Abstract
Hyperuricemia is common among patients with hypertension and metabolic syndrome and therefore may be a cause of or result from these comorbid conditions. Few studies, however, have examined the relationship between the presence–absence of hyperuricemia and changes in the estimated glomerular filtration rate (eGFR) using the large cohort of the general population. We examined subjects who participated in two screenings, in 1993 and 2003, in Okinawa, Japan, yielding data on serum creatinine and uric acid levels (N=16 630). eGFR (ml min−1 per 1.73 m2) was calculated using the formula used by the Japanese Society of Nephrology. In both sexes, a uric acid (UA) level >7.0 mg dl−1 was defined as hyperuricemia (H), and a UA level below that threshold was classified as normouricemia (N). Based on the absence or presence of hyperuricemia in both the 1993 screening and the 2003 screening, we categorized patients into four groups: group 1, N/N; group 2, H/N; group 3, N/H; and group 4, H/H. Multiple regression analysis was performed to estimate the independent effects of several variables on the decline in eGFR. In all groups, an increase in UA from 1993 to 2003 (ΔUA) was a strong independent risk factor for a decline in eGFR than that of the baseline levels of UA, the presence of hypertension, or diabetes. The estimated decline in eGFR per 1 mg dl−1 increase in UA was 4.19, 1.91, 2.36 and 2.01 ml min−1 per 1.73 m2 in groups 1, 2, 3 and 4, respectively. The results suggest that UA has a role in chronic kidney disease (CKD) progression. We have no information on medications used, such as xanthine oxidase, uricosuric drugs and hypotensives; therefore, the impact of hyperuricemia might be underestimated in our analysis. The results suggest that maintaining a normal range of UA is important to maintain eGFR decline in a normal range.
Similar content being viewed by others
Introduction
Hyperuricemia, defined as a UA level >7.0 mg dl−1, is often observed in patients with hypertension and diabetes mellitus (DM), which are the leading causes of end-stage renal disease.1 Recently, hyperuricemia has been recognized as a risk factor in CKD incidence and progression.2 It is often associated with metabolic syndrome and obesity, which are prevalent in developed countries.3, 4 Moreover, hyperuricemia is associated with the onset of type 2 DM5 and stroke.6
In addition to the basal levels of UA, changes in UA are suggested to be a determinant of glomerular filtration rate (GFR) change. However, the precise relationship between estimated GFR (eGFR) and UA is largely unknown, and no large cohort study has been conducted to elucidate this relationship.7 We investigated the changes in eGFR and UA among screened cohorts in Okinawa using the newly established eGFR formula for Japanese patients. The serum levels of creatinine and UA in the participants were measured at a screening in both 1993 and 2003.
Methods
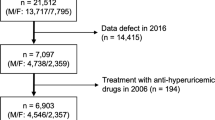
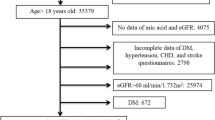
Individual records for 16 630 participants who were screened in both 1993 and 2003 by the Okinawa General Health Maintenance Association (OGHMA) were examined in this study. The study was approved by the Institutional Review Board at Ryukyu University and the equivalent committee at the OGHMA.
Screening program
The OGHMA is a nonprofit organization, founded in 1972, that conducts a large annual community-based health examination.8, 9, 10 Once each year, the staff, doctors and nurses visit residences and workplaces throughout the prefecture to perform health examinations. All subjects voluntarily participated in the screening. The OGHMA personnel provided mass screening, informed the participants of the results, and, when necessary, recommended further evaluation or treatment. This process included an interview concerning health status, a physical examination and urine and blood tests. A nurse or doctor measured blood pressure using a standard mercury sphygmomanometer with the subject in a sitting position. Dipstick testing for proteinuria (Ames dipstick, Tokyo, Japan) was performed in spontaneously voided fresh urine. Proteinuria was assessed by a technician as negative, trace, 1+, 2+, 3+ or 4+. A score of 1+ and higher was regarded as proteinuria. For this study, we excluded those patients with proteinuria scores of 2+ and higher. A blood sample was taken after an overnight fast. The blood was analyzed at a central laboratory at the OGHMA. Body mass index was calculated as weight (kg) divided by the square of the height (m). Obesity was defined as BMI⩾25 kg m–2, and hypertension was defined as systolic blood pressure ⩾140 mm Hg or diastolic blood pressure⩾90 mm Hg. DM was defined as fasting blood glucose ⩾126 mg dl−1.
