Abstract
Purpose
Recent evidence has suggested a correlation between reduced vitamin D levels and delayed angiogenesis and reduced inflammatory response, which are known to have a major role in the development and progression of age-related macular degeneration (AMD).
Design
Cross-sectional study.
Participants
Members of the Maccabi Healthcare Services (MHS, one of the four largest Israeli Health Maintenance Organization) aged ≥60 years, whose vitamin D levels were taken as part of routine examinations between 2000 and 2008.
Methods
All data for this study were obtained from MHS databases that include medical information on 1.8 million subscribers.
Main outcome measures
Serum 25-OH vitamin D levels.
Results
The total study population comprised of 1045 members diagnosed as having AMD, and 8124 as non-AMD, for whom there was information on vitamin D levels. The mean±SD level of 25-OH vitamin D was 24.1±9.41 ng/ml (range 0.8–120) for the AMD patients and 24.13±9.50 ng/ml (range 0.0–120) for the controls (P=ns). One-third (33.6%) of the AMD patients and 32.86% of the controls had a 25-OH vitamin D level <16 ng/ml, and the proportions of tests in which the 25-OH vitamin D level was >74 ng/ml were 0.19 and 0.14%, respectively (P=ns)
Conclusions
No association was detected between vitamin D levels and the presence of AMD in this cross-sectional study. These results raise some doubt about an association between reduced vitamin D levels and the prevalence of AMD.
Similar content being viewed by others
Introduction
Age-related macular degeneration (AMD) is the leading cause of legal blindness among people in the western world.1
High-dose antioxidants have been shown to slow progression from intermediate to late AMD.1 Several potential risk factors for the development and progression of AMD have been identified, such as age,2 cigarette smoking,3 hypertension2 and family history of the disease.4 Other potential risk factors associated less consistently in previous studies include sunlight exposure2, 5 and diets low in lutein and zeaxanthin,6, 7 or diets high in fats.8, 9
The pathogenesis of AMD is not fully understood, but it is well established that angiogenesis has a major role in the development and progression of AMD.10 Inflammation has recently received some attention as a potential risk factor for AMD.11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22 Immunological changes seemed to be related to early pathological changes in retinal pigment epithelial (RPE) and drusen formation. Immune components, including immunoglobulins, complement factors and fibrinogen, have been observed to be entrapped within drusen.11, 12, 13, 14, 16 Evidence of inflammatory cell involvement in the later stages of AMD includes the presence of multinucleated giant cells and leukocytes in the choroid of AMD eyes15 and in excised choroidal neovascularization.20, 22 A number of in vitro and in vivo studies have suggested an anti-inflammatory role for vitamin D.23, 24 It was also shown that vitamin D reduces the proliferation of cells of the immune system,25, 26, 27, 28, 29 and that there is an inverse relationship between vitamin D levels and several chronic conditions associated with inflammation.30, 31, 32, 33 Owing to the potential causative role of inflammation in AMD development and progression, it is possible that vitamin D may protect against the occurrence and progression of AMD by virtue of its anti-inflammatory properties. Furthermore, it was recently shown that vitamin D was a potent inhibitor of angiogenesis by its effects on endothelial cells34 and by interrupting signaling pathways that are key to angiogenesis, specifically in tumorigenesis.35, 36
The primary purpose of this study was to examine the relationship between serum vitamin D levels and AMD. We hypothesized that individuals in the highest quintile of serum vitamin D levels would have a lower prevalence of AMD compared with those in the lowest quintile.
Materials and methods
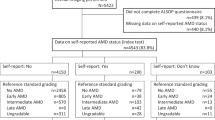
This cross-sectional study was carried out in Maccabi Healthcare Services (MHSs), a 1.8 million enrollee health maintenance organization operating in Israel. It was approved by the MHS institutional review board. All the data were obtained from the MHS's automated databases, that were used to retrieve information on biochemistry results, and medical diagnoses using the international classification of diseases 9 (ICD-9). Included in the study were MHS members aged 60 or above, that have had their vitamin D test between 2000 and 2008 as part of a routine exam. For each eligible patient, information on age at vitamin D test, sex and past diagnoses of AMD, diabetes mellitus and hypertension were collected from the electronic medical files using a unique nine-digit personal number. AMD was identified by the presence of the following ICD-9 codes: unspecified macular degeneration (senile) of retina, non-exudative senile macular degeneration of retina, exudative senile macular degeneration of retina.
