Abstract
Purpose
The purpose of this study is to investigate the factors associated with reactivation of the lesion during the first year in patients with polypoidal choroidal vasculopathy (PCV) treated with intravitreal ranibizumab.
Patients and methods
This retrospective observational study included 84 eyes diagnosed with PCV and treated with 3-monthly ranibizumab injections. Only those patients who exhibited complete resolution of fluid after initial treatment and were followed up at least 12 months were included. The baseline characteristics of the patients, including their age and sex, location of the polyps, greatest linear dimensions of the lesions, largest polyp diameter, choroidal vascular hyperpermeability, submacular hemorrhages ≥1 disc area in size, presence of grape-like polyp clusters, central foveal thickness, and best-corrected visual acuity were compared between patients with and without reactivation of the lesion.
Results
During the 12-month follow-up period, reactivation of the lesion was observed in 60 patients (71.4%). The first reactivation was noted at a mean duration of 3.9±1.7 months after the third ranibizumab injection. Cox regression analysis revealed that the absence of submacular hemorrhages ≥1 disc area (P=0.009), presence of grape-like polyp clusters (P=0.002), and greatest linear dimension of the lesions (P=0.019) were associated with reactivation of the lesion.
Conclusion
The absence of submacular hemorrhages, presence of grape-like polyp clusters, and large lesion size at diagnosis were associated with a high risk of reactivation of PCV in patients treated with intravitreal ranibizumab. Patients exhibiting these characteristics may require close monitoring.
Similar content being viewed by others
Introduction
Polypoidal choroidal vasculopathy (PCV) is a peculiar type of choroidal neovascularization (CNV) characterized by the presence of polypoidal vascular lesions and a branching vascular network.1, 2 Although it has been debated whether PCV is a subtype of neovascular, age-related macular degeneration (AMD),3 anti-vascular endothelial growth factor (VEGF) therapy, which had been developed to treat neovascular AMD,4, 5 has also been used as one of the effective treatment methods for PCV.6, 7, 8
The as-needed regimens9 and treat-and-extend regimens10 are widely used strategies for the treatment of the neovascular AMD. In an as-needed regimen, once a dry macula is noted after the initial injections, the additional treatment is performed only in the cases of reactivation.9 In a treat-and-extend regimen, additional injections are administered at each of the follow-up visits, whose intervals are regulated based on the results of the optical coherence tomography (OCT) and clinical examinations.10
It is important, for several reasons, to investigate the factors associated with PCV reactivation. When using an as-needed regimen, patients with high-risk characteristics require frequent follow-up. Furthermore, establishing risk factors for reactivation may help to determine which patients require proactive rather than as-needed regimens. That is, patients at high-risk of reactivation may be good candidates for proactive treatment, such as the treat-and-extend regimens. In previous studies, largest polyp diameter,11 old age,12 and male sex12 were found to be associated with a high-risk of reactivation. However, grape-like polyp clusters13 and submacular hemorrhage have not yet been considered as potential predictive factors of reactivation, even though they are not rare findings.
The purpose of the present study was to investigate the factors associated with reactivation of the lesion in patients with PCV treated with intravitreal ranibizumab. In particular, the abilities of grape-like polyp clusters and submacular hemorrhages to predict reactivation were analyzed.
Materials and methods
This retrospective, observational, case series study was performed at a single study center. The study was approved by the Institutional Review Board of the Kim’s Eye Hospital and was conducted in accordance with the tenets of the Declaration of Helsinki.
Patients
The present study included the patients who were diagnosed with treatment-naive PCV between January 2013 and October 2013 at our institution, and were initially treated with three monthly ranibizumab injections. The inclusion criteria included the following: (1) complete resolution of intraretinal/subretinal fluid a month after the third ranibizumab injection; (2) a post-diagnosis follow-up period of 12 months or longer; and (3) treatment by ranibizumab monotherapy during the 12-month follow-up period. The exclusion criteria included the following: (1) severe media opacity; (2) myopia of ≥−6.0 D and an axial length of ≥26.0 mm; (3) center-involving geographic atrophy or a disciform scar; (4) concomitant retinal vascular disorders (eg, macroaneurysms, proliferative diabetic retinopathy, and central retinal vascular occlusion); and (5) intraocular surgery during the follow-up period. When both eyes of a patient met the eligibility criteria, the eye that developed the symptoms first was included in the study.
