Abstract
The Japanese Society of Hypertension (JSH) updated its hypertension management guidelines in 2009. One of the most significant changes with respect to the 2004 version was the stance towards the use of diuretics: in 2004, their use was cautioned against, but in 2009, it was actively promoted. The purpose of this study was to measure the impact of this change in guidelines on prescription patterns for antihypertensive medications, and to investigate the overall trend in the use of antihypertensives. We used monthly claims data obtained from a database company. Data of patients who were 20 or more years old and prescribed antihypertensives were extracted and analyzed. There were 66 223 patients who were prescribed antihypertensives (mean age 53.6±11.0). Of these, 38 130 were men and 28 093 were women. The two most prescribed classes of antihypertensives were angiotensin receptor blockers, whose usage steadily increased over a 7-year period, and calcium channel blockers. Prescriptions for antihypertensives in these two classes were also more likely to be continued than those for other antihypertensive classes. The prescription rate for diuretics increased from December 2006 (P<0.0001), but the rate of increase was the same before and after 2009 (P=0.09). The clinical guidelines published in 2009 had no apparent impact on the trend of diuretic prescriptions, despite the radical change in stance concerning the use of antihypertensives. Further effort to disseminate the content of these guidelines, so that it is reflected in actual clinical practice, may be warranted.
Similar content being viewed by others
Introduction
In 2009, the Japanese Hypertension Society updated its guidelines for the management of hypertension (JSH2009). Many changes from the 2004 version were made, one of the most prominent being the stance towards the use of diuretics, especially thiazides. In the 2004 version of the guidelines, thiazides and thiazide-like diuretics were listed as agents prone to cause hypokalemia, which, if severe, increases the risk of arrhythmias and sudden death. The 2004 version continued with a listing of numerous adverse effects, such as gout, hyperlipidemia, glucose intolerance, erectile dysfunction, concentration of the blood due to dehydration and photosensitivity dermatitis.1 It then went on to say that ‘due to the possibility that the adverse effects of thiazides on the metabolic system may be harmful to the long-term outcome, it should be prescribed in low-doses’, conveying a rather negative attitude towards the use of such diuretics.
In contrast to this stance, the first paragraph of the section describing diuretics in the 2009 guidelines begins with a sentence reprimanding the low usage of diuretics in Japan, saying that ‘According to various surveys, the frequency of hypertensive patients treated with diuretics is markedly low in Japan, being less than 10%’.2 It then continues that, as Japanese people consume a lot of salt, it is important that they restrict salt intake, and more frequent use of diuretics is recommended. It also states that using diuretics is economically advantageous due to their low cost.
This dramatic change in attitude towards the prescription of diuretics might be responsible for measurable changes in actual prescription patterns. Using a claims database, this study was conducted to test the hypothesis that the changed content in JSH2009 positively affected the trend of diuretic prescriptions, especially for thiazides and thiazide-like diuretics, in addition to investigating the overall pattern of antihypertensive prescription in Japan.
Methods
Data source and management
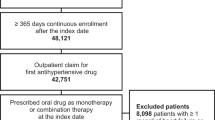
Monthly claims data (from January 2005 to October 2011) were obtained from a database company.3 The population covered by the database consisted of insurees and their dependents belonging to one of several health insurance unions in Japan. For each patient, the data consisted of an encrypted personal identifier, age and gender, procedures carried out, diagnosis name and diagnosis code according to ICD10, and prescribed drugs. Drug information included the month and year of prescription, brand name and generic name, dosage and number of days prescribed. Of the total one million patients in the database, those whose diagnosis name included ‘hypertension’ at least once and were at or over 20 years of age were initially extracted. However, not all patients with a hypertension diagnosis were prescribed antihypertensives, therefore the group was restricted to those who were prescribed any kind of antihypertensive at least once. Most prescription periods ranged from 14 days to 3 months. We intended to determine the frequency of drug prescriptions per patient per month. In order to do this, multiple prescriptions for a given drug during a single month were counted only once. For prescription periods of 2 months, data were generated for the month following the first month and added to the original database. For prescription periods of 3 months or more, data were generated for the 2 months following the initial month and added to the original database. Patients who had undergone coronary revascularization were extracted by searching the procedure database using codes representing either some form of percutaneous coronary intervention or coronary artery bypass graft operation. Patients who were on maintenance dialysis were extracted by searching the procedure database using a code representing a special fee for maintenance dialysis. Patients who were prescribed at least one type of antidiabetic drug or statin drugs were extracted by searching the prescription database.
