrey field analyzer (HFA) using 24-2 Swedish Interactive Threshold Algorithm (SITA) standard strategy (Carl-Zeiss Meditec).
Patients were randomly scanned with both, Cirrus-HD and Stratus-OCT, on the same day by one trained operator (GA).
Optical coherence tomography
For the Stratus-OCT (software version, 4.0), the Fast RNFL 3.4 scan protocol was used. It consists of a series of three consecutive 3.46-mm diameter circumpapillary scans, with 256 A-scans taken over 1.92 s. All poor-quality scans were excluded, defined as those with signal strength of <6, decentration of the measurement circle location assessed subjectively or images with horizontal eye motion observed within the measurement circle.
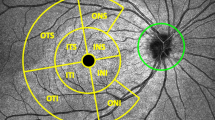
For the Cirrus HD-OCT (software version 3.0) the acquisition rate is 27000 A-scans per second, nearly 70 times faster than time-domain technology. The protocol used was the Optic Disk Cube 2. It generates a cube obtained from a three-dimensional data set composed of 200 A-scans from each of 200 B-scans that cover a 6-mm2 area. The software automatically determined the center of the disc and then extracted a circumpapillary circle (3.46 mm in diameter) from the cube data set for RNFL thickness measurement. We used the same signal-strength cutoff value as for the Stratus-OCT, and we excluded scans with movement artifacts.
Both OCT technologies provide average RNFL thickness measurements overall and by quadrants (superior, inferior, nasal, and temporal) and 12 h, including classification by an internal normative database. For both OCTs, normative classification consisted of four categories: the 95th to 100th percentiles were hypernormal (white color on thickness map); 5th to 95th percentiles were normal (green); 1st to 5th percentiles were borderline (yellow); and <1st percentiles was abnormal (red). Right-hand orientation was used for documentation of clock-hour measurements, so that 9 o'clock represents the temporal side of the optic disc for both right and left eyes. For this study, we have considered as abnormal both red and yellow categories.
All analyses were performed using the Statistical Package SPSS 15.0 for Windows (SPSS Inc., Chicago, IL, USA). Of the three scans taken for each, the one with the best signal score and least motion artifact was chosen as the single best scan.
All results were considered from non-parametric variables and were expressed by the formula median±interquartile range.
Comparisons between the ON-group and the fellow-group were made by a generalized estimating equation (GEE) regression model because data cannot be considered completely independent as both groups belong to the same patient. The percentage of eyes with abnormal RNFL thickness (as determined by the two OCTs) was compared using Cohen's kappa coefficient.
The relationships between the two OCTs measurements were assessed by Spearman's correlation analysis. Intraclass correlation coefficient (ICC) was also used to compare the Cirrus and Stratus RNFL measurements. A Bland–Altman plot was graphed to assess the agreement between the two instruments.
P-value less than 0.05 was considered statistically significant.
Results
A total of 22 Caucasian patients (7 males and 15 females) who had unilateral ON were enrolled in this study and imaged with Stratus- and Cirrus-OCT. Four eyes were finally excluded from the study owing to the poor image quality. Two of these eyes had signal strengths of <6 (one of them in Cirrus and the other one in Stratus) and two eyes had horizontal eye motion within the Cirrus measurement circle.
Table 1 summarizes clinical and demographical characteristics of the subjects. The median age was 39. Median time lapsed from the ON was 2.5 years. Median visual acuity (VA) was significantly worse in ON-eyes than in fellow-eyes (P=0.001). ON-eyes had significantly lower average RNFL thickness than fellow-eyes using both Stratus- and Cirrus-OCT (P=0.001).
The median signal strength was significantly higher with Cirrus-OCT (median: 9) than with Stratus (median signal 8) (P=0.002).
The respective median average RNFL thicknesses measured by Stratus-OCT and Cirrus-OCT were 86.3 μ (76–104.8) and 81 μ (72.5–93) for the ON-group and 102 μ (95–114.9) and 93.5 μ (86.5–106) for the fellow-eye group (P=0.001) (Table 1).
The average and quadrant RNFL thicknesses obtained from Cirrus HD-OCT were less than those obtained with Stratus-OCT (Table 2) in both groups, except in the nasal and temporal quadrant of ON-group.
The RNFL thickness measured by Stratus-OCT and Cirrus-OCT were significantly correlated in all quadrants and average thicknesses (except in the temporal quadrant of the fellow-eyes group) (Table 2, Figure 1). In the ON-group the best correlation between measurements was found in the average thickness (ρ=0.906; P<0.001) and in the nasal quadrant thickness (ρ=0.836; P<0.001). These correlations were weaker in temporal, superior, and inferior quadrants. Similar results were found in the fellow-eye group (Table 2).