Computer-based data were available from 1 April 1993 through 31 March 1994 (n=143 948), for the 1993 screening and from 1 April 2003 through 31 March 2004, for the 2003 screening. Participants who were screened at both screenings were identified using ID number, birthdates and other identifiers. In addition to formulaic matching, all matches were visually inspected to confirm their accuracy. We identified 44 230 subjects who participated in both the 1993 screening and the 2003 screening (30.7% of the total). For this study, we selected those subjects who had measurements of serum creatinine and UA at both screenings, totaling 16 796 subjects (men 7495 and women 9301). We excluded subjects with proteinuria, assessed as dipstick 1+ and higher.
Serum creatinine was measured using a modified Jaffe reaction (1993) and enzymatic method (2003) in an auto-analyzer at the OGHMA laboratory. After converting the serum creatinine value of 1993 to that of the enzymatic method,11 the eGFR was calculated using the Japanese Society of Nephrology formula.12 Subjects who were already on chronic dialysis were excluded from the cohort. Only coded data sets were used for this study. In both sexes, a UA level >7.0 mg dl−1 was defined as hyperuricemia (H), and a UA level below that threshold was classified as normouricemia (N). Based on the absence or presence of hyperuricemia in both the 1993 screening and the 2003 screening, we categorized patients into four groups: group 1, N/N; group 2, H/N; group 3, N/H; and group 4, H/H.
Statistical analysis
Data were analyzed with SAS statistical software (version 9.23, SAS Institute, Cary, NC, USA). Demographic data were presented as the mean (s.d.) for quantitative variables and absolute number (%) for frequencies. Student’s t-test and analyses of covariance were performed to compare the significance of discrete variables. Stepwise multiple regression analysis was performed to estimate the independent effect of several variables on decline in eGFR. A P-value of <0.05 was considered statistically significant in all analyses.
Results
Baseline characteristics of the study participants are summarized in Table 1. Over 10 years, the eGFR decreased 9.6 ml min−1 per 1.73 m2 and serum uric acid increased 0.2 mg dl−1 (both P<0.0001). Proteinuria developed in 961 subjects (6.0%).
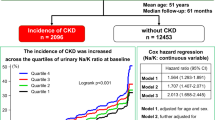
Table 2 summarizes the changes in clinical demographics and changes in eGFR (ΔeGFR) by changes in UA (ΔUA) in groups 1–4, with the groups categorized by the baseline levels of eGFR. We observed that 8.5% of the total screened population remained hyperuricemic, particularly men. An increase in UA was associated with a decrease in eGFR regardless of comorbid patterns of hyperuricemia and the baseline levels of eGFR.
Table 3 summarizes the risk factors for a decline in eGFR estimated by a multiple regression model in groups 1–4. In all groups, an increase in UA was a strong independent risk factor for a decline in eGFR compared with the baseline level of UA as well as for the presence of hypertension or DM in 1993. The estimated decline in eGFR per 1 mg dl−1 increase in UA was 4.19, 1.91, 2.36 and 2.01 ml min−1 per 1.73 m2 in groups 1, 2, 3 and 4, respectively. These results were also observed for women, even when the definition for hyperuricemia was >6.0 mg dl−1 (data not shown).
Changes in eGFR (ΔeGFR) were associated with ΔUA, in both men (Figure 1) and women (Figure 2; P<0.001 analysis of covariance). Changes in eGFR are summarized for each group according to the baseline levels of eGFR (Figure 3). At each level of baseline eGFR, groups with increased UA (N/H and H/H) seemed to show lower eGFR compared with those with unchanged or decreased UA (N/N and H/N).