Examination and treatment
A comprehensive ophthalmological examination, including the measurement of the best-corrected visual acuity (BCVA) and a 90 D-lens slit lamp biomicroscopy evaluation, was performed on all the patients. The photographs of the fundus, fluorescein angiography images, and indocyanine green angiography (ICGA) images were captured by combined confocal scanning laser ophthalmoscopy and spectral domain OCT (Spectralis HRA+OCT; Heidelberg Engineering GmbH, Heidelberg, Germany). The OCT scans were also performed using the Spectralis HRA+OCT device, which provides 40 000 A scans per second with 7 μm optical and 3.5 μm digital axial resolution. Horizontal and vertical OCT crosshair scans centered at the center of the fovea covering 30° were conducted. To improve visualization, 70–100 scans were averaged for each section.
The diagnosis of PCV was based on the presence of polypoidal lesions with or without branching vascular networks in the ICGA images. Choroidal vascular hyperpermeability was defined as the presence of the multifocal hyperfluorescent areas in late-phase ICGA images.14, 15 The presence of intraretinal or subretinal fluid was identified based-on OCT images. Two independent examiners (JHK and YSC) reviewed the ICGA and OCT results. Any disagreement was settled by a discussion between the two examiners. The central foveal thickness was defined as the distance between the internal limiting membrane and the Bruch’s membrane at the fovea and was manually measured using the calipers provided by Heidelberg Eye Explorer program (ver. 1.8.6.0, Heidelberg Engineering GmbH). The greatest linear dimensions of the PCV lesions, including the whole of the polypoidal lesions and the branching vascular networks, was also measured on the ICGA images using the built-in calipers of the ICGA software program. The size of the lesion, including hemorrhage, leakage from neovascularization, and staining of the retinal pigment epithelium, was also measured on the fluorescein angiography images. Two examiners (YSC and JHK) performed the measurements. The mean values of the measurements recorded by both examiners were used for further analysis.
All eyes included in the study were initially treated with three intravitreal ranibizumab injections (0.5 mg/0.05 ml) at intervals of one month. The patients were then scheduled to visit the hospital every 1–2 months at the discretion of the clinician. In some of the cases without the reactivation of PCV for a relatively longer period, the follow-up interval was extended to 3 months. Reactivation of the lesion was defined by the re-accumulation of the subretinal or intraretinal fluid on the OCT images. The fresh development of the retinal/subretinal hemorrhage observed upon clinical examination was also considered as a reactivation.
Outcome measures
The incidence and timing of the first reactivation were recorded and the cumulative incidence of reactivation was estimated on the basis of the follow-up period. The patients who experienced PCV reactivation were included in the reactivation group, whereas those who did not experience the PCV reactivation were included in the no-reactivation group. The baseline characteristics, including age and sex, intraretinal fluid, subretinal fluid, location of the polyps, greatest linear dimensions, largest polyp diameter, choroidal vascular hyperpermeability, ≥1 disc area size of the submacular hemorrhage (Figures 1a and b), presence of the grape-like polyp clusters (Figures 1c and d), central foveal thickness, and BCVA were compared between the reactivation and the no-reactivation groups.
Fundus photography (a,c) and indocyanine-green angiography (b,d) images showing submacular hemorrhage (a,b) and grape-like polyp clusters (c,d), and submacular hemorrhage in polypoidal choroidal vasculopathy. A single arrow (b) indicates polypoidal lesions and double arrows (d) indicate grape-like polyp clusters.
Statistics
The data were presented as the mean±SD where applicable. The statistical analyses were performed using a commercially available software package (SPSS, ver. 12.0 for Windows; IBM Corporation, Armonk, NY, USA). The independent samples t-test or Mann–Whitney U-test were performed to compare the parametric values. The non-parametric values were compared using the chi-square test or the Fisher’s exact test. The risk factors were analyzed by multiple Cox regression analysis. The P-values <0.05 were considered significant.