The ICCs for the average, superior, inferior, nasal, and temporal RNFL thicknesses were 0.831, 0.613, 0.593, 0.765, and 0.609 in the ON-group and 0.623, 0.646. 0.544, 0.712, and 0.403 in the fellow-group, respectively.
Considering yellow and red colors as abnormal, Cirrus HD-OCT classified higher percentage of ON-eyes as having abnormal average thickness (44.4%) than Stratus-OCT (38.8%). The κ coefficient obtained between both OCTs was 0.889.
Figure 2 shows the Bland–Altman plots evaluating the agreement of RNFL measurements obtained with Cirrus HD-OCT and Stratus-OCT in ON-eyes. The Stratus measurements are higher than Cirrus at thicker RNFL values but smaller at thinner RNFL values.
Bland–Altman plots of agreement between Stratus-OCT and Cirrus-OCT for the average, superior, inferior, temporal, and nasal quadrants. The difference between both instruments is plotted against the average of both devices. The line of equality (solid) is plotted with the 95% limits of agreement (dashed).
Discussion
The widespread use of the OCT in the assessment of the optic nerve has revolutionized management and understanding of neuro-ophthalmic diseases. Cettomai et al13 demonstrated that mean RNFL thickness in patients with MS can be reproducibly measured by trained technicians using the OCT-3 model. They found excellent agreement with respect to interrater (ICC, 0.89), intrarater (ICC, 0.98), and intervisit (ICC, 0.91) results. The development of new OCT technologies such as the Cirrus HD spectral-domain OCT, with better resolution and reproducibility18 give us a new useful device for daily clinical practice. However, the appearance of a new technology also implies the need of assessing its correlation with previous existing technologies. Several studies have evaluated the agreement between Cirrus- and Stratus-OCT measurements in normal patients and patients with glaucoma,16, 17, 18, 19, 20, 21, 22 nevertheless to our knowledge no previous studies have been published comparing RNFL thickness in patients with ON scanned with Stratus-OCT and Cirrus-OCT.
As previously reported,4, 5, 6, 7, 8, 9, 10, 11, 12 ON-eyes had significantly lower average RNFL thickness than fellow-eyes using both Stratus- and Cirrus-OCT (P=0.001).
The results of this study demonstrate that Cirrus RNFL measurements correlate well with those from Stratus-OCT in patients with ON. However, the measurements obtained were different. These measurements are generally higher with Stratus than with Cirrus, except when the RNFL is very thin. In fact, when average thicknes was ≤56 μ, Cirrus gave a higher value compared with Stratus.
Although the patterns of RNFL loss are different in ON compared with other diseases such as glaucoma, with the highest degree of RNFL loss in the temporal quadrant,10, 23 our findings are similar to that previously observed in glaucoma patients.
Knight et al16 reported a systematic difference in measurement values between the two instruments. Cirrus measured thinner at thicker RNFL values and thicker at thinner glaucomatous RNFL values. Therefore, the difference is not in a single direction. In fact, in the ON-group, the nasal and temporal RNFL thicknesses obtained from Cirrus HD-OCT were 3.2 and 1 μ, respectively, thicker than that obtained with Stratus-OCT.
Considering both groups, the average and the nasal quadrant had the stronger correlation between the Cirrus and Stratus-OCT RNFL thickness measurements (Table 2). However, in glaucoma patients, Sung et al17 found that the correlations were weaker in the nasal quadrant. Differences in the distribution of RNFL damage between glaucoma and ON might explain these differences. In fact, RNFL thickness in patients with ON and/or MS is thinner than in controls, particularly in the temporal quadrant.23, 24 Rebolleda et al25 evaluated 50 patients after unilateral ON by Stratus-OCT and they found a significant inverse correlation between the C/D ratios asymmetry and RNFL thickness, mainly in the temporal quadrant. In this study, measurements are higher with Cirrus than Stratus at thinner RNFL values (Figure 2). According to this finding, the median temporal quadrant RNFL thicknesses in ON-group obtained from Cirrus HD-OCT (55 μ) was higher than those obtained with Stratus-OCT (54 μ) (Table 2).
Although this study demonstrates that RNFL thickness measurements in ON scanned with Stratus-OCT correlate well with those from Cirrus-OCT, it does not mean that the measurements are the same. As reported in previous studies with normal and glaucomatous patients, RNFL thickness measurements are generally higher with Stratus.
