Abstract
Aims
Anti-vascular endothelial growth factor compounds are routinely used for the treatment of diabetic macular edema (DME). We aim to evaluate for the existence and magnitude of treatment effect on fellow un-injected eyes.
Methods
A consecutive group of patients with bilateral DME who received unilateral bevacizumab injections was retrospectively evaluated. Data collected included demographics, ophthalmic and systemic findings, and optical coherence tomography (OCT) measurements of macular thickness.
Results
Thirty-five patients were evaluated. Mean follow-up was 245 days (range: 30–800), and the mean number of bevacizumab injections was 3.6 (range: 1–11). At end of follow-up, the mean (SD) OCT central subfield thickness reduced by 72±112 micron in the injected eye (from 469±139 to 397±120 micron; P=0.001), while in the non-injected eye it reduced by 49±75 micron (from 380±130 to 331±106 micron; P<0.001). Sixteen injected eyes (45.7%) showed central subfield thickness reduction of ≥50 micron while 10 (28.6%) non-injected eyes showed such thickness reduction. Improved VA following treatment was detected in 14 (40%) injected eyes and in 15 (43%) non-injected eyes.
Conclusions
Unilateral bevacizumab injections in patients with bilateral DME are often associated with bilateral response.
Summary Statement
Anti-vascular endothelial growth factor compounds are routinely used for the treatment of diabetic macular edema (DME). In this retrospective study, we show that unilateral bevacizumab injections often result in reduction of the macular thickness in the fellow un-injected eye.
Similar content being viewed by others
Introduction
Recent randomized clinical trials have demonstrated the efficacy, tolerability, and safety of intravitreal anti-vascular endothelial growth factor (VEGF) therapy in eyes with diabetic macular edema (DME) and have shown that the benefit is maintained for >2 years.1, 2, 3, 4 Based on these trials, a pro re nata (PRN) bevacizumab or ranibizumab treatment with monthly monitoring with or without a loading dosage of 3–4 monthly injections is usually used for DME.5, 6 In daily practice, patients frequently present with bilateral DME. Yet, current treatment algorithm of anti-VEGF compound is fitted to an individual eye regardless of the presence of DME in the fellow eye.
Intraocular injections of anti-VEGF compounds result in their systemic distribution and may affect systemic levels of VEGF.7, 8, 9 Conflicting data were reported with respect to the existence of a contralateral eye effect and the presence of biologically significant levels of anti-VEGF compound in the contralateral eye following unilateral injection.10, 11, 12, 13, 14, 15, 16
In the clinic setting, bilateral injections may mask such a contralateral effect. If such a clinically meaningful effect on the contralateral eye exists, it may influence the treatment algorithm of patients with bilateral DME. It is therefore important to identify and quantify such an effect. To that end, we have evaluated the contralateral eye effect in a group of patients with bilateral DME who received unilateral bevacizumab injection.
Materials and methods
A retrospective analysis was performed on a consecutive group of patients with bilateral DME who received unilateral bevacizumab injection (1.25 mg/0.05 ml) as part of the routine clinic care at the Retina Service, Department of Ophthalmology, Hadassah–Hebrew University Medical Center, Jerusalem, Israel. The study was approved by the institutional ethics committee.
Inclusion criteria included patients with type 1 or type 2 diabetes mellitus aged >18 years. Patients received at least one unilateral intravitreal injection of bevacizumab for DME in the presence of bilateral center-involved DME. DME was defined according to the presence of intraretinal fluid within 1 mm from the center point according to an OCT (Spectralis, Heidelberg, Germany). No thickness threshold was determined for inclusion.
Although fellow eyes of patients included in the study also had center-involved DME per OCT, injections were withheld at patients’ request from one of the eyes. At the time of the study, anti-VEGF therapy for DME was not covered by the national health system in Israel. Accordingly, many patients preferred to withhold therapy from fellow eyes while observing the outcome of the therapy in one eye first.