Serum data
Serum 25-hydroxyvitamin D was measured as part of the member's routine examination with no relation to suspected or confirmed AMD. The level was determined by collecting approximately 100 ml of whole blood in evacuated containers. Serum specimens were immediately frozen at −70°C and subsequently used to estimate serum vitamin D levels within 2 weeks of collection.37 In Israel, estimation of serum 25-hydroxyvitamin D in humans is regularly carried out with the LIAISON 25 OH Vitamin D TOTAL assay38 (now DiaSorin Inc., Stillwater, MN, USA) based on a radioimmunoassay method. Values of vitamin D are usually described in quintiles: a level of <16 ng/ml indicates deficiency, a level between 17 and 73 ng/ml is considered as being sufficient and a level ≥74 ng/ml is indicative of vitamin D toxicity. The standard deviation is 9% and it is calculated as coefficient of variation (CV−SD/mean × 100).
Statistical analysis
The χ2-test for categorical variables and the t-test for comparing averages were performed to determine significant differences in baseline characteristics between AMD and non-AMD patients. Pearson's correlation was used to measure the association between vitamin D levels and age. Statistical significance was considered when P<0.05.
Results
The total study population of 9167 was comprised of 1045 AMD and 8124 non-AMD subjects, which represents 12.5% of the AMD patients and 9.5% of the non-AMD patients in MHS. The participants’ characteristics are summarized in Table 1. Compared with the non-AMD study participants, AMD patients were more likely to be older (77.7 vs 76.0, P<0.01). Both study groups, had a comparable sex distribution and a similar prevalence of DM and hypertension.
Mean serum levels of 25-hydroxyvitamin D correlated negatively with age ranging from above 26 ng/ml in subjects aged 60–69 to less than 22 in elderly aged 85 or above (Figure 1), which suggest a bi-variate correlation of −0.136 ng/ml per increase of 1 year of age (P<0.01). Similar trends were found in men and women. The mean 25-OH vitamin D levels for the AMD patients and the controls are provided in Table 2. Vitamin D levels were 24.1±9.41 ng/ml for the former and 24.13±9.50 ng/ml for the latter (P=0.925). The proportion of tests in which the 25-OH vitamin D level was below the normal limit (<16 ng/ml) was 33.6% for the AMD patients and 32.86% for the controls (P=0.642). When we examined the proportion of tests in which the 25-OH vitamin D level was higher than the normal laboratory limit (>74 ng/ml), it emerged that 0.19% of the AMD patients had vitamin D level >74 ng/ml compared with 0.14% of the controls (P=0.987).
Discussion
We had hypothesized that AMD patients would have lower levels of vitamin D compared with non-AMD subjects, basing our expectations on several putative mechanisms supporting the anti-inflammatory properties of vitamin D as well as its anti-angiogenic properties. The evidence we accumulated from our data on a large number of AMD patients failed to support any association between vitamin D levels and the prevalence of AMD, as the MHS members with AMD had 25-OH vitamin D levels similar to those of non-AMD controls. The relatively large number of AMD patients in our study allowed a statistical power of 80% to detect an OR of at least 1.3 for AMD among patients with low vitamin D level, and 99% power to detect an OR of at least 1.5. Therefore, it is unlikely that our negative results are explained by type II error.
Several studies have reported that vitamin D decreases the proliferation of T-helper cells,23 T-cytotoxic cells and natural killer cells24 and enhances T-suppressor cell activity.31 Other studies have reported that vitamin D also decreases the production of proinflammatory agents, such as IL-2,25, 26 IL-8,27 IL-628 and IL-12.29 One recent study demonstrated that vitamin D intake reduces C-reactive protein, a marker of systemic inflammation.33
Dramatic advances have been made in unraveling the biological bases of AMD, implicating chronic local inflammation and activation of the complement cascade in the pathogenesis of the condition.16, 17 A number of complement system proteins, complement activators and complement regulatory proteins were identified as molecular constituents of drusen, the hallmark extracellular deposits associated with early AMD12, 39, 40, 41, 42 and of geographic atrophy and choroidal neovascularization, the hallmark of advanced AMD.43 Genetic studies revealed highly significant associations between AMD and variants of several complement pathway-associated genes, including complement factor H, complement factor H-related 1 and 3, complement factor B, complement component 2 and complement component 3.39, 40, 41, 42, 44 Associations between markers of inflammation (such as C-reactive protein) and AMD have been observed in some45, 46 but not all47 previous epidemiological studies. Results of the Beaver Dam Eye Study indicated an association between histories of gout and emphysema, two diseases associated with inflammation, and intermediate and late stages of AMD.31
A comprehensive review by Zarbin18 described several concepts relevant to the cell biology of AMD. One especially relevant concept was that in AMD (and perhaps in aging), injury to the RPE and, possibly, choriocapillaris results in a chronic inflammatory response within the bruch membrane and the choroid and that this inflammation leads to formation of an abnormal extracellular matrix (ECM), which causes altered diffusion of nutrients to the retina and RPE, possibly precipitating further RPE and retinal damage. The abnormal ECM results in altered RPE-choriocapillaris behavior, leading ultimately to atrophy of the retina, RPE, and the choriocapillaris and to choroidal new vessel growth. Inflammation clearly has a major role in AMD pathogenesis in such a sequence of events.