Changes in estimated glomerular filtration rate (eGFR) from baseline levels of eGFR in each group. Based on the absence or presence of hyperuricemia (H) in the 1993 and 2003 screenings, we categorized patients into four groups: N/N (●), H/N (▴), N/H (♦) and H/H (▪). Hyperuricemia was defined as serum uric acid ⩾7.0 mg dl–1 in both sexes, and >7.0 mg dl–1 was defined as normouricemia (N).
Discussion
This study demonstrates the significance of hyperuricemia for a decline in eGFR among the screened subjects, thus supporting our previous observation.13, 14 Hyperuricemia is common among patients with hypertension and DM because of the increase in the prevalence of obesity and metabolic syndrome in these patients. The presence of metabolic syndrome has been reported to be associated with the prevalence15 and incidence of CKD.7, 16 The higher number of comorbid conditions, such as hypertension, hyperglycemia and lipidemia related to obesity, increases the prevalence of hyperuricemia. The reasons for the increase in serum uric acid or the maintained hyperuricemic levels are not clear from the results of this study. This cohort participated voluntarily and therefore was a self-selected population.
Hyperuricemia has several unexpected effects on kidney function, even without hypertension.1 The beneficial effects of angiotensin II receptor blockade are also explained by the associated effect of lowering serum levels of uric acid.2, 17 Several statins lower the serum UA levels, and the beneficial effect of statins on cardiovascular events could be related to its lowering effect on serum UA levels.18
Significant changes in risk factors and treatments may have occurred during the study period. Angiotensin II receptor blockers, which may reduce the uric acid level, have been available since 1998 in Japan. Hyperuricemia with gout would have been treated, if needed, by conventional medicine, such as xanthine oxidase inhibitor and/or uricosuric agent. A new type of xanthine oxidase inhibitor, febuxostat, was introduced in Japan in 2011.
The causes of the greater decline in eGFR are not clear from the results of this study. The age-related decline of GFR is relatively small in the general Japanese population.19 In this study, a greater decline in GFR was observed among those who had increased levels of serum UA over a 10-year period. Several papers have reported the benefit of treating hyperuricemia on the progression of CKD, particularly for patients with gout. However, whether the asymptomatic hyperuricemia should be treated remains unknown. Hyperuricemia may be related to other lifestyle-related factors, such as alcohol consumption, smoking and socioeconomic stress. Unfortunately, such information is not available in this study.
Early detection and treatment are important to prevent the progression of CKD and therefore the incidence of cardiovascular disease and end-stage renal disease. Based on the recent Kidney Disease: Improving Global Outcomes (KDIGO) meta-analyses, classifications of CKD based on both GFR (namely, serum creatinine) and albuminuria have been proposed.20 Subjects with hyperuricemia usually do not have albuminuria or proteinuria, and therefore these conditions may be ignored with regard to medical attention. The population in Japan is ageing. Therefore, the number of CKD patients, particularly those with CKD stage 3a, A1, will increase. These patients are the targets for life-style modification, which would be the most cost-effective method of preventing cardiovascular disease and end-stage renal disease. Although the number of studies is small, there are reports supporting the treatment of asymptomatic hyperuricemia.21, 22, 23 In this regard, the effect of uric acid-lowering agents should be evaluated in the future.
There are several limitations to our study. First, the study subjects were relatively healthy individuals who were concerned about their health status and should therefore be considered a self-selected population. The prevalence of CKD remained stable while the prevalence of obesity increased and the prevalence of hypertension decreased from 1993 to 2003.9 As in other large-cohort studies, the follow-up was passive. Some of the individuals who participated in the screening may already have been treated for gout or hyperuricemia. Unfortunately, information on the use of such medication is not available. Treatment of hyperuricemia or gout and the use of angiotensin receptor blockers may decrease the serum levels of uric acid, thus blunting the relationship between the changes in UA and eGFR. CKD prevalence was comparable between the groups and similar to that in other parts of Japan.19 As reported, a new-type of xanthine oxidase inhibitor has shown beneficial effects on kidney function with the degree of changes in UA.24 Second, the causes of hyperuricemia were not clear from the results of this study. Acute deterioration of GFR may accompany hyperuricemia or vice versa. However, the likelihood of this possibility is low because we adopted two time points that were 10 years apart. Moreover, the magnitude of change in UA was significantly associated with the change in eGFR. Several lifestyle-related factors such as smoking, alcohol intake and exercise habits may explain the change in serum levels of uric acid. Third, the relative homogeneity of the Okinawa population enhanced the internal validity of our results. Our findings remain to be confirmed in other parts of Japan and in other races, however. Finally, the cutoff point for hyperuricemia (>7.0 mg dl−1) that was used in this study was arbitrary; however, this cutoff is accepted as the guideline for the management of hyperuricemia and gout.25 The effect of hypouricemia, <5.0 mg dl−1, remains to be studied.