Exclusion criteria included previous injection of any intravitreal or systemic anti-VEGF compound before the study period, sub-tenon or intraocular steroid injection, presence of any other significant macular pathology such as age-related macular degeneration or vascular occlusive disorder, epiretinal membrane or vitreomacular traction, previous retinal surgery, history of intraocular inflammation or postsurgical macular edema, and laser photocoagulation during the study.
Injections were delivered following a PRN protocol every 4–6 weeks without a mandatory loading dosage. The decision of reinjection was at the clinician’s discretion, based on the presence of persistent intraretinal fluid. Following initiation of therapy for the first eye, some of the patients elected to commence therapy in the second eye as well. In these cases, the period running from the first injection to the visit before contralateral injection was taken into account. Consequently, some eyes received only one injection before fellow eyes were also injected. As controls, we have used a consecutive group of patients from the same clinic, with bilateral DME, who were treated with focal photocoagulation in one eye before the era of anti-VEGF therapy for DME.
Data collected included demographics, systemic co-morbidities, current HBA1C levels, previous laser treatments, ETDRS best-corrected visual acuity (BCVA), ophthalmic findings, and macular central point and central subfield macular thicknesses (CST) according to OCT at first and last visit recorded from both eyes.
The data were analyzed using the SPSS program (version 16; SPSS, Inc., Chicago, IL, USA) and the Instat software (GraphPad, San Diego, CA, USA). T-test, Mann–Whitney test, Wilcoxon matched-pairs signed-ranks test, analysis of variance, and Pearson correlation were utilized when appropriate.
Results
Demographics and clinical characteristics
Thirty-five patients were included in the study. Patients demographics and clinical information are provided in Table 1. The right eye was injected in 18 (51.4%) of the patients. Mean follow-up time was 245±196 days (range: 30–800 days), and the mean number of bevacizumab injections during follow-up was 3.6±2.7 (range: 1–11 injections). Previous focal photocoagulation had been performed in 18 (51.4%) of the injected eyes and 13 (37.1%) of the non-injected eyes. The mean interval between laser photocoagulation treatment and the first intraviteral bevacizumab injection was 5.3±5.3 months (range 2–17 months). The majority of patients had non-proliferative diabetic retinopathy in the injected eye (24 eyes; 68.6%) and non-injected eye (23 eyes; 65.7%). The remainder were classified as having arrested proliferative diabetic retinopathy, which was previously treated with pan retinal photocoagulation, except one non-injected eye in which the severity of retinopathy could not be determined. Pseudophakia was present in 20% of the injected eyes and 14.3% of the non-injected eyes, the rest being phakic.
Visual acuity and macular thickness
There was a trend towards a better initial VA in injected vs non-injected eyes (P=0.07; Mann–Whitney test, Table 2), and initial central subfield thickness (P=0.011; Mann–Whitney test) and central point thickness (P=0.0074; Mann–Whitney test) were higher in injected eyes compared with non-injected eyes (Table 2).
Following bevacizumab injections, there was no significant improvement of the VA in the injected eye (mean logMAR change following injections: −0.067±0.303; P=0.19) and non-injected eye (mean logMAR change following injections: −0.013±0.539; P=0.89, Table 2). Of the 35 patients included in the study, 24 (68.5%) injected eyes and 25 (71.4%) non-injected eyes showed increased or stable VA following bevacizumab therapy (P=1; Fisher’s exact test). Improved VA was detected in 14 (40%) injected eyes and 15 (43%) non-injected eyes (P=1; Fisher’s exact test).
Following bevacizumab treatment, the central macular subfield and central point thicknesses decreased in both the injected and non-injected eyes (Table 2). The average (SD) CST reduction in the injected eye was 72±112 micron while in the non-injected eye it was 49±75 micron (P=0.32 for the comparison of thickness reduction between the eyes; Mann–Whitney test). Sixteen injected eyes (45.7%) showed CST reduction of ≥50 micron (range 68–377 micron), while three injected eyes showed thickness increase of ≥50 micron (range: 50–118 micron). By comparison, 10 (28.6%) non-injected eyes showed thickness reduction >50 micron (range 73–261 micron) while none had increased thickness of >50 micron during the follow-up.