Vitamin D might protect against AMD by virtue of its antiangiogenic properties. Vitamin D is a potent inhibitor of angiogenesis by its effects on endothelial cells34, 35, 36 and by interrupting signaling pathways that are key to angiogenesis, specifically in tumorigenesis. Vitamin D is provided by some foods and is also generated endogenously on exposure to sunlight. The serum levels of 25-hydroxyvitamin D that were assessed in this study reflected the cumulative quantity of vitamin D from all sources.
Parekh et al48 evaluated the associations between levels of vitamin D (25-hydroxyvitamin D) in serum and prevalent AMD in a large population based cross-sectional study. They found that levels of serum vitamin D were inversely associated with early AMD but not advanced AMD. When they evaluated associations of early and late AMD with important food and supplemental sources of vitamin D, they found that milk intake was inversely associated with early AMD (OR, 0.75; 95% CI, 0.6–0.9) and that fish intake was inversely associated with advanced AMD (OR, 0.41; 95% CI, 0.2–0.9).
Other studies evaluated the association of fish intake (a major source of vitamin D) to AMD and found that higher fish intake was associated with a lower risk of AMD development and progression.8, 9, 49, 50
This cross-sectional study found that higher vitamin D levels are not associated with decreased prevalence of AMD, as expected by the above evidence.
We found that vitamin D levels were inversely associated with age (Figure 1). This finding was also demonstrated in a large cross-sectional study, investigating the association between 25(OH)D levels with all-cause, cancer and cardiovascular disease (CVD) mortality in 13 331 nationally representative adults 20 years or older from the Third National Health and Nutrition Examination Survey.51 In cross-sectional multivariate analyses, they found that increasing age, female sex, non-white race/ethnicity, diabetes, current smoking and higher body mass index were all independently associated with higher odds of 25(OH)D deficiency (lowest quartile of 25(OH)D level ≤17.8 ng/ml). They found that in the general United States population, 25(OH)D deficiency (lowest quartile ≤17.8 ng/ml) was associated with a 26% higher risk of all-cause mortality, independent of baseline demographics, traditional and non-traditional CVD risk factors, and measures of a healthy lifestyle. The estimated association with increased risk of CVD mortality was similar, though not statistically significant. No association was found with cancer mortality or other causes of death.
Several potential limitations of our study must be considered before drawing any conclusions from the results. We did not estimate the food and supplement intake of the patients or the amount of sun exposure, the lack or excess of which could have affected the results. As in many cross-sectional studies, the recorded serum 25-hydroxyvitamin D values would reflect sun exposure and food intake over recent weeks, rather than years, a feature that would have increased the random measurement error. However, we do not believe that this potential non-differential misclassification of exposure has biased the reported associations toward the null, as a pervious study from Israel has shown that sun exposure carries only a small and insignificant effect on the variation in vitamin D levels between seasons.52
Cases of AMD were defined by diagnostic codes according to ICD-9 without detailed clinical data (eg, retinal pigment epithelial depigmentation, size and type of drusen and so on), which were unavailable. Therefore, no distinctions were made between early and late AMD, and we were not able to examine any associations of serum vitamin D levels and the advanced form of AMD, which are meaningful, given the antiangiogenic properties of vitamin D. Several important differences between the findings of our study and those of other population-based studies on this issue6 may lie in the fact that we did not examine the amount of sun exposure of the patients, a factor that could have a great impact on the results measured.