Statistical analysis
Our initial hypothesis was that the prominent change regarding the recommendation of diuretics in the JSH2009 exerted enough influence on physicians so that we would observe a significant difference in the prescription rate of diuretics before and after the publication of JSH2009. Thus, we initially planned to compare the prescription trend between the two periods. However, when we actually plotted the prescription rate for the entire observation period, it was obvious that there was significant change in the trend of diuretics usage beginning at around the end of 2006. Thus, we changed our initial plan and compared the trend among the three periods. To test the difference of slopes of diuretic usage trends across different periods, we used an analysis of covariance, with the monthly prescription rate as the dependent variable, and the three period groups (2005/1–2006/11, 2006/12–2009/1, 2009/2–2011/10) and time since each initial time point as the independent variables. An analysis of covariance model included an interaction term between period group and time. To investigate how long each drug class was prescribed, survival analyses of the drug classes were performed as follows: first, only data on patients who were prescribed antihypertensive drugs for at least a prescription period of 4 months were included. Prescription period was defined as from the time of first prescription to the time of last prescription. Then, those who were prescribed for 75% or more months during the prescription period were extracted. Drug classes were judged to be terminated when they were not prescribed for 3 or more consecutive months. Survival curves are presented using the Kaplan–Meier method and time to discontinuation of drug was compared between drug classes using the proportional hazard frailty model with the Tukey–Kramer’s method.
All P-values for statistical tests are two-sided. All statistical analyses were performed using Stata 12.1 (Stata Corporation, College Station, TX, USA)
Ethical considerations
The data used in this study were completely anonymized and informed consent from the subjects was not necessary. This study was approved by the ethical committee of the University of Tokyo.
Results
As shown in Table 1, there were 66 223 patients who were prescribed at least one antihypertensive drug at least once during the period from January 2005 to October 2011. Of these, 38 130 were men and 28 093 were women. The mean age of the overall population was 53.6±11.0 years. The mean age of the women was 54.9±11.9 years and that of the men was 52.6±10.2 years. As shown in Figure 1, the distribution was skewed towards those who were 60 years of age or younger (skewness=−0.276). The number of patients who were prescribed at least one antidiabetic drug at least once was 9750 (14.7%). The number of those who underwent at least one procedure of coronary revascularization (percutaneous catheter intervention or coronary bypass grafting) was 846 (1.3%). The number of those who were under chronic hemodialysis was 537 (0.8%). The number of those who were prescribed at least one statin at least once was 19 485 (29.4%).
Figure 2 shows the rate of prescription for each drug class, from January 2005 to October 2011. While the prescription rate for calcium channel blockers (CCBs) remained almost constant, that for angiotensin receptor blockers (ARBs) showed a nearly constant increase. The prescription rates for other drug classes, except for diuretics, showed constant declines during this period.
Prescription rate for each drug class, by month. Each drug class was counted once per month per patient and divided by the number of patients that were prescribed antihypertensives each month. ACE-I, angiotensin converting enzyme inhibitor; AB, alpha blocker; BB, beta blocker; ARB, angiotensin receptor blocker; CCB, calcium channel blocker.