As injected eyes had thicker macula compared with non-injected eyes at baseline, we have also calculated percentage of thickness reduction following treatment. The magnitude of the average reduction in thickness was similar in the injected (10.48±14.9%) and non-injected (12.8±20%) eyes (P=0.29; Mann–Whitney test). Decreased thickness of≥10% following treatment was observed in 16 (45.7%) injected eyes and 13 (37.1%) non-injected eyes (P=0.62, Fisher’s exact test). Twenty-eight (80%) injected eyes and 28 (80%) non-injected eyes showed stable or decreased CST following treatment (P>1; Fisher’s exact test). Examples of response of the non-injected eye to contralateral injection are illustrated in Figures 1 and 2.
Bilateral response to unilateral bevacizumab injection. A 71-year-old male had bilateral diabetic macular edema. Initial central subfield thickness (top row) was 425 μm in the right eye and 682 μm in the left eye. Ten bevacizumab injections were given to the left eye over 18 months while the right eye was observed. Following the first injection (second row) macular thickness reduced to 589 μm (−93 μm) in the left eye and 344 μm (−81 μm) in the right, non-injected eye. At the end of follow-up (third row), macular thickness reduced to 333 μm in the injected eye (−349 μm from baseline; −51.2%) and 268 μm in the non-injected eye (−157 μm from baseline; −37.0%). LogMar BCVA improved from 0.4 to 0.3 (Snellen equivalent from 20/50 to 20/40) in the injected eye and from 0.22 to 0 (Snellen equivalent from 20/33 to 20/20) in the non-injected eye.
Response to repeated contralateral bevacizumab injections in a 62-year-old male with bilateral diabetic macular edema. Initial central subfield thickness (top row) was 446 μm in the right eye and 327 μm in the left eye. LogMar BCVA was 0.32 (Snellen equivalent 20/42) in both eyes. Five bevacizumab injections were given to his left eye during 10 months while the right remained untreated. Iterative injections were requested before a clinical effect was observed (no substantial response recorded in either eye after the first injection, second row). At the end of follow-up (third row), macular thickness reduced to 318 μm (−9 μm, −2.8%) in the left injected eye and to 335 μm (−111 μm, −24.9%) in the right non-injected eye. LogMar BCVA remained 0.32 (Snellen equivalent 20/42) in the injected eye but improved to 0.22 (Snellen equivalent 20/33) in the non-injected eye.
To exclude potential sources of bias, the analysis was also performed after exclusion of patients with CST of <300 micron in either injected or fellow eye (n=9) and patients who underwent intraocular surgery during the study period (n=4). In addition, follow-up was limited for 1 year to exclude large variation in follow-up time among the patients. The remaining 22 patients had mean initial and final macular thickness in the injected eye of 504±139 and 407±117 micron (P=0.0002; Wilcoxon matched-pairs signed-ranks test), respectively. In the non-injected eye, initial mean macular thickness was 423±119 while the final thickness was 369±114 (P=0.0005; Wilcoxon matched-pairs signed-ranks test).
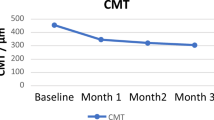
To exclude an effect of a short follow-up time, we have also analyzed a sub-group of 20 patients who were treated with at least three bevacizumab injections. These patients were analyzed at 3 months following initiation of therapy. The CST decreased in these eyes from 477±155 to 432±123 micron in the bevacizumab-injected eyes (P=0.25; Wilcoxon matched-pairs signed-ranks test). At the same time, in the non-injected eyes the thickness reduced from 394±109 to 344±87 micron (P=0.01; Wilcoxon matched-pairs signed-ranks test).
The historical control group included 32 patients with bilateral DME who were treated with focal photocoagulation in one eye during 2009. Fourteen patients were excluded owing to missing data. Demographics and clinical characteristics of the remaining 18 patients as compared with the bevacizumab-treated patients are presented in Table 1. The mean (SD) initial CST in the laser-treated and non-treated eye was 348±107 (range 197–578) and 328±105 micron (range 178–573 micron; P=0.3), respectively. The follow-up period for these eyes before the treatment of the fellow eye with laser photocoagulation ranged from 3 to 5 months. CST (SD) at the end of follow-up in the treated and the control eye was 376±126 micron (range 249–650 micron; P=0.12 vs initial thickness), and 334± 129 micron (range 202–677 micron; P=0.87 vs initial thickness), respectively.
