Abstract
Objective:
Roux-en-Y gastric bypass (RYGB) produces more durable glycemic control than sleeve gastrectomy (SG) or intensive medical therapy (IMT). However, the contribution of acylated ghrelin (AG), a gluco-regulatory/appetite hormone, to improve glucose metabolism and body composition in patients with type 2 diabetes (T2D) following RYGB is unknown.
Design:
STAMPEDE (Surgical Treatment and Medication Potentially Eradicate Diabetes Efficiently) was a prospective, randomized controlled trial.
Subjects:
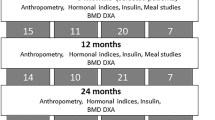
Fifty-three (body mass index: 36±3 kg m−2, age: 49±9 years) poorly controlled patients with T2D (HbA1c (glycated hemoglobin): 9.7±2%) were randomized to IMT, IMT+RYGB or IMT+SG and underwent a mixed-meal tolerance test at baseline, 12, and 24 months for evaluation of AG suppression (postprandial minus fasting) and beta-cell function (oral disposition index; glucose-stimulated insulin secretion × Matsuda index). Total/android body fat (dual-energy X-ray absorptiometry) was also assessed.
Results:
RYGB and SG reduced body fat comparably (15–23 kg) at 12 and 24 months, whereas IMT had no effect. Beta-cell function increased 5.8-fold in RYGB and was greater than IMT at 24 months (P<0.001). However, there was no difference in insulin secretion between SG vs IMT at 24 months (P=0.32). Fasting AG was reduced fourfold following SG (P<0.01) and did not change with RYGB or IMT at 24 months. AG suppression improved more following RYGB than SG or IMT at 24 months (P=0.01 vs SG, P=0.07 vs IMT). At 24 months, AG suppression was associated with increased postprandial glucagon-like peptide-1 (r=−0.32, P<0.02) and decreased android fat (r=0.38; P<0.006).
Conclusions:
Enhanced AG suppression persists for up to 2 years after RYGB, and this effect is associated with decreased android obesity and improved insulin secretion. Together, these findings suggest that AG suppression is partly responsible for the improved glucose control after RYGB surgery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Kahn SE, Hull RL, Utzschneider KM . Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 2006; 444: 840–846.
Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR et al. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement executive summary. Diabetes Care 2010; 33: 2692–2696.
Buchwald H, Oien DM . Metabolic/bariatric surgery Worldwide 2008. Obesity Surg 2009; 19: 1605–1611.
Mingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Leccesi L et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med 2012; 366: 1577–1585.
Schauer PR, Kashyap SR, Wolski K, Brethauer S, Kirwan JP, Pothier CE et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med 2012; 366: 1567–1576.
Peterli R, Steinert RE, Woelnerhanssen B, Peters T, Christoffel Courtin C, Gass M et al. Metabolic and hormonal changes after laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy: a randomized, prospective trial. Obesity Surg 2012; 22: 740–748.
Karamanakos SN, Vagenas K, Kalfarentzos F, Alexandrides TK . Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy: a prospective, double blind study. Ann Surg 2008; 247: 401–407.
Mingrone G, Nolfe G, Gissey GC, Iaconelli A, Leccesi L, Guidone C et al. Circadian rhythms of GIP and GLP1 in glucose-tolerant and in type 2 diabetic patients after biliopancreatic diversion. Diabetologia 2009; 52: 873–881.
Cummings DE, Overduin J, Foster Schubert KE . Gastric bypass for obesity: mechanisms of weight loss and diabetes resolution. J Clin Endocrinol Metab 2004; 89: 2608–2615.
Korner J, Bessler M, Inabnet W, Taveras C, Holst JJ . Exaggerated glucagon-like peptide-1 and blunted glucose-dependent insulinotropic peptide secretion are associated with Roux-en-Y gastric bypass but not adjustable gastric banding. Surg Obesity Relat Dis 2007; 3: 597–601.
Kashyap SR, Daud S, Kelly KR, Gastaldelli A, Win H, Brethauer S et al. Acute effects of gastric bypass versus gastric restrictive surgery on beta-cell function and insulinotropic hormones in severely obese patients with type 2 diabetes. Int J Obes 2010; 34: 462–471.
Thaler JP, Cummings DE . Minireview: hormonal and metabolic mechanisms of diabetes remission after gastrointestinal surgery. Endocrinology 2009; 150: 2518–2525.
Davies JS, Kotokorpi P, Eccles SR, Barnes SK, Tokarczuk PF, Allen SK et al. Ghrelin induces abdominal obesity via GHS-R-dependent lipid retention. Mol Endocrinol 2009; 23: 914–924.
Theander Carrillo C, Wiedmer P, Cettour Rose P, Nogueiras R, Perez Tilve D, Pfluger P et al. Ghrelin action in the brain controls adipocyte metabolism. J Clin Invest 2006; 116: 1983–1993.
Tong J, Prigeon RL, Davis HW, Bidlingmaier M, Kahn SE, Cummings DE et al. Ghrelin suppresses glucose-stimulated insulin secretion and deteriorates glucose tolerance in healthy humans. Diabetes 2010; 59: 2145–2151.