There are several possible explanations for the differences observed. The two instruments use different scan registration technologies, algorithms, data processing, and analysis. Moreover, segmentation algorithm is different; Cirrus aims to identify the bottom of the fiber layer, whereas Stratus attemps to localize the top of the ganglion cell layer.16 Each patient was scanned by one examiner on the same two instruments on the same day. In the same environment it was more difficult to obtain the same signal-scored images with the Cirrus-OCT than the Stratus-OCT. In fact, three of the four eyes were excluded owing to the poor image quality with Cirrus-OCT. However, in cases with signal strength ≥6, the median signal strength was higher with Cirrus-OCT than with Stratus-OCT (P=0.002). This finding has been previously mentioned by other authors in glaucoma patients.20
Cirrus-OCT assigned more ON-eyes as abnormal based on internal normative database (44.4 vs 38%). This might be because of the higher scan resolution and more accurate data registration of this instrument. Because there is no external validation for measurements taken from either instrument, it is not possible to know which instrument is more accurate.
Limitations of this study include the use of a small population of patients having a single ON episode. Imaging patients having MS or several episodes of ON might result in different outcome in terms of RNFL thickness differences.
OCT is evolving into an important primary or secondary outcome metric for MS clinical trials and patient care.26 OCT's advancement into spectral domain refined its ability to measure RNFL by increasing scanner speed. If refining the retinal segmentation algorithm to define RNFL better produces lower RNFL values, each newer generation instrument may find their RNFL values to be lower than the current version. Clinicians should be aware that there are systematic differences between the two instruments. From a clinical point of view, patients who are part of clinical trials that require a high degree of consistency with RNFL thickness measurements may not be able to interchange between Stratus- and Cirrus-OCT. Perhaps, in the case of switching from Stratus- to Cirrus-OCT technology, the best strategy for switching from one to the other during the follow-up of a patient may be to perform a follow-up Stratus scan to determine whether there has been a change from prior Stratus scans and then perform a new baseline scan with Cirrus for future comparison.10
In conclusion, our findings show that RNFL thickness measurements by Cirrus HD-OCT and Stratus-OCT were different in patients having ON, although the two measurements were well correlated. Stratus measurements are generally higher than Cirrus, except at thinner RNFL values. Further work is needed to establish the role of the Cirrus-OCT in the detection and monitoring of ON-eyes and patients with MS in comparison with the conventional Stratus-OCT.

References
Huang D, Swanson EA, Lin CP, Schuman JS, Stinson WG, Chang W et al. Optical coherence tomography. Science 1991; 254: 1178–1181.
Wojkowski M, Leitgeb R, Kowalczyk A, Bajraszewski T, Fercher AF . In vivo human retinal imaging by Fourier domain optical coherence tomography. J Biomed Opt 2002; 7: 457–463.
Trip SA, Schlottmann PG, Jones SJ, Li WY, Garway-Heath DF, Thompson AJ et al. Retinal nerve fiber layer axonal loss and visual dysfunction in optic neuritis. Ann Neurol 2005; 58: 383–391.
Noval S, Contreras I, Rebolleda G, Muñoz-Negrete FJ . Optical coherence tomography versus automated perimetry for follow-up of optic neuritis. Acta Ophthalmol Scand 2006; 84: 790–794.
Noval S, Contreras I, Rebolleda G, Muñoz-Negrete FJ . Optical coherence tomography in optic neuritis. Ophthalmology 2007; 114: 200.
Costello F, Coupland S, Hodge W, Lorello GR, Koroluk J, Pan YI et al. Quantifying axonal loss after optic neuritis with optical coherence tomography. Ann Neurol 2006; 59: 963–969.
Fisher JB, Jacobs DA, Markowitz CE, Galetta SL, Volpe NJ, Nano-Schiavi ML et al. Relation of visual function to retinal nerve fiber layer thickness in multiple sclerosis. Ophthalmology 2006; 113: 324–332.
Kallenbach K, Frederiksen J . Optical coherence tomography in optic neuritis and multiple sclerosis: a review. Eur J Neurol 2007; 14: 841–849.
Trip SA, Schlottmann PG, Jones SJ, Garway-Heath DF, Thompson AJ, Plant GT et al. Optic nerve atrophy and retinal nerve fibre layer thinning following optic neuritis: evidence that axonal loss is a substrate of MRI-detected atrophy. Neuroimage 2006; 31: 286–293.
Toledo J, Sepulcre J, Salinas-Alaman A, García-Layana A, Murie-Fernandez M, Bejarano B et al. Retinal nerve fiber layer atrophy is associated with physical and cognitive disability in multiple sclerosis. Mult Scler 2008; 14: 906–912.