Factors associated with visual acuity and macular thickness response to treatment
There was a correlation between the VA changes in the injected and non-injected eyes following bevacizumab treatment (Pearson’s correlation coefficient=0.467, P=0.005). There was also a trend towards correlation between the injected and non-injected eyes in terms of central subfield thickness change following treatment (Pearson’s correlation coefficient=0.286, P=0.096).
Patient’s age correlated with VA changes following treatment in the injected eyes (Pearson’s correlation coefficient=0.469, P=0.004), and a trend towards such a correlation was present in the non-injected eye (Pearson’s correlation coefficient=0.307, P=0.073). There was no correlation between the VA or macular thickness changes following bevacizumab injections and other factors evaluated. Among these factors were gender, diabetes duration and type, HBA1C levels, severity of diabetic retinopathy, number of bevacizumab injections, systemic co-morbidities, duration of follow-up, lens status, and previous laser photocoagulation.
Discussion
This study shows a considerable effect of unilateral bevacizumab injections in the non-injected eye of patients with bilateral DME. More than a quarter of the patients experienced a reduction >50 micron of central macular thickness in the non-injected eye and more than a third showed a >10% reduction in central subfield thickness. In fact, there was no significant difference between thickness reduction in the injected and non-injected fellow eye in this series of patients. Conceivably, such an effect is facilitated by escape of bevacizumab to the systemic circulation that may be facilitated by the breakdown of the blood–retina barrier in eyes with DME. There was no such contralateral eye effect following unilateral application of laser photocoagulation in eyes with bilateral DME. This fact as well as the known natural course of DME supports the conclusion that fellow eye effect which we have observed is related to anti-VEGF therapy.
In rabbits, low concentrations of bevacizumab, of unknown functional significance, were measured in the fellow non-injected eye following intravitreal injection.17, 18, 19 In humans, it has been well established that anti-VEGF drugs delivered within the vitreous can pass into the systemic circulation. Serum level of VEGF was demonstrated to be reduced after intravitreal bevacizumab injections in infants with retinopathy of prematurity,8 in patients with neovascular age-related macular degeneration9 and in patients with type 2 diabetes.7 In patients with age-related macular degeneration, contralateral intravitreal bevacizumab injection influenced retrobulbar hemodynamic parameters.20
Systemic presence of anti-VEGF compounds following intraocular injection are a matter of concern with respect to potential systemic side effects. On the other hand, such systemic distribution can underlie unexpected treatment effects that have been anecdotally reported in non-injected fellow eyes of patients receiving intravitreal anti-VEGF therapy for a variety of retinal pathologies.10, 11, 12, 14, 16
Other studies provided conflicting data on the effect of anti-VEGF treatment on fellow eyes. Meyer et al13 reported undetectable levels of unbound bevacizumab in the aqueous of non-injected eye following intravitreal injection of bevacizumab. The authors concede that VEGF-bounded bavacizumab may exert an effect on DME without being detected in the aqueous by their method. It is also possible that systemic alterations in VEGF level may affect DME.
Velez-Mentoya et al15 failed to identify a contralateral eye effect in a prospective study of 23 patients with bilateral DME who received unilateral intravitreal bevacizumab followed by 4 weeks of follow-up. Similarly, Gamulescu and Helbig21 failed to identify contralateral eye effect in a short-term prospective study of 26 patients with bilateral neovascular age-related macular degeneration (NVAMD) who were treated with ranibizumab. On the other hand, Bakbak et al22 recently reported of significant contralateral eye effect for bevacizumab in 55 patients with bilateral DME, whereas such an effect was not noted in 32 eyes treated with ranibizumab for the same indication.
