Abstract
Purpose
To assess the incidence and clinical features of unexpected visual loss after removal of silicone oil (ROSO).
Patients and methods
A retrospective cross-sectional observational study of 421 consecutive eyes, which underwent silicone oil removal at one institution over a 2-year period.
Results
Fourteen (3.3%) patients, (12 male, mean age of 53.1 years) suffered unexplained visual loss. In these eyes, the mean duration of silicone oil fill was 141 days (range 76–218). The mean loss of visual acuity was 3.7 (range 2–6) Snellen lines (SL) at 1 month, 3.5 (2–6) SL at 3 months and 2.91 (0–6) SL at 6 months. The change from preoperative visual acuity was statistically significant at all visits (P=0.02). Subgroup analysis of 20 fovea-sparing giant retinal tear (GRT) detachments, observed 10 (50%) cases of visual loss after ROSO. Electrodiagnostic testing suggested predominantly macular dysfunction, with optic nerve involvement in one case. Five of the 14 cases had variable recovery of vision.
Conclusion
There is a 3.3% overall incidence of visual loss following ROSO with a high rate (50%) observed in maculae on GRT detachments. Although recovery of visual acuity is seen in a minority of cases, visual loss after ROSO remains a serious and unexplained concern for vitreoretinal surgeons.
Similar content being viewed by others
Introduction
Silicone oil is widely used as a long-lasting retinal tamponade agent in vitreoretinal surgery. It is frequently used in retinal detachment cases complicated by proliferative vitreoretinopathy (PVR), giant retinal tears (GRT), viral retinitis, ocular trauma, and proliferative diabetic retinopathy.1, 2, 3
Removal of silicone oil (ROSO) is usually indicated for visual (often refractive) improvement and to reduce the risk of progressive oil-associated complications such as cataract, glaucoma and keratopathy.4, 5 In addition, pathological evidence suggests that silicone oil droplets can become impregnated within the neuroretina, pigment epithelium, optic nerve and trabecular meshwork6, 7 and this can potentially be prevented by oil removal. It has been documented that after ROSO, complications resulting in loss of vision occur in up to 32% of patients.8, 9, 10, 11 This is most commonly due to re-detachment (6–25%), CMO (12%), hypotony (16%) and epiretinal membranes (12%). In addition, there have been concerns that retinal toxicity may result from silicone oil use.11
Unexplained vision loss immediately after ROSO was first described in 2004.12 Subsequently, further similar series have documented this phenomenon.13, 14, 15, 16, 17, 18, 19 The etiology and prevalence of this complication is still unclear and this makes counseling patients challenging. The purpose of this study was, therefore, to determine the incidence of unexplained loss of visual acuity after ROSO in a large unselected, consecutive cohort of patients and to identify risk factors through analysis of clinical features of cases with this complication.
Materials and methods
Institutional Review Board/Ethics Committee approval was obtained. A retrospective analysis was carried out on all consecutive patients who underwent ROSO at the vitreoretinal unit at Moorfields Eye Hospital from January 2005 to December 2006. Subgroup analysis was performed on GRT cases, as these were frequently fovea-sparing and had good preoperative visual acuities. The primary outcome was defined as sudden and unexplained loss of two or more lines of Snellen visual acuity after ROSO from the best corrected visual acuity (BCVA) at any point with silicone oil in situ. Cases with recurrent retinal detachment were excluded.
Electronic patient database information collected included age, gender, affected eye, macular status at the time of presentation, presence of GRT, type and date of initial surgery, silicone oil viscosity and type, total number of operations, BCVA at presentation, pre and post ROSO, and at months 1, 2, 3, 6, 9, and 12 after removal of oil. In addition, the presence of PVR, lens status, duration of silicone oil fill, type of surgery for ROSO, pre, intra and post surgical complications were noted. Snellen visual acuity was recorded and converted to logMar acuity for statistical analysis purposes. Where performed, the results of ancillary tests such as fluorescein angiography, OCT and electrodiagnostics were also recorded. Statistical analysis for independent samples was performed using Friedman’s test to compare non-parametric repeated measures on SPSS v.16 (IBM, New York, NY, USA).
Results
A total of 421 patients underwent ROSO between January 2005 and December 2006 and were included in the study. Fourteen patients (3.3%) (12 men and 2 women, mean age 53.1 years) were found to have a loss of visual acuity of two or more Snellen lines (SL) in the immediate postoperative period (first postoperative review on day 1) following ROSO (Table 1).