Figure 3 shows the rate of prescription for diuretics alone. As shown, the prescription rate for diuretics remained constant until December 2006 and steadily increased thereafter. When the slope of the diuretic prescription rate for the period from January 2005 to November 2006 was compared with that for the period from December 2006 to January 2009, a significant difference was apparent (P<0.0001). However, a similar prescription rate comparison for the period of December 2006 to January 2009, when JSH2009 was published, with the period from February 2009 to October 2011, showed no significant difference (P=0.090).
Prescription rates for diuretics, by month. A trend of an increasing number of prescriptions was observed from January 2007. The 2009 guidelines for the management of hypertension were published in January 2009. The dotted lines represent regression lines for the following periods: January 2005–December 2006; January 2007–January 2009 and February 2009–October 2011.
Figure 4 shows that the rate of single-pill ARB/diuretics combination drugs, among diuretics overall, showed a steady increase since December 2006.
Figure 5 shows the time-to-termination curves for several classes of antihypertensives. The survival rates of patients prescribed CCBs and ARBs were the highest, and almost similar (P=0.9736). The drug class with the third highest survival rate was the beta-blockers (BBs), but it was significantly lower compared with either the ARB (P<0.0001) or CCB (P<0.0001) class. The survival rate of patients prescribed diuretics was significantly lower than that for either ARB (P<0.0001) or CCB (P<0.0001) drugs. The complete comparison matrix is shown in Supplementary Table S1.
Discussion
We found that despite a prominent change in the 2009 guidelines concerning the stance towards the use of diuretics for the management of hypertension, the impact that this change had on actual clinical practice was not clearly observed. A more significant change in clinical practice was observed prior to the publication of JSH2009, starting around December 2006, when a medication combining an ARB, losartan and hydrochlorothiazide as a single pill became available.
Prior to conducting this study, we hypothesized that the change in stance towards the use of diuretics as antihypertensives included in JSH2009, compared with JSH2004 recommendations, should have led to a significantly increased rate of diuretic prescriptions. However, as shown in Figure 2, although the rate of diuretic prescriptions was increasing, the trend started before the publication of JSH2009, and there was no significant acceleration after publication. The results of our study indicate two points. One is the absence of an accelerated increase in prescription rates for diuretics after the publication of JSH2009, and the other is the trend toward an increasing rate of diuretic prescriptions that started around December 2006.
Concerning the absence of an accelerated increase in the prescription rates of diuretics after the publication of JSH2009, it is quite possible that the key messages of the guidelines were poorly conveyed to physicians. When wording in JSH2004 and JSH2009 is compared, although the change in attitude towards diuretics is prominent in the chapter parts that explain the individual drug classes, the respective stances toward the prescription of diuretics are not very obvious in the main part of each chapter. JSH2004 did not negate the use of diuretics, but stated that the use of each class of antihypertensive should be optimized and that diuretics were suitable for the elderly, and patients with congestive heart failure or chronic kidney disease. Thus, although JSH2009 explicitly stated that diuretics should be used as first-line antihypertensives along with CCBs, ARBs, BBs and angiotensin-converting enzyme inhibitors, this significant change in stance might have been overlooked if physicians only read the general part of the drug selection chapter. In fact, a recent report showed that the recognition rate of the existence of the hypertension management guidelines themselves was quite high,4 suggesting a possible failure to communicate the content of the guidelines.
In 1996, Pathman5 proposed a four-step model of physicians’ changes in behavior, namely, that physicians need to be aware of, agree with, adopt and adhere to guidelines. A recent article reviewed several studies on physicians’ adherence to clinical guidelines, to investigate different patterns of ‘leakage’ (that is, departure from guideline recommendations) in the utilization of clinical guidelines.6 It revealed that adherence rates varied among different guidelines but that the leakage was progressive across all four steps in the studies reviewed. This accords with our results, in that although the recognition rate of the existence of the guidelines is high,4 their key messages were not reliably transferred to physicians and were not reflected in clinical practices.