Results
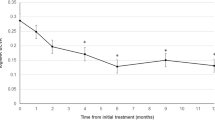
During the study period, a total of 129 patients (129 eyes) were initially treated with three ranibizumab injections at monthly intervals. None of the patients diagnosed with PCV during the study period received photodynamic therapy as the first-line treatment. Of the 129 patients, dry macula a month after the third injection was noted in 106 patients. Of these patients, 16 failed to present for the follow-up examination during the subsequent 12 months, and were excluded from the study. Additional six patients were excluded from the study on the basis of the aforementioned exclusion criteria. Ultimately, 84 eyes of 84 patients (60 male and 24 female) were included in the study (Table 1). The mean age of the patients was 67.6±7.9 years. The mean size of the lesion was 14.1±10.6 mm2. During the 12-month follow-up period, the reactivation of PCV was noted in 60 of the 84 patients (71.4%). The first reactivation was noted at a mean duration of 3.9±1.7 months (range, 2–9 months) after the third ranibizumab injection, which was equivalent to the mean duration of 5.9 months after diagnosis.
Factors associated with reactivation during the 12-month follow-up period
Table 2 summarizes the results of the comparisons of the baseline characteristics between the patients with reactivation (n=60) and those without (n=24). The mean value of the greatest linear dimension of the lesions of the reactivation group was 2.69±1.09 mm, which was significantly greater than that in the no-reactivation group (2.16±0.73 mm; P=0.033). In the reactivation group, 11 patients (18.3%) presented submacular hemorrhages and 11 (18.3%) presented the grape-like polyp clusters during the follow-up. In the no-reactivation group, submacular hemorrhages were noted in 12 of the patients (50.0%) and the grape-like polyp clusters were noted in none. The proportion of the submacular hemorrhages was significantly lower (P=0.003), and that of the grape-like polyp clusters significantly greater (P=0.029) in the reactivation group than in the no-reactivation group. There were no significant differences between the two groups in terms of the mean age (P=0.761), sex (P=0.252), intraretinal fluid (P=0.685), subretinal fluid (P=0.683), location of the polyp (P=0.084), largest polyp diameter (P=0.125), proportion of choroidal vascular hyperpermeability (P=0.094), mean central foveal thickness (P=0.117), and mean BCVA measurements (P=0.344). The results of Cox regression analysis revealed that the absence of submacular hemorrhages ≥1 disc area (P=0.035), presence of grape-like polyp clusters (P=0.009), and high values of greatest linear dimension of the lesions (P=0.036) were associated with reactivation of the lesion.
Discussion
In the present study, three factors—absence submacular hemorrhage of ≥1 disc area, grape-like polyp clusters, and large greatest linear dimension of lesions—were found to be closely associated with a high risk of reactivation of the lesion within one year of treatment.
Submacular hemorrhage is one of the frequently observed features in patients with PCV. The results of the present study revealed the association of submacular hemorrhages with a low risk of reactivation of PCV after anti-VEGF therapy. We suggest the following mechanisms as being involved in this marked difference in reactivation rates between the patients with and without submacular hemorrhage. First, the hemorrhage may have originated from the rupture of a relatively large, active, vascular lesion, such as a major polyp. The rupture of a major vascular lesion might reduce the risk of reactivation. Second, changes in retinal tissues caused by the hemorrhage may have had an influence. It is well known that myopic CNV generally shows a good prognosis after a small number of anti-VEGF injections. Indeed, after CNV regression, reactivation is noted in only a limited proportion of patients.16, 17 Conversely, in the majority of patients with neovascular AMD, CNV recurs several months after anti-VEGF injection. Campochiaro suggested that this disparity arises from extracellular matrix differences between the two disorders.18 Specifically, the abnormal extracellular matrix of AMD may promote survival signaling, making the endothelial cells in new vessels less dependent upon VEGF for survival.18 We postulate that the development of subretinal hemorrhage itself, as well as the inflammatory response that occurs during resolution of the hemorrhage, induces degeneration of the extracellular matrix, subsequent regression of CNV, and inhibition of the latter’s reactivation. Spectral-domain OCT studies have shown that the branching vascular network is located in the space between the retinal pigment epithelium and Bruch’s membrane.19, 20 The hemorrhage may affect the extracellular matrix adjacent to the branching vascular network vessels.