In conclusion, this study suggests that maintaining serum levels of uric acid in a normal range is important to maintain eGFR decline within a normal range. Hyperuricemia >7.0 mg dl−1 is an independent predictor of the progression of CKD and therefore end-stage renal disease incidence. In this regard, careful monitoring of lifestyle leading to hyperuricemia is important and probably warranted among those with obesity and metabolic syndrome. Future intervention studies on the subjects with asymptomatic hyperuricemia are needed.
References
Feig DI, Kang DH, Johnson RJ . Uric acid and cardiovascular risk. N Engl J Med 2008; 359: 1811–1821.
Yu M, Sanchez-Lozada LG, Johnson RJ, Kang DH . Oxidative stress with an activation of the renin-angiotensin system in human vascular endothelial cells as a novel mechanism of uric acid-induced endothelial dysfunction. J Hypertens 2010; 28: 1234–1242.
Kambham N, Markowitz GS, Valeri AM, Lin J, D'Agati VD . Obesity-related glomerulopathy: an emerging epidemic. Kidney Int 2001; 59: 1498–1509.
Sowers JR . Metabolic risk factors and renal disease. Kidney Int 2007; 71: 719–720.
Bhole V, Choi JW, Kim SW, de Vera M, Choi H . Serum uric acid levels and the risk of type 2 diabetes: a prospective study. Am J Med 2010; 123: 957–961.
Kim SY, Guevara JP, Kim KM, Choi HK, Heitjan DF, Albert DA . Hyperuricemia and risk of stroke: a systemic review and meta-analysis. Arthritis Rheum 2009; 161: 885–892.
Tanaka H, Shiohira Y, Uezu Y, Higa A, Iseki K . Metabolic syndrome and chronic kidney disease in Okinawa, Japan. Kidney Int 2006; 69: 369–374.
Iseki K, Iseki C, Ikemiya Y, Fukiyama K . Risk of developing end-stage renal disease in a cohort of mass screening. Kidney Int 1996; 49: 800–805.
Iseki K, Ikemiya Y, Iseki C, Takishita S . Proteinuria and the risk of developing end-stage renal disease. Kidney Int 2003; 63: 1468–1474.
Iseki K . The Okinawa screening program. J Am Soc Nephrol 2003; 14 (Suppl 2): S127–S130.
Iseki K, Kinjo K, Iseki C, Takishita S . Relationship between predicted creatinine clearance and proteinuria and the risk of developing ESRD in Okinawa, Japan. Am J Kidney Dis 2004; 44: 806–814.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A . Collaborators developing the Japanese equation for estimated GFR. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 2009; 53: 982–992.
Iseki K, Oshiro S, Tozawa M, Iseki C, Ikemiya Y, Takishita S . Significance of hyperuricemia on the early detection of renal failure in a cohort of screened subjects. Hypertens Res 2001; 24: 691–697.
Iseki K, Ikemiya Y, Inoue T, Iseki C, Kinjo K, Kinjo K, Takishita S . Significance of hyperuricemia as a risk factor of developing ESRD in a screened cohort. Am J Kidney Dis 2004; 44: 642–650.
Chen J, Muntner P, Hamm LL, Jones DW, Batuman V, Fonseca V, Whelton PK, He J . The metabolic syndrome and chronic kidney disease in U.S. adults. Ann Intern Med 2004; 140: 167–174.