There have been reports of ways to improve physicians’ adherence to guideline recommendations. A trial in Italy recruited 1120 internists from around the country to participate in a workshop to discuss hypertension management, so that a consensus could be reached.7 In Canada, a non-profit organization is striving to disseminate the recommendations for hypertension therapies to target groups throughout the country.8 A study that evaluated the efficacies of various types of traditional dissemination activities in changing physicians’ behavior found that there is some evidence that interactive continuing medical education sessions can effect change in professional practice, but didactic sessions do not appear to be effective.9 These studies indicate that considerable effort would be needed to ensure that physicians are not only aware of guidelines, but that they also agree with their precepts, adopt them, and ultimately adhere to guideline recommendations in practice.
Another reason that the increase in the rate of diuretic prescriptions did not accelerate after the publication of JSH2009 might be that diuretics do possibly cause several adverse effects, and this might have prevented physicians from adopting diuretics as antihypertensive drugs at a more rapid pace, despite their promotion in JSH2009. In fact, the survival curves in Figure 5 illustrate that diuretic prescriptions tend to be terminated more frequently than those of other drug classes such as CCBs, ARBs and BBs. A previous study showed that patient-reported adverse events tend to be higher with diuretics compared with those in other classes of antihypertensives.10
Concerning the increase in the diuretic prescription rate starting around December 2006, this might have been the result of pharmaceutical companies’ promotions of their drugs. Thiazides and thiazide-like diuretics are the oldest type of antihypertensive drugs, and older drugs, especially after their patents have expired, are not promoted by pharmaceutical companies. However, a single-pill losartan/hydrochlorothiazide was made available at the end of 2006 and was promoted as a ‘new drug’. Several other companies have also started selling single-pill ARB/hydrochlorothiazide combination drugs in Japan, which might have been the reason for the observed sustained increasing rate of diuretic prescriptions. This is supported by the increasing prescription rate for single-pill combination drugs in diuretic prescriptions shown in Figure 4.
As for the overall trend in prescription rate for each drug class, CCBs remained the most preferred class of antihypertensive drug, although ARBs have recently approached their popularity. These two classes of drugs also showed longer periods of continual use than those of other classes of drugs. Although the exact reasons why these drug classes were preferred and prescribed for longer periods could not be determined from the data, we surmise that both these drug classes are as effective as other drug classes and have fewer adverse effects.
As for the changes from JSH2004 to JSH2009 for other classes of antihypertensives, alpha-blockers were downgraded to drugs that lack sufficient evidence for cardiovascular risk reduction. Their prescription rate was declining at a constant pace since 2005, and the trend did not change with the publication of JSH2009.
In conclusion, despite a prominent change in attitude towards the prescription of diuretics in the transition from JSH2004 to JSH2009, a significantly accelerated rate of diuretic prescriptions was not observed. One possible reason might be the failure to effectively communicate the content of changed recommendations to physicians. If this is the case, then an effective mechanism should be sought for disseminating key changes, so that physicians can take advantage of future guideline revisions and adhere to such recommendations in actual clinical care settings.
Limitations
This study has several limitations. First, the database used in this study included only patients who were employed by large companies and did not include patients employed in small businesses, the self-employed or retirees. Thus, the population included in this study might differ from the general population in terms of income level and age distribution. However, the way the statutory healthcare insurance system is set up in Japan permits physicians to prescribe any drug and be reimbursed as long as they are medically justified. Thus, is it not very likely that the income level affected the prescription pattern of physicians, although clear evidence is lacking in literature. The skewness in age distribution may have introduced some bias into the obtained results, but the prescription patterns for patients over 60 years of age were not greatly different from those of patients between 40 and 60 (data not shown), suggesting that the observed prescription patterns would not have varied greatly if the older population were excluded in this study. However, it still may render the result difficult to be generalized for the whole prescription pattern in Japan. Secondly, antihypertensives are not only used to treat hypertension, but also angina, congestive heart failure, and arrhythmias. Thus, data in the current study includes patients who had congestive heart failure, paroxysmal supraventricular tachycardia and other diseases, rather than hypertension. However, as the population covered in this study was based on health insurance data and not those of hospital cohorts, the number of non-hypertensive patients compared to the number of hypertensive patients should have been small, and therefore, little effect upon the overall conclusion of this study would be expected. Thirdly, there was no data for separating the impact of the availability of single-pill ARB/hydrochlorothiazide drugs and the impact of the guidelines, and the possibility that both contributed to the increasing trend remains.