The compromised Bruch’s membrane is an important factor in CNV development. Animal studies have demonstrated that increased VEGF levels in the outer retina, without concomitant Bruch’s membrane disruption, are not sufficient to cause CNV.21, 22 For this reason, we postulate that the hemorrhage, as well as the inflammatory process that occurs during resolution of the hemorrhage, alters the tissue composition adjacent to the compromised Bruch’s membrane where CNV had developed. This altered tissue composition may induce a barrier effect between the sub-retinal pigment epithelial space and the choroid, thus impeding the neovascularization process. Lastly, decreased functioning of the damaged retinal tissue may also contribute to the low reactivation rate. Previous animal studies have shown that retinal outer layer tissue, including photoreceptors, have been damaged after experimental subretinal hemorrhage.23, 24 This damage can lead to reduced tissue function that, in turn, leads to a decrease in nutrients and oxygen demand. We postulate that this decrease in nutrients and oxygen demand impedes the neovascular drive of PCV lesions and, subsequently, contributes partially to low reactivation rates in patients with hemorrhages. Figure 2 depicts all our hypotheses regarding how submacular hemorrhage influences PCV reactivation.
A depiction of how submacular hemorrhage may influence reactivation of the lesion. (a) Polypoidal choroidal vasculopathy with small (asterisk) and large (double asterisks) polypoidal lesions and branching vascular networks (arrowhead). A short arrow indicates disruption of Bruch’s membrane. (b) Rupture of a large polypoidal lesion induces subretinal hemorrhage (long arrows, light gray area) accompanied by sub-retinal pigment epithelial hemorrhage (short arrows, dark grey area). (c) After resolution of hemorrhage, the major polypoidal lesion has resolved. The photoreceptor layer and outer retinal layers have degenerated (thick grey dotted line). This degenerative change leads to decreased secretion of neovascularization-inducing agents, such as VEGF. Inflammatory processes that occur during the resolution of the sub-retinal pigment epithelial hemorrhage induce sub-retinal pigment epithelial tissue changes, including changes in extracellular matrix. These in turn cause regression and consolidation of the sub-retinal pigment epithelial neovascular lesion (double arrowheads). The same changes also alter the microstructure of the tissues adjacent to the disrupted Bruch’s membrane (arrow, black thin dotted line), inducing a barrier effect between the sub-retinal pigment epithelial space and choroid. All these processes impede progression and reactivation of the neovascular lesion, even though a small polypoidal lesion (asterisk) remains. PRL: photoreceptor layer, RPE: retinal pigment epithelium.
It has been reported that the grape-like polyp-clusters are associated with a poor treatment outcome in cases with PCV.13, 25, 26 Moreover, the eyes manifesting this condition generally require frequent anti-VEGF injections.26 Recently, Lee and Lee26 reported the 2-year treatment outcome of the anti-VEGF therapy of patients with this condition; the mean number of injections required for the treatment of the condition during the 2-year follow-up period was 12.5±2.8. Considering the number of injections was between 9 and 18 in that study,26 it is unsurprising that PCV recurred in all patients. This was a markedly different result from those of Kuroda et al12 and Kang et al11 wherein PCV did not recur in 25.5% of patients during the 2-year follow-up period, and in 36% during the 3-year follow-up period, respectively. Lee and Lee26 suggested that the grape-like polypoidal lesions have a potent neovascular drive and characteristics of typical CNV, thereby requiring more frequent injections than ordinary PCVs. In the present study, all of the 11 eyes with the grape-like polyp clusters developed the reactivation of PCV during the first year, suggesting the association of a high probability of reactivation with this condition.
Recently, Kuroda et al12 suggested that the treat-and-extend regimen may lead to the redundant administration of the injections to the patients who do not develop any reactivation after the initial three injections, despite not undergoing any treatment. Considering the close association of the absence of submacular hemorrhages, presence of grape-like polyp clusters, and large lesion size with the high risk of reactivation of PCV, we propose that patients exhibiting these characteristics might be good candidates for receiving proactive treatments such as those involving the treat-and-extend regimen.