Tozawa M, Iseki C, Tokashiki K, Chinen S, Kohagura K, Kinjo K, Takishita S, Iseki K . Metabolic syndrome and risk of developing chronic kidney disease in Japanese adults. Hypertens Res 2007; 30: 937–943.
Hoieggen A, Alderman MH, Kjeldsen SE, Julius S, Devereux RB, De Faire U, Fyhrquist F, Ibsen H, Kristianson K, Lederballe-Pedersen O, Lindholm LH, Nieminen MS, Omvik P, Oparil S, Wedel H, Chen C, Dahlöf B LIFE Study Group. The impact of serum uric acid on cardiovascular outcomes in the LIFE study. Kidney Int 2004; 65: 1041–1049.
Athyros VG, Athyros VG, Elisaf M, Papageorgiou AA, Symeonidis AN, Pehlivanidis AN, Bouloukos VI, Milionis HJ, Mikhailidis DP, GREACE Study Collaborative Group. Effect of statins versus untreated dyslipidemia on serum uric acid levels in patients with coronary heart disease: a subgroup analysis of the GREek Atorvastatin and Coronary-heart-disease Evaluation (GREACE) study. Am J Kidney Dis 2004; 43: 589–599.
Imai E, Horio M, Yamagata K, Iseki K, Hara S, Ura N, Kiyohara Y, Makino H, Hishida A, Matsuo S . Slower decline of glomerular filtration rate in the Japanese general population: a longitudinal 10-year follow-up study. Hypertens Res 2008; 31: 433–441.
Chronic Kidney Disease Prognosis Consortium, Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, de Jong PE, Coresh J, Gansevoort RT . Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet 2010; 375: 2073–2081.
Siu YP, Leung KT, Tong MKH, Kwan TH . Use of allopurinol in slowing the progression of renal disease through its ability to lower serum uric acid level. Am J Kidney Dis 2006; 47: 51–59.
Goicoechea M, de Vinuesa SG, Verdalles U, Ruiz-Caro C, Ampuero J, Rincón A, Arroyo D, Luño J . Effect of allopurinol in chronic kidney disease progression and cardiovascular risk. Clin J Am Soc Nephrol 2010; 5: 1388–1393.
Cain L, Shankar A, Ducatman AM, Steenland K . The relationship between uric acid and chronic kidney disease among Appalachian adults. Nephrol Dial Transplant 2010; 25: 3593–3599.
Whelton A, Macdonald PA, Zhao L, Hunt B . Renal function in gout: long-term treatment effects of febuxostat. J Clin Rheumatol 2011; 17: 7–13.
Guideline for the management of hyperuricemia and gout. Second Edition, 2010. Japanese Society of Gout and Nucleic Acid Metabolism.
Acknowledgements
We are indebted to the staff of the OGHMA, particularly Mr M Itokazu and Mr K Shiroma, for retrieving data files from the 1993 to 2003 screenings.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Iseki, K., Iseki, C. & Kinjo, K. Changes in serum uric acid have a reciprocal effect on eGFR change: a 10-year follow-up study of community-based screening in Okinawa, Japan. Hypertens Res 36, 650–654 (2013). https://doi.org/10.1038/hr.2013.11
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2013.11
Keywords
This article is cited by
-
Open-label study of long-term administration of dotinurad in Japanese hyperuricemic patients with or without gout
Clinical and Experimental Nephrology (2020)
-
Factors related to suboptimal recovery of renal function after living donor nephrectomy: a retrospective study
BMC Nephrology (2019)
-
Importance of glomerular filtration rate change as surrogate endpoint for the future incidence of end-stage renal disease in general Japanese population: community-based cohort study
Clinical and Experimental Nephrology (2018)
-
Hyperuricemia after orthotopic liver transplantation: divergent associations with progression of renal disease, incident end-stage renal disease, and mortality
BMC Nephrology (2017)
-
Associations between serum uric acid levels and the incidence of nonfatal stroke: a nationwide community-based cohort study
Clinical and Experimental Nephrology (2017)