Abstract
Objective:
Prader–Willi syndrome (PWS) is a genetic neurodevelopmental disorder with several nutritional phases during childhood proceeding from poor feeding, through normal eating without and with obesity, to hyperphagia and life-threatening obesity, with variable ages of onset. We investigated whether differences in appetite hormones may explain the development of abnormal eating behaviour in young children with PWS.
Subjects:
In this cross-sectional study, children with PWS (n=42) and controls (n=9) aged 7 months–5 years were recruited. Mothers were interviewed regarding eating behaviour, and body mass index (BMI) was calculated. Fasting plasma samples were assayed for insulin, leptin, glucose, peptide YY (PYY), ghrelin and pancreatic polypeptide (PP).
Results:
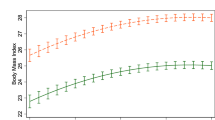
There was no significant relationship between eating behaviour in PWS subjects and the levels of any hormones or insulin resistance, independent of age. Fasting plasma leptin levels were significantly higher (mean±s.d.: 22.6±12.5 vs 1.97±0.79 ng ml−1, P=0.005), and PP levels were significantly lower (22.6±12.5 vs 69.8±43.8 pmol l−1, P<0.001) in the PWS group compared with the controls, and this was independent of age, BMI, insulin resistance or IGF-1 levels. However, there was no significant difference in plasma insulin, insulin resistance or ghrelin levels between groups, though PYY declined more rapidly with age but not BMI in PWS subjects.
Conclusion:
Even under the age of 5 years, PWS is associated with low levels of anorexigenic PP, as in older children and adults. Hyperghrelinaemia or hypoinsulinaemia was not seen in these young children with PWS. Change in these appetite hormones was not associated with the timing of the transition to the characteristic hyperphagic phase. However, abnormal and/or delayed development or sensitivity of the effector pathways of these appetitive hormones (for example, parasympathetic and central nervous system) may interact with low PP levels, and later hyperghrelinaemia or hypoinsulinaemia, to contribute to hyperphagia in PWS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Whittington JE, Holland A . Prader-Willi Syndrome: Development and Manifestations. Cambridge University Press: Cambridge, 2004.
Goldstone AP . Prader-Willi syndrome: advances in its genetics, pathophysiology and treatment. Trends Endocrinol Metab 2004; 15: 12–20.
Goldstone AP, Holland AJ, Hauffa BP, Hokken-Koelega AC, Tauber M . Recommendations for the diagnosis and management of Prader-Willi syndrome. J Clin Endocrinol Metab 2008; 93: 4183–4197.
Cassidy SB, Driscoll DJ . Prader-Willi syndrome. Eur J Hum Genet 2009; 17: 3–13.
Butler JV, Whittington JE, Holland AJ, Mcallister CJ, Goldstone AP . The transition between the phenotypes of Prader-Willi syndrome during infancy and early childhood. Dev Med Child Neurol 2009; 52: E88–E93.
Miller JL, Driscoll DC, Lynn CH, Goldstone AP, Kimonis V, Dykens E et al. Nutritional phases in Prader-Willi syndrome. Am J Med Genet A 2011; 155: 1040–1049.
Butler JV, Whittington JE, Holland AJ, Boer H, Clarke D, Webb T . Prevalence of, and risk factors for, physical Ill-health in people with Prader-Willi syndrome: a population-based study. Dev Med Child Neurol 2002; 44: 248–255.
Butler MG . Management of obesity in Prader-Willi syndrome. Nat Clin Pract Endocrinol Metab 2006; 2: 592–593.
Holland A, Whittington J, Hinton E . The paradox of Prader-Willi syndrome: a genetic model of starvation. Lancet 2003; 362: 989–991.
Goldstone AP . The hypothalamus, hormones, and hunger: alterations in human obesity and illness. Prog Brain Res 2006; 153: 57–73.
Holland AJ, Treasure J, Coskeran P, Dallow J, Milton N, Hillhouse E . Measurement of excessive appetite and metabolic changes in Prader-Willi syndrome. Int J Obes 1993; 17: 527–532.
Zipf WB, Berntson GG . Characteristics of abnormal food-intake patterns in children with Prader-Willi syndrome and study of effects of naloxone. Am J Clin Nutr 1987; 46: 277–281.
Hinton EC, Holland AJ, Gellatly MS, Soni S, Patterson M, Ghatei MA et al. Neural representations of hunger and satiety in Prader-Willi syndrome. Int J Obes 2005; 30: 313–321.