In all of these cases, 1300 centistoke (cs) silicone oil had been used. In six cases (patients 2, 3, 5, 9, 10, and 14, Oxane 1300 (Bausch and Lomb, USA) was used and in eight cases Arciolane 1300 (Arcadophtha, France) was used. In all cases, the retina remained attached under silicone oil fill and for at least 12 months after its removal.
In nine of the 14 cases with visual loss, ROSO had been performed in combination with phacoemulsification. Oil was removed using a 19-gauge syringe through a posterior capsule rhexis prior to intraocular lens implantation. In five cases the technique was 19-gauge syringe aspiration through a pars plana sclerotomy with either pars plana infusion (four cases) or anterior chamber infusion (one case). Identical oil removal techniques were used in cases where no visual loss was recorded.
Three hundred and sixty degrees anterior retinal laser barrier was performed in 13 cases (92.8%) to reduce the risk of retinal re-detachment on oil removal. In five cases this was performed at the time of original surgery and in eight cases prior to silicone oil removal. The mean duration of silicone oil fill in affected eyes was 141 days (76–218).
In cases with visual loss, the mean drop of visual acuity from silicone oil-filled eyes was 3.7 SL (range 2–6) at 1 month, 3.5 lines (range 2–6) at month 3 and 2.91 lines (range 0–6) at month 6. Mean logMar visual acuity prior to initial surgery was 0.48 logMar (range –0.08–1.48) and after vitrectomy and silicone oil insertion was 0.3 logMar (range −0.08–0.6). Visual acuities subsequently dropped after removal of oil to a mean of 1.35 logMar (range 0.6–2.00) at 1 month, 1.03 logMar (range 0.6–1.77) at month 3, 0.99 logMar (range 0.47–1.77) at month 6 and 0.98 logMar (range 0.47–1.77) at month 12.
Of the 14 patients who lost at least two SL of vision after 1 month post silicone oil removal, 2 patients (numbers 4 and 11) recovered visual acuity to the same level as with oil in situ after 6 months. A further three patients (5, 7, and 14) experienced a gradual recovery in visual acuity although this remained markedly reduced compared with preoperative or silicone oil fill visual acuities. Patient 5 improved from 3/60 1 month after removal of oil to 6/36 at month 6; patient 7 improved from 3/60 at month 6 to 6/36 at month 12, and patient number 14 improved from count fingers vision at month one to 6/18 at month 6 after oil removal. The recovery of visual acuity did not relate to changes in refraction, media opacities or macular edema. In nine other patients the reduced visual acuity remained stable over the follow-up period (in patient 12 follow-up was limited to 3 months post removal of oil). At the time of oil removal, three patients were pseudophakic and 11 patients were phakic. Phacoemulsification with IOL implant was performed at the same time of ROSO in 9 of the 11 phakic cases. The two remaining phakic cases had no significant media opacity at the time of final follow-up, and cataract was not deemed a confounding factor contributory to visual loss.
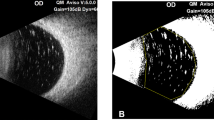
Electrodiagnostics test were performed in six patients, (1, 8, 9, 10, 11, and 13), all of which included pattern electroretinogram (ERG) and full-field ERG according to the International Society for Clinical Electrophysiology of Vision standards (scotopic rod ERG, bright flash ERG, photopic 20 Hz, flicker ERG and transient photopic ERG). Mild-to-moderate generalized retinal dysfunction affecting rod and cone photoreceptors with macular involvement was present in patients 1, 8, 10, 11, and 13. Subnormal pattern ERG suggestive of isolated macular dysfunction was identified in patient 9. Optic nerve involvement ranging in abnormality from mild-to-moderate dysfunction was detected in pattern visual evoked potential (VEP) in patients 8 and 13.
Optical coherence tomography (OCT) was performed in eight patients and excluded cystoid macular edema (CMO) in all cases. Patients 7, 8, and 10 were noted to have a mild epiretinal membrane, which was not considered to be significantly contributory to loss of vision.
Patient 13 had raised intraocular pressure post ROSO, which was managed successfully with topical medication. Patient 1 underwent a further procedure to remove residual oil bubbles 7 weeks after the initial removal of oil. After the second procedure visual acuity remained unchanged.