Several factors may underlie our apparently contradicting findings compared with studies by Velez-Montoya and Gamulescu.15, 21 First, it is plausible that in DME anti-VEGF compounds may be more likely to escape to the systemic circulation compared with NVAMD due to the widespread failure of the blood–retina barrier in diabetic retinopathy.
Second, it has been suggested that the long-term effect of anti-VEGF compounds on blood–retina barrier could account for the fact that multiple injections are frequently required before maximal clinical response can be seen in DME.23 Thus the short-term design of the studies by Velez-Montoya and Gamulescu might not be sufficient to capture contralateral eye effect, whereas our longer follow-up (average 245 days) and larger number of injections (3.6) facilitate its detection.
Finally, a DRCR network study, which compared ranibizumab, steroid, and laser photocoagulation therapy for DME, also failed to detect an excess contralateral eye effect in a subgroup of study patients where one eye was treated with ranibizumab and the second with photocoagulation.1 Yet, this study was not designed to assess for a contralateral eye effect, and the effect of the photocoagulation may mask a contralateral eye effect of ranibizumab if these effects are not additive and of similar magnitude. In addition, intravitreal delivery of bevacizumab was recently demonstrated to result in larger reduction in systemic VEGF levels compared with intravitreal ranibizumab injection.9 This finding corroborates the report by Bakbak et al22 on the contralateral eye effect in DME of bevacizumab but not of ranibizumab injections. Thus, the contralateral effect of ranibizumab and bevacizumab may not necessarily be similar. This discrepancy may be underlined by the presence of Fc portion in the bevacizumab but not in the ranibizumab molecule and an active transport of the compound into the systemic circulation that is facilitated by this portion.
Existence of clinical meaningful contralateral eye effect in more than a quarter of patients implies that a treatment strategy may be potentially tailored to the patient with bilateral DME rather than addressing one’s individual eye. Hypothetically, in such cases it may be appropriate to initiate anti-VEGF treatment in one eye only while observing the fellow eye for an effect. There are several advantages in treating one eye instead of both, among them reduced discomfort associated with intravitreal injection, reduced risk for ocular complication, and reduced cost. Potential dose-dependent drug-related systemic adverse events may also be reduced. However, we did not detect visual improvement in fellow eye following unilateral injections. Thus, further research is required to characterize such contralateral eye effect and to evaluate the efficacy and safety of such potential treatment algorithm.

References
Elman MJ, Aiello LP, Beck RW, Bressler NM, Bressler SB, Edwards AR et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology 2010; 117: 1064–1077.
Elman MJ, Bressler NM, Qin H, Beck RW, Ferris FL 3rd, Friedman SM et al. Expanded 2-year follow-up of ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology 2011; 118: 609–614.
Mitchell P, Bandello F, Schmidt-Erfurth U, Lang GE, Massin P, Schlingemann RO et al. The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology 2011; 118: 615–625.
Nguyen QD, Brown DM, Marcus DM, Boyer DS, Patel S, Feiner L et al. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology 2012; 119: 789–801.
Aiello LP, Beck RW, Bressler NM, Browning DJ, Chalam KV, Davis M et al. Rationale for the diabetic retinopathy clinical research network treatment protocol for center-involved diabetic macular edema. Ophthalmology 2011; 118: e5–14.
Wang H, Sun X, Liu K, Xu X . Intravitreal ranibizumab (Lucentis) for the treatment of diabetic macular edema: a systematic review and meta-analysis of randomized clinical control trials. Curr Eye Res 2012; 37: 661–670.
Matsuyama K, Ogata N, Matsuoka M, Wada M, Takahashi K, Nishimura T . Plasma levels of vascular endothelial growth factor and pigment epithelium-derived factor before and after intravitreal injection of bevacizumab. Br J Ophthalmol 2010; 94: 1215–1218.
Sato T, Wada K, Arahori H, Kuno N, Imoto K, Iwahashi-Shima C et al. Serum concentrations of bevacizumab (avastin) and vascular endothelial growth factor in infants with retinopathy of prematurity. Am J Ophthalmol 2012; 153: 327–333.