Miller JL, James GA, Goldstone AP, Couch JA, He G, Driscoll DJ et al. Enhanced activation of reward mediating prefrontal regions in response to food stimuli in Prader-Willi syndrome. J Neurol Neurosurg Psychiatry 2007; 78: 615–619.
Holsen LM, Zarcone JR, Brooks WM, Butler MG, Thompson TI, Ahluwalia JS et al. Neural mechanisms underlying hyperphagia in Prader-Willi syndrome. Obesity 2006; 14: 1028–1037.
Swaab DF, Purba JS, Hofman MA . Alterations in the hypothalamic paraventricular nucleus and its oxytocin neurons (putative satiety cells) in Prader-Willi syndrome: a study of five cases. J Clin Endocrinol Metab 1995; 80: 573–579.
Miller JL, Couch JA, Schmalfuss I, He G, Liu Y, Driscoll DJ . Intracranial abnormalities detected by three-dimensional magnetic resonance imaging in Prader-Willi syndrome. Am J Med Genet A 2007; 143: 476–483.
Korbonits M, Goldstone AP, Gueorguiev M, Grossman AB . Ghrelin - a hormone with multiple functions. Front Neuroendocrinol 2004; 25: 27–68.
Field BC, Chaudhri OB, Bloom SR . Bowels control brain: gut hormones and obesity. Nat Rev Endocrinol 2010; 6: 444–453.
Scerif M, Goldstone AP, Korbonits M . Ghrelin in obesity and endocrine diseases. Mol Cell Endocrinol 2011; 340: 15–25.
Zipf WB, O'dorisio TM, Cataland S, Sotos J . Blunted pancreatic polypeptide responses in children with obesity of Prader-Willi syndrome. J Clin Endocrinol Metab 1981; 52: 1264–1266.
Zipf WB, O'dorisio TM, Cataland S, Dixon K . Pancreatic polypeptide responses to protein meal challenges in obese but otherwise normal children and obese children with Prader-Willi syndrome. J Clin Endocrinol Metab 1983; 57: 1074–1080.
Tomita T, Greeley Jr G, Watt L, Doull V, Chance R . Protein meal-stimulated pancreatic polypeptide secretion in Prader-Willi syndrome of adults. Pancreas 1989; 4: 395–400.
Schuster DP, Osei K, Zipf WB . Characterization of alterations in glucose and insulin metabolism in Prader-Willi subjects. Metabolism 1996; 45: 1514–1520.
Butler MG, Carlson MG, Schmidt DE, Feurer ID, Thompson T . Plasma cholecystokinin levels in Prader-Willi syndrome and obese subjects. Am J Med Genet 2000; 95: 67–70.
Cummings DE, Clement K, Purnell JQ, Vaisse C, Foster KE, Frayo RS et al. Elevated plasma ghrelin levels in Prader Willi syndrome. Nat Med 2002; 8: 643–644.
Delparigi A, Tschop M, Heiman ML, Salbe AD, Vozarova B, Sell SM et al. High circulating ghrelin: a potential cause for hyperphagia and obesity in Prader-Willi syndrome. J Clin Endocrinol Metab 2002; 87: 5461–5464.
Bizzarri C, Rigamonti AE, Giannone G, Berardinelli R, Cella SG, Cappa M et al. Maintenance of a normal meal-induced decrease in plasma ghrelin levels in children with Prader-Willi syndrome. Horm Metab Res 2004; 36: 164–169.
Mogul HR, Lee PD, Whitman B, Zipf W, Frey M, Myers SE et al. Preservation of insulin sensitivity and paucity of metabolic syndrome symptoms in Prader Willi syndrome adults: preliminary data from the us multi-center study. Obes Res 2004; 12: 171, Ht-08.
Goldstone AP, Thomas EL, Brynes AE, Bell JD, Frost G, Saeed N et al. Visceral adipose tissue and metabolic complications of obesity are reduced in Prader-Willi syndrome female adults: evidence for novel influences on body fat distribution. J Clin Endocrinol Metab 2001; 86: 4330–4338.
Goldstone AP, Brynes AE, Thomas EL, Bell JD, Frost G, Holland A et al. Resting metabolic rate, plasma leptin concentrations, leptin receptor expression, and adipose tissue measured by whole-body magnetic resonance imaging in women with Prader-Willi syndrome. Am J Clin Nutr 2002; 75: 468–475.
Haqq AM, Farooqi IS, O'rahilly S, Stadler DD, Rosenfeld RG, Pratt KL et al. Serum ghrelin levels are inversely correlated with body mass index, age, and insulin concentrations in normal children and are markedly increased in Prader-Willi syndrome. J Clin Endocrinol Metab 2003; 88: 174–178.