This study has certain limitations, including the retrospective nature of the study design. Furthermore, a strict monthly follow-up was not performed and variable follow-up intervals were set at the discretion of the clinician. Thus, the timing of reactivation could not be accurately estimated in some patients. All studied eyes were treated with ranibizumab; therefore, our results might not be valid in the cases of patients treated with other anti-VEGF agents. As ICGA was not routinely performed during the follow-up period, the influence of the post-treatment ICGA findings, such as the regression of the polyps, on the reactivation of PCV could not be evaluated. Reactivation was evaluated on the basis of the cross-hair OCT findings. Therefore, fluid re-accumulation outside the OCT scanning region might not have been accurately detected, particularly in peripapillary PCV cases. For this reason, our results need confirmation in further studies using raster scans covering entire macular area.
In summary, we evaluated the factors influencing the first reactivation of PCVs that were initially treated with three ranibizumab injections. During the first 12 months post diagnosis, the reactivation of PCV was observed in 71.4% of the patients. Three baseline characteristics—absence of submacular hemorrhages, presence of grape-like polyp clusters, and large lesion size—were correlated with a high risk of PCV reactivation. Frequent follow-ups may be necessary in patients who present high-risk characteristics. Further studies investigating whether patients with the high risk characteristics can be more effectively managed with the treat-and-extend regimens than with the as-needed regimens, would be of value.

References
Spaide RF, Yannuzzi LA, Slakter JS, Sorenson J, Orlach DA . Indocyanine green videoangiography of idiopathic polypoidal choroidal vasculopathy. Retina 1995; 15: 100–110.
Yannuzzi LA, Sorenson J, Spaide RF, Lipson B . Idiopathic polypoidal choroidal vasculopathy (IPCV). Retina 1990; 10: 1–8.
Laude A, Cackett PD, Vithana EN, Yeo IY, Wong D, Koh AH et al. Polypoidal choroidal vasculopathy and neovascular age-related macular degeneration: same or different disease? Prog Retin Eye Res 2010; 29: 19–29.
Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, Kim RY et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med 2006; 355: 1432–1444.
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 2006; 355: 1419–1431.
Kokame GT, Yeung L, Lai JC . Continuous anti-VEGF treatment with ranibizumab for polypoidal choroidal vasculopathy: 6-month results. Br J Ophthalmol 2010; 94: 297–301.
Oishi A, Kojima H, Mandai M, Honda S, Matsuoka T, Oh H et al. Comparison of the effect of ranibizumab and verteporfin for polypoidal choroidal vasculopathy: 12-month LAPTOP study results. Am J Ophthalmol 2013; 156: 644–651.
Cho HJ, Kim JW, Lee DW, Cho SW, Kim CG . Intravitreal bevacizumab and ranibizumab injections for patients with polypoidal choroidal vasculopathy. Eye (Lond) 2012; 26: 426–433.
Fung AE, Lalwani GA, Rosenfeld PJ, Dubovy SR, Michels S, Feuer WJ et al. An optical coherence tomography-guided, variable dosing regimen with intravitreal ranibizumab (Lucentis) for neovascular age-related macular degeneration. Am J Ophthalmol 2007; 143: 566–583.
Engelbert M, Zweifel SA, Freund KB . 'Treat and extend' dosing of intravitreal antivascular endothelial growth factor therapy for type 3 neovascularization/retinal angiomatous proliferation. Retina 2009; 29: 1424–1431.
Kang HM, Koh HJ, Lee SC . Baseline polyp size as a potential predictive factor for recurrence of polypoidal choroidal vasculopathy. Graefes Arch Clin Exp Ophthalmol 2016; 254: 1519–1527.
Kuroda Y, Yamashiro K, Miyake M, Yoshikawa M, Nakanishi H, Oishi A et al. Factors associated with recurrence of age-related macular degeneration after anti-vascular endothelial growth factor treatment: a retrospective cohort study. Ophthalmology 2015; 122: 2303–2310.
Lee WK, Kim KS, Kim W, Lee SB, Jeon S . Responses to photodynamic therapy in patients with polypoidal choroidal vasculopathy consisting of polyps resembling grape clusters. Am J Ophthalmol 2012; 154: 355–365.e351.