Chakravarthy U, Harding SP, Rogers CA, Downes SM, Lotery AJ, Wordsworth S et al. Ranibizumab versus bevacizumab to treat neovascular age-related macular degeneration: one-year findings from the IVAN randomized trial. Ophthalmology 2012; 119: 1399–1411.
Acharya NR, Sittivarakul W, Qian Y, Hong KC, Lee SM . Bilateral effect of unilateral ranibizumab in patients with uveitis-related macular edema. Retina 2011; 31: 1871–1876.
Al-Dhibi H, Khan AO . Bilateral response following unilateral intravitreal bevacizumab injection in a child with uveitic cystoid macular edema. J AAPOS 2009; 13: 400–402.
Avery RL, Pearlman J, Pieramici DJ, Rabena MD, Castellarin AA, Nasir MA et al. Intravitreal bevacizumab (Avastin) in the treatment of proliferative diabetic retinopathy. Ophthalmology 2006; 113: 1691–1695.
Meyer CH, Krohne TU, Holz FG . Concentrations of unbound bevacizumab in the aqueous of untreated fellow eyes after a single intravitreal injection in humans. Acta Ophthalmol 2012; 90: 68–70.
Scartozzi R, Chao JR, Walsh AC, Eliott D . Bilateral improvement of persistent diffuse diabetic macular oedema after unilateral intravitreal bevacizumab (Avastin) injection. Eye 2009; 23: 1229.
Velez-Montoya R, Fromow-Guerra J, Burgos O, Landers MB 3rd, Morales-Catón V, Quiroz-Mercado H . The effect of unilateral intravitreal bevacizumab (avastin), in the treatment of diffuse bilateral diabetic macular edema: a pilot study. Retina 2009; 29: 20–26.
Wu Z, Sadda SR . Effects on the contralateral eye after intravitreal bevacizumab and ranibizumab injections: a case report. Ann Acad Med Singapore 2008; 37: 591–593.
Bakri SJ, Snyder MR, Reid JM, Pulido JS, Ezzat MK, Singh RJ . Pharmacokinetics of intravitreal ranibizumab (Lucentis). Ophthalmology 2007; 114: 2179–2182.
Nomoto H, Shiraga F, Kuno N, Kimura E, Fujii S, Shinomiya K et al. Pharmacokinetics of bevacizumab after topical, subconjunctival, and intravitreal administration in rabbits. Invest Ophthalmol Vis Sci 2009; 50: 4807–4813.
Sinapis CI, Routsias JG, Sinapis AI, Sinapis DI, Agrogiannis GD, Pantopoulou A et al. Pharmacokinetics of intravitreal bevacizumab (Avastin(R)) in rabbits. Clin Ophthalmol 2011; 5: 697–704.
Hosseini H, Lotfi M, Esfahani MH, Nassiri N, Khalili MR, Razeghinejad MR et al. Effect of intravitreal bevacizumab on retrobulbar blood flow in injected and uninjected fellow eyes of patients with neovascular age-related macular degeneration. Retina 2012; 32: 967–971.
Gamulescu MA, Helbig H . Lack of therapeutic effect of ranibizumab in fellow eyes after intravitreal administration. J Ocul Pharmacol Ther 2010; 26: 213–216.
Bakbak B, Ozturk BT, Gonul S, Yilmaz M, Gedik S . Comparison of the effect of unilateral intravitreal bevacizumab and ranibizumab injection on diabetic macular edema of the fellow eye. J Ocul Pharmacol Ther 2013; 29: 728–732.
Kook D, Wolf A, Kreutzer T, Neubauer A, Strauss R, Ulbig M et al. Long-term effect of intravitreal bevacizumab (avastin) in patients with chronic diffuse diabetic macular edema. Retina 2008; 28: 1053–1060.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Hanhart, J., Tiosano, L., Averbukh, E. et al. Fellow eye effect of unilateral intravitreal bevacizumab injection in eyes with diabetic macular edema. Eye 28, 646–653 (2014). https://doi.org/10.1038/eye.2014.94
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.94