References
Japanese Society of Hypertension. Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2004). Hypertens Res 2006; 29 (Suppl): S1–S105.
Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ito S, Iwao H, Kario K, Kawano Y, Kim-Mitsuyama S, Kimura G, Matsubara H, Matsuura H, Naruse M, Saito I, Shimada K, Shimamoto K, Suzuki H, Takishita S, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Ueshima H, Umemura S, Ishimitsu T, Rakugi H . The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2009). Hypertens Res 2009; 32: 3–107.
Kimura S, Sato T, Ikeda S, Noda M, Nakayama T . Development of a database of health insurance claims: standardization of disease classifications and anonymous record linkage. J Epidemiol 2010; 20: 413–419.
Ikeda N, Hasegawa T, Saito I, Saruta T . Awareness of the Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2000) and compliance to its recommendations: surveys in 2000 and 2004. J Hum Hypertens 2006; 20: 263–266.
Pathman DE, Konrad TR, Freed GL, Freeman VA, Koch GG . The awareness-to-adherence model of the steps to clinical guideline compliance. The case of pediatric vaccine recommendations. Med Care 1996; 34: 873–889.
Mickan S, Burls A, Glasziou P . Patterns of ‘leakage’ in the utilisation of clinical guidelines: a systematic review. Postgrad Med J 2011; 87: 670–679.
Malacco E, Ferri C, Grandi AM, Kilama MO, Soglian AG, Vigna L . Treatment of hypertension and adherence to treatment guidelines in clinical practice: an Italian study. Adv Ther 2005; 22: 96–106.
Tobe SW, Touyz RM, Campbell NR . The Canadian Hypertension Education Program - a unique Canadian knowledge translation program. Can J Cardiol 2007; 23: 551–555.
Davis D, O'Brien MA, Freemantle N, Wolf FM, Mazmanian P, Taylor-Vaisey A . Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA 1999; 282: 867–874.
Chen K, Chiou CF, Plauschinat CA, Frech F, Harper A, Dubois R . Patient satisfaction with antihypertensive therapy. J Hum Hypertens 2005; 19: 793–799.
Acknowledgements
This work was supported by a grant from the Japanese Ministry of Economy, Trade and Industry and by the Japan Society for the Promotion of Science (JSPS), through the ‘Funding Program for World-Leading Innovative R&D on Science and Technology (FIRST Program),’ initiated by the Council for Science and Technology Policy (CSTP).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Kohro, T., Yamazaki, T., Sato, H. et al. The impact of a change in hypertension management guidelines on diuretic use in Japan: trends in antihypertensive drug prescriptions from 2005 to 2011. Hypertens Res 36, 559–563 (2013). https://doi.org/10.1038/hr.2012.216
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2012.216
Keywords
This article is cited by
-
Analysis of antihypertensive treatment using real-world Japanese data—the retrospective study of antihypertensives for lowering blood pressure (REAL) study
Hypertension Research (2019)
-
A nationwide survey on non-B, non-C hepatocellular carcinoma in Japan: 2011–2015 update
Journal of Gastroenterology (2019)
-
Current prescription status of antihypertensive drugs with special reference to the use of diuretics in Japan
Hypertension Research (2017)
-
Analysis of second- and third-line antihypertensive treatments after initial therapy with an angiotensin II receptor blocker using real-world Japanese data
Hypertension Research (2016)
-
Safety and clinical outcome in combination therapy for high-risk elderly hypertensive patients
Hypertension Research (2015)