Frohman EM, Dwyer MG, Frohman T, Cox JL, Salter A, Greenberg BM et al. Relationship of optic nerve and brain conventional and non-conventional MRI measures and retinal nerve fiber layer thickness, as assessed by OCT and GDx: a pilot study. Neurol Sci 2009; 282: 96–105.
Siger M, Dziegielewski K, Jasek L, Bieniek M, Nicpan A, Nawrocki J et al. Optical coherence tomography multiple sclerosis: thickness of the retinal nerve fiber layer as a potential measure of axonal loss and brain atrophy. J Neurol 2008; 255: 1555–1560.
Cettomai D, Pulicken M, Gordon-Lipkin E, Salter A, Frohman TC, Conger A et al. Reproducibility of optical coherence tomography in multiple sclerosis. Arch Neurol 2008; 65: 1218–1222.
Frohman EM, Fujimoto JG, Frohman TC, Calabresi PA, Cutter G, Balcer LJ et al. Optical coherence tomography: a window into the mechanisms of multiple sclerosis. Nat Clin Pract Neurol 2008; 4: 664–675.
Sergott RC, Frohman E, Glanzman R, Al-Sabbagh A . The role of optical coherence tomography in multiple sclerosis: expert panel consensus. Neurol Sci 2007; 263: 3–14.
Knight OJ, Chang RT, Feuer WJ, Budenz DL . Comparison of retinal nerve fiber layer measurements using time domain and spectral domain optical coherent tomography. Ophthalmology 2009; 116: 1271–1277.
Sung KR, Kim DY, Park SB, Kook MS . Comparison of retinal nerve fiber layer thickness measured by Cirrus HD and Stratus optical coherence tomography. Ophthalmology 2009; 116: 1264–1270.
Leung CK, Cheung CY, Weinreb RN, Qiu K, Liu S, Li H et al. Retinal nerve fiber layer imaging with spectral-domain optical coherence tomography: a variability and diagnostic performance study. Ophthalmology 2009; 116: 1257–1263.
Vizzeri G, Weinreb RN, Gonzalez-Garcia AO, Bowd C, Medeiros FA, Sample PA et al. Agreement between spectral-domain and time-domain OCT for measuring RNFL thickness. Br J Ophthalmol 2009; 93: 775–781.
Moreno-Montañes J, Olmo N, Alvarez A, García N, Zarranz-Ventura J . Cirrus high-definition optical coherence tomography compared to stratus optical coherence tomography in glaucoma diagnosis. Invest Ophthalmol Vis Sci 2010; 51: 335–343.
Chang RT, Knight OR, Feuer WJ, Budenz DL . Sensitivity and specificity of time-domain versus spectral-domain optical coherence tomography in diagnosing early to moderate glaucoma. Ophthalmology 2009; 116: 2294–2299.
Kim JS, Ishikawa H, Gabriele ML, Wollstein G, Bilonick RA, Kagemann L et al. Retinal nerve fiber layer thickness measurement comparability between time domain optical coherence tomography (OCT) and spectral domain OCT. Invest Ophthalmol Vis Sci 2010; 51: 896–902.
Bock M, Brandt AU, Dörr J, Kraft H, Weinges-Evers N, Gaede G et al. Patterns of retinal nerve fiber layer loss in multiple sclerosis patients with or without optic neuritis and glaucoma patients. Clin Neurol Neurosurg 2010; 112: 647–652.
Sepulcre J, Murie-Fernandez M, Salinas-Alaman A, García-Layana A, Bejarano B, Villoslada P . Diagnostic accuracy of retinal abnormalities in predicting disease activity in MS. Neurology 2007; 68: 1488–1494.
Rebolleda G, Noval S, Contreras I, Arnalich-Montiel F, García-Perez JL, Muñoz-Negrete FJ . Optic disc cupping after optic neuritis evaluated with optic coherence tomography. Eye 2009; 23: 890–894.
Subei AM, Eggenberger ER . Optical coherence tomography: another useful tool in a neuro-ophthalmologist's armamentarium. Curr Opin Ophthalmol 2009; 20: 462–466.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Rebolleda, G., García-García, A., Won Kim, H. et al. Comparison of retinal nerve fiber layer measured by time domain and spectral domain optical coherence tomography in optic neuritis. Eye 25, 233–238 (2011). https://doi.org/10.1038/eye.2010.206
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2010.206
Keywords
This article is cited by
-
Anatomical and functional retinal changes in multiple sclerosis
Eye (2016)
-
Optical coherence tomography measurements in compressive optic neuropathy associated with dysthyroid orbitopathy
Graefe's Archive for Clinical and Experimental Ophthalmology (2016)