The mean change in visual acuity from pre-ROSO levels was statistically significant at all visits (P=0.02). BCVA at months 1, 3, 6, and 12 did not show any statistically significant correlation with presence of IOL, intraoperative laser, PVR, duration of silicone oil fill, or type of silicone oil used.
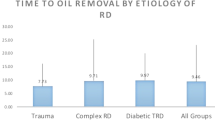
GRT cases
Of the total study population of 421 cases we identified 54 retinal detachments secondary to GRTs 26 (48.1%) of which were fovea-sparing at the time of initial surgery. Silicone oil tamponade is a standard treatment for GRT cases at Moorfields Eye Hospital. Six patients were excluded from analysis—in four silicone oil was not removed owing to high risk of re-detachment and two patients were lost to follow-up. Hence, 20 patients who underwent silicone oil removal were analyzed.
Analysis of these macula on rhegmatogenous retinal detachments (RRDs) secondary to GRT identified 10 cases of visual loss (≥2 SL) after ROSO, giving a rate of visual loss of 50% in this subgroup. (see Table 1). No other ocular pathology was found to explain the reduction in vision. Of the other 10 patients, 7 had improved visual acuity after removal of oil and in three, visual acuity remained unchanged.
Discussion
Visual loss after ROSO oil is an important and serious complication. In this study we analyzed 421 consecutive removal of oil operations over 2 years at one tertiary referral institution and found 14 cases of unexplained visual loss. This suggests an overall incidence of 3.3%.
The etiology of visual loss following removal of oil remains uncertain. Several hypotheses have been proposed including sudden changes in potassium concentration in retro-oil fluid that may lead to macular dysfunction due to photoreceptor apoptosis on oil removal,18, 20 photo-toxicity at the time of silicone oil removal,15, 21, 22 and fibrogenic growth factor disturbances.23
Of the 14 patients who had at least two SL reduction in visual acuity in our study this appeared to happen at the time of oil removal. None of our patients was noted to have central scotomas prior to oil removal. This finding contrasts to that of Herbert et al24 where central visual loss developed with oil in situ in a retrospective study of five patients. In all of our cases good vision was documented following initial vitrectomy and silicone oil exchange and vision fell immediately after oil removal. The timing of visual loss is similar to most previous reports12, 16, 17 although it is notable that Cazabon et al20 reported visual loss 1 week following oil removal. Whether visual loss with silicone oil in situ is an entirely different phenomenon from visual loss after oil removal is yet to be established.
Six patients underwent electrophysiology of these five had reduction in PERG P50 component and full-field ERG reduction consistent with macular dysfunction and generalized retinal involvement of both rod and cone systems at the photoreceptor level. One patient had markedly subnormal PERG with no definite evidence of more generalized retinal involvement suggestive of isolated macular involvement. In two cases we identified pattern VEP delay compatible with primary optic nerve dysfunction. In previous series, electrodiagnostic results are variable and showed three different presentations; generalized retinal dysfunction with macular involvement, circumscribed macular involvement, and optic nerve dysfunction (Table 2).
As generalized, retinal dysfunction is expected in cases of retinal detachment, most cases we have analyzed appear to have visual loss due to additional macular dysfunction. Of the 17 cases with electrophysiology published in the literature,12, 13, 20, 24 15 had macular involvement, whereas two cases had optic nerve dysfunction. This is in line with our findings where the most common electrodiagnostic finding is macular involvement with generalized retinal dysfunction, and optic nerve dysfunction accounting for only a small number of cases (Table 2).
In our series there was a higher prevalence in men (85.7%) as previously reported,12 although this may be biased by the higher proportion of males who suffer GRTs generally.25 Unlike Newsom et al, we did not find a higher prevalence in younger patients—in our patients the mean age was 53.1 years (range 40–74). We did not find an association between loss of vision and duration of silicone oil fill, silicone oil type, nor lens status. When visual loss occurs it is usually severe. In the group of affected patients average visual acuity was 0.3 Log Mar with oil fill and 1.0 Log Mar at month 3 following removal of oil (average 3.5 SL) and this visual reduction usually persisted. Mean visual acuity 12 months after removal of oil was 0.98 Log Mar. Two of the 14 patients did, however, recover vision to the level with oil in situ and three patients experienced a modest and gradual improvement in their visual acuities. The recovery in visual acuity we have noted in these cases has in general not been reported in previous series.