Another explanation for the difference could be the level of awareness to the value of supplement intake by both the AMD patients and the controls, as we do not have any data on the percentage of AMD patients who take vitamin supplements (vitamin D in particular). Finally, our results could be influenced by a large percentage of the MHS membership who takes supplement vitamin D for other medical conditions (osteomalacia, osteoporosis and so on)
Also, the categorization values of vitamin D used to determine deficiency is not definite, although it is widely agreed that 25(OH)D <15 ng/ml (or <37.5 nmol/l) is generally considered inadequate.53
However, this relatively high cutoff value may have masked effects of more severe hypovitaminosis D.
In conclusion, this study, which was conducted on a large, representative sample of the Israeli population, provides no evidence for inverse associations between AMD and serum vitamin D levels, as we had expected from the findings of others. Our results warrant reconsidering the existence of an association between vitamin D and the occurrence and progression of AMD.

References
Age-Related Eye Disease Study Research Group. A randomized, placebo controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol 2001; 119: 1417–1436.
Klein R, Peto T, Bird A, Vannewkirk MR . The epidemiology of age-related macular degeneration. Am J Ophthalmol 2004; 137: 486–495.
Mitchell P, Wang JJ, Smith W, Leeder SR . Smoking and the 5-year incidence of age-related maculopathy: the Blue Mountains Eye Study. Arch Ophthalmol 2002; 120: 1357–1363.
Klein ML, Mauldin WM, Stoumbos VD . Heredity and age-related macular degeneration: observations in monozygotic twins. Arch Ophthalmol 1994; 112: 932–937.
Taylor HR, West S, Muñoz B, Rosenthal FS, Bressler SB, Bressler NM . The longterm effects of visible light on the eye. Arch Ophthalmol 1992; 110: 99–104.
Mares J . Carotenoids and eye disease: epidemiologic evidence. In: Krinsky NI, Mayne S (eds). Carotenoids in Health and Disease. Marcel Dekker Inc: New York, NY, 2003, p 19.
Mares-Perlman JA, Millen AE, Ficek TL, Hankinson SE . The body of evidence to support a protective role for lutein and zeaxanthin in delaying chronic disease. J Nutr 2002; 132: 518S–524S.
Mares-Perlman JA, Brady WE, Klein R, VandenLangenberg GM, Klein BE, Palta M . Dietary fat and age-related maculopathy. Arch Ophthalmol 1995; 113: 743–748.
Seddon JM, Rosner B, Sperduto RD, Yannuzzi L, Haller JA, Blair NP et al. Dietary fat and risk for advanced agerelated macular degeneration. Arch Ophthalmol 2001; 119: 1191–1199.
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY, et al. MARINA Study Group. Ranibizumab for neovascular age related macular degeneration. N Engl J Med 2006; 355 (14): 1419–1431.
Johnson LV, Ozaki S, Staples MK, Erickson PA, Anderson DH . A potential role for immune complex pathogenesis in drusen formation. Exp Eye Res 2000; 70: 441–449.
Johnson LV, Leitner WP, Staples MK, Anderson DH . Complement activation and inflammatory processes in Drusen formation and age related macular degeneration. Exp Eye Res 2001; 73: 887–896.
Anderson DH, Mullins RF, Hageman GS, Johnson LV . A role for local inflammation in the formation of drusen in the aging eye. Am J Ophthalmol 2002; 134: 411–431.
Hageman GS, Luthert PJ, Victor Chong NH, Johnson LV, Anderson DH, Mullins RF . An integrated hypothesis that considers drusen as biomarkers of immune-mediated processes at the RPE–Bruch's membrane interface in aging and age-related macular degeneration. Prog Retin Eye Res 2001; 20: 705–732.
Dastgheib K, Green W . Granulomatous reaction to Bruch's membrane in age related macular degeneration. Arch Ophthalmol 1994; 112: 813–818.
Anderson DH, Radeke MJ, Gallo NB, Chapin EA, Johnson PT, Curletti CR et al. The pivotal role of the complement system in aging and age related macular degeneration: hypothesis re-visited. Prog Retin Eye Res 2010; 29: 95–112.
Augustin AJ, Kirchhof J . Inflammation and the pathogenesis of age related macular degeneration. Expert Opin Ther Targets 2009; 13: 641–651.
Zarbin MA . Current concepts in the pathogenesis of age-related macular degeneration. Arch Ophthalmol 2004; 122: 598–614.
Smith W, Mitchell P, Leeder SR, Wang JJ . Plasma fibrinogen levels, other cardiovascular risk factors, and age-related maculopathy: the Blue Mountains Eye Study. Arch Ophthalmol 1998; 116: 583–587.