Haqq AM, Stadler DD, Rosenfeld RG, Pratt KL, Weigle DS, Frayo RS et al. Circulating ghrelin levels are suppressed by meals and octreotide therapy in children with Prader-Willi syndrome. J Clin Endocrinol Metab 2003; 88: 3573–3576.
Goldstone AP, Thomas EL, Brynes AE, Castroman G, Edwards R, Ghatei MA et al. Elevated fasting plasma ghrelin in Prader-Willi syndrome adults is not solely explained by their reduced visceral adiposity and insulin resistance. J Clin Endocrinol Metab 2004; 89: 1718–1726.
Goldstone AP . Ghrelin and Other Gastrointestinal Hormones in Prader-Willi Syndrome. Abstracts 5th Prader-Willi Syndrome International Conference: Christchurch, New Zealand, 2004.
Tauber M, Conte AF, Moulin P, Molinas C, Delagnes V, Salles JP . Hyperghrelinemia is a common feature of Prader-Willi syndrome and pituitary stalk interruption: a pathophysiological hypothesis. Horm Res 2004; 62: 49–54.
Paik KH, Jin DK, Song SY, Lee JE, Ko SH, Song SM et al. Correlation between fasting plasma ghrelin levels and age, body mass index (BMI), BMI percentiles, and 24-hour plasma ghrelin profiles in Prader-Willi syndrome. J Clin Endocrinol Metab 2004; 89: 3885–3889.
Goldstone AP, Patterson M, Kalingag N, Ghatei MA, Brynes AE, Bloom SR et al. Fasting and post-prandial hyperghrelinemia in Prader-Willi syndrome is partially explained by hypoinsulinemia, and is not due to peptide YY 3-36 deficiency or seen in hypothalamic obesity due to craniopharyngioma. J Clin Endocrinol Metab 2005; 90: 2681–2690.
Erdie-Lalena CR, Holm VA, Kelly PC, Frayo RS, Cummings DE . Ghrelin levels in young children with Prader-Willi syndrome. J Pediatr 2006; 149: 199–204.
Paik KH, Choe YH, Park WH, Oh YJ, Kim AH, Chu SH et al. Suppression of acylated ghrelin during oral glucose tolerance test is correlated with whole-body insulin sensitivity in children with Prader-Willi syndrome. J Clin Endocrinol Metab 2006; 91: 1876–1881.
Paik KH, Jin DK, Lee KH, Armstrong L, Lee JE, Oh YJ et al. Peptide YY, cholecystokinin, insulin and ghrelin response to meal did not change, but mean serum levels of insulin is reduced in children with Prader-Willi syndrome. J Korean Med Sci 2007; 22: 436–441.
Butler MG, Bittel DC . Plasma obestatin and ghrelin levels in subjects with Prader-Willi syndrome. Am J Med Genet A 2007; 143: 415–421.
Gimenez-Palop O, Gimenez-Perez G, Mauricio D, Gonzalez-Clemente JM, Potau N, Berlanga E et al. A lesser postprandial suppression of plasma ghrelin in Prader-Willi syndrome is associated with low fasting and a blunted postprandial PYY response. Clin Endocrinol (Oxf) 2007; 66: 198–204.
Bizzarri C, Rigamonti AE, Luce A, Cappa M, Cella SG, Berini J et al. Children with Prader-Willi syndrome exhibit more evident meal-induced responses in plasma ghrelin and peptide YY levels than obese and lean children. Eur J Endocrinol 2010; 162: 499–505.
Haqq AM, Muehlbauer M, Svetkey LP, Newgard CB, Purnell JQ, Grambow SC et al. Altered distribution of adiponectin isoforms in children with Prader-Willi syndrome (Pws): association with insulin sensitivity and circulating satiety peptide hormones. Clin Endocrinol (Oxf) 2007; 67: 944–951.
Haqq AM, Grambow SC, Muehlbauer M, Newgard CB, Svetkey LP, Carrel AL et al. Ghrelin concentrations in Prader-Willi syndrome (PWS) infants and children: changes during development. Clin Endocrinol (Oxf) 2008; 69: 911–920.
Feigerlova E, Diene G, Conte-Auriol F, Molinas C, Gennero I, Salles JP et al. Hyperghrelinemia precedes obesity in Prader-Willi syndrome. J Clin Endocrinol Metab 2008; 93: 2800–2805.