The 20 patients with GRT and macular on retinal detachment managed with silicone oil tamponade represent a subgroup in which excellent visual recovery would be expected following removal of oil with or without cataract extraction. We documented an alarming rate of severe unexplained visual loss of 50% in this subgroup. All cases were fovea-sparing at presentation and at surgery, and no PVR was documented in any case. All had laser barrier prior to silicone oil removal and none re-detached. Our findings concur with those of Chirstensen and La Cour.19 They report a series of nine patients who had had macula on RRD where SO was used as a tamponade. Three (33%) of this series had a resultant postoperative BCVA ≤6/60. They suggest inner retinal thinning as a mechanism behind this. This theory remains to be replicated.
It remains uncertain as to whether our findings represent a genuinely higher incidence in GRT cases or whether other cases where silicone oil is used may have a similar incidence, which may be masked by co-existing pathology such as macular detachment or PVR. Vitreoretinal surgeons frequently note that some patients, following removal of oil and cataract extraction, do not improve their visual acuity or experience a very modest improvement and these may represent de facto visual loss cases. Therefore, the true incidence of visual loss following silicone oil removal may be significantly underestimated.
The incidence of this problem has implications for our clinical practice and also raises questions on what measures can be taken to possibly prevent this severe complication. Reducing the number of cases where silicone oil is used and the amount of exposure to light during the surgical ROSO should be considered. It is also important to advise patients about the potential for this as yet, untreatable complication.
Our study is retrospective and therefore did not have a standardised investigation protocol for affected cases. We therefore lack electrophysiology and OCT data on some patients. Furthermore fundus autofluorescence may have provided a further insight. Nevertheless, we have detailed visual acuity assessments on all patients and our primary aim was to define the incidence rate of this condition. Although follow-up varied because of the retrospective nature of the analysis, only one patient did not have follow-up beyond 3 months. Our criterion for visual loss was a reduction of two or more SL. This was considered to be clinically relevant and sufficiently inclusive. Our study was undertaken at a single center enabling accurate and comprehensive data collection, but may not account for geographical variation. Nationwide surveillance may be required to definitively determine the national incidence.
This is the largest published cohort of consecutive patients undergoing ROSO from the vitreous cavity. The overall incidence of visual loss on oil removal was 3.3% with a higher documented rate in GRT-related macula on retinal detachments. This is the first report of modest visual recovery occurring in some patients over time. Our incidence rate of unexplained visual loss is significant, particularly in those with apparent good visual potential, and represents an unexplained concern for vitreoretinal surgeons.

References
Lim JI, Enger C, Haller JA, Campochiaro PA, Meredith TA, de Bustros S et al. Improved visual results after surgical repair of cytomegalovirus-related retinal detachments. Ophthalmology 1994; 101 (2): 264–269.
Azen SP, Scott IU, Flynn HW Jr, Lai MY, Topping TM, Benati L et al. Silicone oil in the repair of complex retinal detachments. A prospective observational multicenter study. Ophthalmology 1998; 105 (9): 1587–1597.
Camacho H, Bajaire B, Mejia LF . Silicone oil in the management of giant retinal tears. Ann ophthalmol 1992; 24 (2): 45–49.
Chan C, Okun E . The question of ocular tolerance to intravitreal liquid silicone. A long-term analysis. Ophthalmology 1986; 93 (5): 651–660.
Federman JL, Schubert HD . Complications associated with the use of silicone oil in 150 eyes after retina-vitreous surgery. Ophthalmology 1988; 95 (7): 870–876.
Shields CL, Eagle RC Jr . Pseudo-Schnabel's cavernous degeneration of the optic nerve secondary to intraocular silicone oil. Arch Ophthalmol 1989; 107 (5): 714–717.
Honda Y, Ueno S, Miura M, Yamaguchi H . Silicone oil particles trapped in the subretinal space: complications after substitution of the vitreous. Ophthalmologica 1986; 192 (1): 1–5.
Franks WA, Leaver PK . Removal of silicone oil—rewards and penalties. Eye 1991; 5 (Pt 3): 333–337.
Larkin GB, Flaxel CJ, Leaver PK . Phacoemulsification and silicone oil removal through a single corneal incision. Ophthalmology 1998; 105 (11): 2023–2027.
Hutton WL, Azen SP, Blumenkranz MS, Lai MY, McCuen BW, Han DP et al. The effects of silicone oil removal. Silicone Study Report 6. Arch Ophthalmol 1994; 112 (6): 778–785.