Seregard S, Algvere PV, Berglin L . Immunohistochemical characterization of surgically removed subfoveal fibrovascular membranes. Graefes Arch Clin Exp Ophthalmol 1994; 232: 325–329.
Klein R, Klein BE, Tomany SC, Cruickshanks KJ . Association of emphysema, gout, and inflammatory markers with long-term incidence of age-related maculopathy. Arch Ophthalmol 2003; 121: 674–678.
Hutchinson AK, Grossniklaus HE, Capone A . Giant-cell reaction in surgically excised subretinal neovascular membrane. Arch Ophthalmol 1993; 111: 734–735.
Topilski I, Flaishon L, Naveh Y, Harmelin A, Levo Y, Shachar I . The anti-inflammatory effects of 1,25-dihydroxyvitamin D3 on Th2 cells in vivo are due in part to the control of integrin-mediated T lymphocyte homing. Eur J Immunol 2004; 34: 1068–1076.
Thomasset M . Vitamin D and the immune system [in French]. Pathol Biol (Paris) 1994; 42: 163–172.
Manolagas SC, Provvedini DM, Murray EJ, Tsoukas CD, Deftos LJ . The antiproliferative effect of calcitriol on human peripheral blood mononuclear cells. J Clin Endocrinol Metab 1986; 63: 394–400.
Müller K, Gram J, Bollerslev J, Diamant M, Barington T, Hansen MB et al. Down-regulation of monocyte functions by treatment of healthy adults with 1 alpha,25 dihydroxyvitamin D3. Int J Immunopharmacol 1991; 13: 525–530.
Takahashi K, Horiuchi H, Ohta T, Komoriya K, Ohmori H, Kamimura T . 1 Alpha,25-dihydroxyvitamin D3 suppresses interleukin-1beta-induced interleukin-8 production in human whole blood: an involvement of erythrocytes in the inhibition. Immunopharmacol Immunotoxicol 2002; 24: 1–15.
Lefebvre d’Hellencourt C, Montero-Menei CN, Bernard R, Couez D . Vitamin D3 inhibits proinflammatory cytokines and nitric oxide production by the EOC13 microglial cell line. J Neurosci Res 2003; 71: 575–582.
D’Ambrosio D, Cippitelli M, Cocciolo MG, Mazzeo D, Di Lucia P, Lang R et al. Inhibition of IL-12 production by 1,25-dihydroxyvitamin D3: involvement of NF-kappaB downregulation in transcriptional repression of the p40 gene. J Clin Invest 1998; 101: 252–262.
Holick MF . Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr 2004; 79: 362–371.
Hayes CE, Nashold FE, Spach KM, Pedersen LB . The immunological functions of the vitamin D endocrine system. Cell Mol Biol (Noisy-le-grand) 2003; 49: 277–300.
Merlino LA, Curtis J, Mikuls TR, Cerhan JR, Criswell LA, Saag KG . Vitamin D intake is inversely associated with rheumatoid arthritis: results from the Iowa Women's Health Study. Arthritis Rheum 2004; 50: 72–77.
Timms PM, Mannan N, Hitman GA, Noonan K, Mills PG, Syndercombe-Court D et al. Circulating MMP9, vitamin D and variation in the TIMP-1 response with VDR genotype: mechanisms for inflammatory damage in chronic disorders? Q J Med 2002; 95: 787–796.
Bernardi RJ, Johnson CS, Modzelewski RA, Trump DL . Antiproliferative effects of 1alpha,25-dihydroxyvitamin D(3) and vitamin D analogs on tumor-derived endothelial cells. Endocrinology 2002; 143: 2508–2514.
Shokravi MT, Marcus DM, Alroy J, Egan K, Saornil MA, Albert DM . Vitamin D inhibits angiogenesis in transgenic murine retinoblastoma. Invest Ophthalmol Vis Sci 1995; 36: 83–87.
Iseki K, Tatsuta M, Uehara H, Iishi H, Yano H, Sakai N et al. Inhibition of angiogenesis as a mechanism for inhibition by 1alpha-hydroxyvitamin D3 and 1,25-dihydroxyvitamin D3 of colon carcinogenesis induced by azoxymethane in Wistar rats. Int J Cancer 1999; 81: 730–733.