Haqq AM, Muehlbauer MJ, Newgard CB, Grambow S, Freemark M . The metabolic phenotype of Prader-Willi syndrome (PWS) in childhood: heightened insulin sensitivity relative to body mass index. J Clin Endocrinol Metab 2011; 96: E225–E232.
Whittington JE, Butler JV, Holland AJ . Changing rates of genetic subtypes of Prader-Willi syndrome in the UK. Eur J Hum Genet 2007; 15: 127–130.
Whittington JE, Butler JV, Holland AJ . Pre-, peri- and postnatal complications in Prader-Willi syndrome in a UK sample. Early Hum Dev 2008; 84: 331–336.
Adrian TE, Bloom SR, Bryant MG, Polak JM, Heitz PH, Barnes AJ . Distribution and release of human pancreatic polypeptide. Gut 1976; 17: 940–944.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Farooqi IS . Monogenic human obesity. Front Horm Res 2008; 36: 1–11.
Michaud JL, Boucher F, Melnyk A, Gauthier F, Goshu E, Levy E et al. Sim1 haploinsufficiency causes hyperphagia, obesity and reduction of the paraventricular nucleus of the hypothalamus. Hum Mol Genet 2001; 10: 1465–1473.
Varela MC, Simoes-Sato AY, Kim CA, Bertola DR, De Castro CI, Koiffmann CP . A new case of interstitial 6q16.2 deletion in a patient with Prader-Willi-like phenotype and investigation of sim1 gene deletion in 87 patients with syndromic obesity. Eur J Med Genet 2006; 49: 298–305.
Berntson GG, Zipf WB, O'dorisio TM, Hoffman JA, Chance RE . Pancreatic polypeptide infusions reduce food intake in Prader-Willi syndrome. Peptides 1993; 14: 497–503.
Stefan M, Simmons RA, Bertera S, Trucco M, Esni F, Drain P et al. Global deficits in development, function, and gene expression in the endocrine pancreas in a deletion mouse model of Prader-Willi syndrome. Am J Physiol Endocrinol Metab 2011; 300: E909–E922.
Eiholzer U, Stutz K, Weinmann C, Torresani T, Molinari L, Prader A . Low insulin, Igf-I and Igfbp-3 levels in children with Prader-Labhart-Willi syndrome. Eur J Paediatrics 1998; 157: 890–893.
Tan TM, Vanderpump M, Khoo B, Patterson M, Ghatei MA, Goldstone AP . Somatostatin infusion lowers plasma ghrelin without reducing appetite in adults with Prader-Willi syndrome. J Clin Endocrinol Metab 2004; 89: 4162–4165.
Eiholzer U, Blum WF, Molinari L . Body fat determined by skinfold measurements is elevated despite underweight in infants With Prader-Labhart-Willi syndrome. J Pediatr 1999; 134: 222–225.
Acknowledgements
Financial support from Baily Thomas Charitable Fund, the Health Foundation, NIHR Collaborations in Leadership for Applied Health Research and Care (CLAHRC) for Cambridgeshire and Peterborough (AJH) and UK Medical Research Council (APG). We thank study participants, PWSA-UK and Addenbrookes Hospital consultants (particularly Miss Allen) for help with recruitment, Nicola Matache (Addenbrookes Hospital, Cambridge), Michael Patterson and Mohammad Ghatei (Section of Investigative Medicine, Imperial College London) for performing assays.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Goldstone, A., Holland, A., Butler, J. et al. Appetite hormones and the transition to hyperphagia in children with Prader-Willi syndrome. Int J Obes 36, 1564–1570 (2012). https://doi.org/10.1038/ijo.2011.274
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2011.274
Keywords
This article is cited by
-
Do patients with Prader–Willi syndrome have favorable glucose metabolism?
Orphanet Journal of Rare Diseases (2022)
-
Prader–Willi Syndrome in Adults: An Update On Nutritional Treatment and Pharmacological Approach
Current Obesity Reports (2022)
-
Serum alpha-melanocyte-stimulating hormone (a-MSH), brain-derived neurotrophic factor (BDNF), and agouti-related protein (AGRP) levels in children with Prader-Willi or Bardet-Biedl syndromes
Journal of Endocrinological Investigation (2022)
-
Obesity in Prader–Willi syndrome: physiopathological mechanisms, nutritional and pharmacological approaches
Journal of Endocrinological Investigation (2021)
-
Mapping the genetic basis of diabetes mellitus in the Australian Burmese cat (Felis catus)
Scientific Reports (2020)