Jiang F, Krause M, Ruprecht KW, Hille K . Risk factors for anatomical success and visual outcome in patients undergoing silicone oil removal. Eur J Ophthalmol 2002; 12 (4): 293–298.
Newsom RS, Johnston R, Sullivan PM, Aylward GB, Holder GE, Gregor ZJ . Sudden visual loss after removal of silicone oil. Retina 2004; 24 (6): 871–877.
Michel G, Meyer L, Naoun O . [Sudden visual loss following silicone oil removal: three patients treated for giant retinal tear]. J Fr Ophtalmol 2009; 32 (2): 104–111.
Williams PD, Fuller CG, Scott IU, Fuller DG, Flynn HW . Vision loss associated with the use and removal of intraocular silicone oil. Clin Ophthalmol 2008; 2 (4): 955–959.
Herbert EN, Laidlaw DA, Williamson TH, Habib M, Steel D . Loss of vision once silicone oil has been removed. Retina 2005; 25 (6): 808–809.
Satchi K, Bolton A, Patel CK . Loss of vision once silicone oil has been removed. Retina 2005; 25 (6): 807–808.
Tavallali A, Soheilian M . Loss of vision once silicone oil has been removed. Retina 2005; 25 (6): 806; author reply 806–807.
Winter M, Eberhardt W, Scholz C, Reichenbach A . Failure of potassium siphoning by Muller cells: a new hypothesis of perfluorocarbon liquid-induced retinopathy. Invest Ophthalmol Vis Sci 2000; 41 (1): 256–261.
Christensen UC, la Cour M . Visual loss after use of intraocular silicone oil associated with thinning of inner retinal layers. Acta Ophthalmol 2012; 90 (8): 733–737.
Cazabon S, Groenewald C, Pearce IA, Wong D . Visual loss following removal of intraocular silicone oil. Br J Ophthalmol 2005; 89 (7): 799–802.
Azzolini C, Docchio F, Brancato R, Trabucchi G . Interactions between light and vitreous fluid substitutes. Arch Ophthalmol 1992; 110 (10): 1468–1471.
Dogramaci M, Williams K, Lee E, Williamson TH . Foveal light exposure is increased at the time of removal of silicone oil with the potential for phototoxicity. Graefes Arch Clin Exp Ophthalmol 2013; 251 (1): 35–39.
Asaria RH, Kon CH, Bunce C, Sethi CS, Limb GA, Khaw PT et al. Silicone oil concentrates fibrogenic growth factors in the retro-oil fluid. Br J Ophthalmol 2004; 88 (11): 1439–1442.
Herbert EN, Habib M, Steel D, Williamson TH . Central scotoma associated with intraocular silicone oil tamponade develops before oil removal. Graefes Arch Clin Exp Ophthalmol 2006; 244 (2): 248–252.
Ang GS, Townend J, Lois N . Epidemiology of giant retinal tears in the United Kingdom: the British Giant Retinal Tear Epidemiology Eye Study (BGEES). Invest Ophthalmol Vis Sci 2010; 51 (9): 4781–4787.
Acknowledgements
This research received no specific grant from any funding agency.
Author contributions
RM and AC were involved in the data acquisition and analysis, drafted and approved final manuscript. PB drafted and approved the final manuscript. DT and NA were involved in the data acquisition and approved the final manuscript. DC supervised the study and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Part of this work was previously presented at Club Jules Gonin Meeting in 2011.
Rights and permissions
About this article
Cite this article
Moya, R., Chandra, A., Banerjee, P. et al. The incidence of unexplained visual loss following removal of silicone oil. Eye 29, 1477–1482 (2015). https://doi.org/10.1038/eye.2015.135
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2015.135
This article is cited by
-
Functional and perfusion changes associated with silicone oil tamponade after macula-off rhegmatogenous retinal detachment surgery: an optical coherence tomography angiography/microperimetry study
International Ophthalmology (2024)
-
Unexplained visual loss in retinal detachment repair: comparing gas, silicone oil and heavy silicone oil by multivariable regression.
International Journal of Retina and Vitreous (2023)
-
Unexplained visual loss after primary pars-plana-vitrectomy with silicone oil tamponade in fovea-sparing retinal detachment
BMC Ophthalmology (2023)
-
Altitude and gas expansion in repaired rhegmatogenous retinal detachment
Eye (2023)
-
Visusminderung und Silikonöltamponade
Die Ophthalmologie (2022)