Gunter EWLB, Koncikowski SM . Laboratory Procedures Used for the Third National Health and Nutrition Examination Survey, 1988-1994: NHANES III Reference Manuals and Reports. Centers for Disease Control and Prevention: Hyattsville, MD, 1996.
25-hydroxyvitamin D 125I RIA kit instruction manual (68100E). DiaSorin Inc.: Stillwater, MN, 2004.
Hageman GS, Anderson DH, Johnson LV, Hancox LS, Taiber AJ, Hardisty LI et al. A common haplotype in the complement regulatory gene factor H (HF1/CFH) predisposes individuals to age-related macular degeneration. Proc Natl Acad Sci USA 2005; 102: 7227–7232.
Despriet DD, Klaver CC, Witteman JC, Bergen AA, Kardys I, de Maat MP et al. Complement factor H polymorphism, complement activators, and risk of age-related macular degeneration. JAMA 2006; 296: 301–309.
Zareparsi S, Branham KE, Li M, Shah S, Klein RJ, Ott J et al. Strong association of the Y402H variant in complement factor H at 1q32 with susceptibility to age-related macular degeneration. Am J Hum Genet 2005; 77: 149–153.
Klein RJ, Zeiss C, Chew EY, Tsai JY, Sackler RS, Haynes C et al. Complement factor H polymorphism in age-related macular degeneration. Science 2005; 308: 385–389.
Sepp T, Khan JC, Thurlby DA, Shahid H, Clayton DG, Moore AT et al. Complement factor H variant Y402H is a major risk determinant for geographic atrophy and choroidal neovascularization in smokers and nonsmokers. Invest Ophthalmol Vis Sci 2006; 47: 536–540.
Gorin MB . A clinician's view of the molecular genetics of age-related maculopathy. Arch Ophthalmol 2007; 125: 21–29.
Seddon JM, George S, Rosner B, Rifai N . Progression of age-related macular degeneration: prospective assessment of C-reactive protein, interleukin 6, and other cardiovascular biomarkers. Arch Ophthalmol 2005; 123: 774–782.
Seddon JM, Gensler G, Milton RC, Klein ML, Rifai N . Association between C-reactive protein and age-related macular degeneration. JAMA 2004; 291: 704–710.
Klein R, Klein BE, Marino EK, Kuller LH, Furberg C, Burke GL et al. Early age-related maculopathy in the cardiovascular health study. Ophthalmology 2003; 110: 25–33.
Parekh N, Chappell RJ, Millen AE, Albert DM, Mares JA . Association between vitamin D and age-related macular degeneration in the Third National Health and Nutrition Examination Survey, 1988 through 1994. Arch Ophthalmol 2007; 125 (5): 661–669.
Seddon JM, Cote J, Rosner B . Progression of age-related macular degeneration f: association with dietary fat, transunsaturated fat, nuts, and fish intake. Arch Ophthalmol 2003; 121 (12): 1728–1737.
Seddon JM, George S, Rosner B . Cigarette smoking, fish consumption, omega-3 fatty acid intake, and associations with age-related macular degeneration: the US Twin Study of Age Related Macular Degeneration. Arch Ophthalmol 2006; 124 (7): 995–1001.
Melamed ML, Michos ED, Post W, Astor B . 25-hydroxyvitamin D levels and the risk of mortality in the general population. Arch Intern Med 2008; 168 (15): 1629–1637.
Tandeter H, Grynbaum M, Zuili I, Shany S, Shvartzman P . Serum 25-OH vitamin D levels in patients with fibromyalgia. Isr Med Assoc J 2009; 11: 339–342.
National Institutes of Health, Office of Dietary Supplements. Dietary Supplement Fact Sheet: Vitamin D, 2011.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Golan, S., Shalev, V., Treister, G. et al. Reconsidering the connection between vitamin D levels and age-related macular degeneration. Eye 25, 1122–1129 (2011). https://doi.org/10.1038/eye.2011.174
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.174
Keywords
This article is cited by
-
Serum 25-hydroxy vitamin D levels in age-related macular degeneration
International Journal of Retina and Vitreous (2022)
-
A systematic review of vitamin D status in southern European countries
European Journal of Nutrition (2018)
-
Vitamin D status and prevalent early age-related macular degeneration in African Americans and Caucasians: The Atherosclerosis Risk in Communities (ARIC) Study
The Journal of nutrition, health and aging (2017)
-
Vitamin D and Diabetic Complications: True or False Prophet?
Diabetes Therapy (2016)