Sasahara M, Tsujikawa A, Musashi K, Gotoh N, Otani A, Mandai M et al. Polypoidal choroidal vasculopathy with choroidal vascular hyperpermeability. Am J Ophthalmol 2006; 142: 601–607.
Iida T, Kishi S, Hagimura N, Shimizu K . Persistent and bilateral choroidal vascular abnormalities in central serous chorioretinopathy. Retina 1999; 19: 508–512.
Calvo-Gonzalez C, Reche-Frutos J, Donate J, Fernandez-Perez C, Garcia-Feijoo J . Intravitreal ranibizumab for myopic choroidal neovascularization: factors predictive of visual outcome and need for retreatment. Am J Ophthalmol 2011; 151: 529–534.
Lai TY, Chan WM, Liu DT, Lam DS . Intravitreal ranibizumab for the primary treatment of choroidal neovascularization secondary to pathologic myopia. Retina 2009; 29: 750–756.
Campochiaro PA . Molecular pathogenesis of retinal and choroidal vascular diseases. Prog Retin Eye Res 2015; 49: 67–81.
Ojima Y, Hangai M, Sakamoto A, Tsujikawa A, Otani A, Tamura H et al. Improved visualization of polypoidal choroidal vasculopathy lesions using spectral-domain optical coherence tomography. Retina 2009; 29: 52–59.
Miura M, Makita S, Iwasaki T, Yasuno Y . Three-dimensional visualization of ocular vascular pathology by optical coherence angiography in vivo. Invest Ophthalmol Vis Sci 2011; 52: 2689–2695.
Okamoto N, Tobe T, Hackett SF, Ozaki H, Vinores MA, LaRochelle W et al. Transgenic mice with increased expression of vascular endothelial growth factor in the retina: a new model of intraretinal and subretinal neovascularization. Am J Pathol 1997; 151: 281–291.
Tobe T, Okamoto N, Vinores MA, Derevjanik NL, Vinores SA, Zack DJ et al. Evolution of neovascularization in mice with overexpression of vascular endothelial growth factor in photoreceptors. Invest Ophthalmol Vis Sci 1998; 39: 180–188.
Glatt H, Machemer R . Experimental subretinal hemorrhage in rabbits. Am J Ophthalmol 1982; 94: 762–773.
Toth CA, Morse LS, Hjelmeland LM, Landers MB 3rd . Fibrin directs early retinal damage after experimental subretinal hemorrhage. Arch Ophthalmol 1991; 109: 723–729.
Hikichi T, Higuchi M, Matsushita T, Kosaka S, Matsushita R, Takami K et al. Results of 2 years of treatment with as-needed ranibizumab reinjection for polypoidal choroidal vasculopathy. Br J Ophthalmol 2013; 97: 617–621.
Lee JH, Lee WK . Anti-vascular endothelial growth factor monotherapy for polypoidal choroidal vasculopathy with polyps resembling grape clusters. Graefes Arch Clin Exp Ophthalmol 2016; 254: 645–651.
Acknowledgements
This study was supported by Kim’s Eye Hospital Research Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kim, J., Chang, Y., Kim, J. et al. Submacular hemorrhage and grape-like polyp clusters: factors associated with reactivation of the lesion in polypoidal choroidal vasculopathy. Eye 31, 1678–1684 (2017). https://doi.org/10.1038/eye.2017.126
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.126
This article is cited by
-
Evolving treatment paradigms for PCV
Eye (2022)
-
Surgical outcomes of vitrectomy for breakthrough vitreous hemorrhage in eyes with exudative age-related macular degeneration
International Ophthalmology (2021)
-
Fibrovascular pigment epithelial detachment in eyes with subretinal hemorrhage secondary to neovascular AMD or PCV: a morphologic predictor associated with poor treatment outcomes
Scientific Reports (2020)
-
Long-term Clinical Course after Vitrectomy for Breakthrough Vitreous Hemorrhage Secondary to Neovascular Age-related Macular Degeneration and Polypoidal Choroidal Vasculopathy
Scientific Reports (2020)
-
Intravitreal aflibercept for submacular hemorrhage secondary to neovascular age-related macular degeneration and polypoidal choroidal vasculopathy
Graefe's Archive for Clinical and Experimental Ophthalmology (2020)