Cummings DE, Weigle D, Frayo RS, Breen P, Ma M, Dellinger EP et al. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med 2002; 346: 1623–1630.
Kashyap SR, Bhatt DL, Wolski K, Wantanabe RM, Abdul-Ghani MA, Abood B et al. Metabolic effects of bariatric surgery in patients with moderate obesity and type 2 diabetes: analysis of a randomized control trial comparing surgery vs. intensive medical treatment. Diabetes Care 2013; 36: 2175–2182.
Patel RT, Shukla AP, Ahn SM, Moreira M, Rubino F . Surgical control of obesity and diabetes: the role of intestinal vs gastric mechanisms in the regulation of body weight and glucose homeostasis. Obesity 2013. e-pub ahead of print 20 March 2013 doi:10.1002/oby.20441.
Kashyap SR, Bhatt DL, Schauer PR . Bariatric surgery vs. advanced practice medical management in the treatment of type 2 diabetes mellitus: rationale and design of the Surgical Therapy And Medications Potentially Eradicate Diabetes Efficiently trial (STAMPEDE). Diabetes Obes Metab 2010; 12: 452–454.
Blatnik M, Soderstrom CI . A practical guide for the stabilization of acylghrelin in human blood collections. Clin Endocrinol (Oxf) 2011; 74: 325–331.
Falken Y, Hellstrom PM, Holst JJ, Naslund E . Changes in glucose homeostasis after Roux-en Y gastric bypass surgery for obesity at day three, two months, and one year after surgery: role of gut peptides. J Clin Endocrinol Metab 2011; 96: 2227–2235.
Vendrell J, Broch M, Vilarrasa N, Molina A, Gomez J, Gutierrez C et al. Resistin, adiponectin, ghrelin, leptin, and proinflammatory cytokines: relationships in obesity. Obes Res 2004; 12: 962–971.
Korner J, Bessler M, Cirilo LJ, Conwell IM, Daud A, Restuccia NL et al. Effects of Roux-en-Y gastric bypass surgery on fasting and postprandial concentrations of plasma ghrelin, peptide YY, and insulin. J Clin Endocrinol Metab 2005; 90: 359–365.
Engstorm BE, Ohrvall M, Sundbom M, Lind L, Karlsson FA . Meal suppression of circulating ghrelin is normalized in obese individuals following gastric bypass surgery. Int J Obes 2007; 31: 476–480.
Rodieux F, Giusti V, D'Alessio DA, Suter M, Tappy L . Effects of gastric bypass and gastricbanding on glucose kinetics and gut hormone release. Obesity 2008; 16: 298–305.
Samat A, Malin SK, Huang H, Schauer PR, Kirwan JP, Kashyap SR . Ghrelin suppression is associated with weight loss and insulin action following gastric bypass surgery at 12 months inobese adults with type 2 diabetes. Diabetes Obes Metab 2013; 15: 963–966.
Barazzoni R, Zanetti M, Nagliati C, Cattin MR, Ferreira C, Giuricin M et al. Gastric bypass does not normalize obesity-related changes in ghrelin profile and leads to higher acylated ghrelin fraction. Obesity 2013; 21: 718–722.
Lee WJ, Chen CY, Chong K, Lee YC, Chen SC, Lee SD . Changes in postprandial gut hormones after metabolic surgery: a comparison of gastric bypass and sleeve gastrectomy. Surg Obes Relat Dis 2011; 7: 683–690.
Tsubone T, Masaki T, Katsuragi I, Tanaka K, Kakuma T, Yoshimatsu H . Ghrelin regulates adiposity in white adipose tissue and UCP1 mRNA expression in brown adipose tissue in mice. Regul Pept 2005; 130: 97–103.
Yu BL, Zhao SP, Hu JR . Cholesterol imbalance in adipocytes: a possible mechanism of adipocytes dysfunction in obesity. Obes Rev 2010; 11: 560–567.
Ariyasu H, Takaya K, Tagami T, Ogawa Y, Hosoda K, Akamizu T et al. Stomach is a major source of circulating ghrelin, and feeding state determines plasma ghrelin-like immunoreactivity levels in humans. J Clin Endocrinol Metab 2001; 86: 4753–4758.
Sondergaard E, Gormsen LC, Nellemann B, Vestergaard ET, Christiansen JS, Nielsen S . Visceral fat mass is a strong predictor of circulating ghrelin levels in premenopausal women. Euro J Endocrinol 2009; 160: 375–379.
Jimenez A, Casamitjana R, Viaplana Masclans J, Lacy A, Vidal J . GLP-1 action and glucose tolerance in subjects with remission of type 2 diabetes mellitus after gastric bypass surgery. Diabetes Care 2013; 36: 2062–2069.
Hagemann D, Holst JJ, Gethmann A, Banasch M, Schmidt W, Meier JJ . Glucagon-like peptide 1 (GLP-1) suppresses ghrelin levels in humans via increased insulin secretion. Regul Pept 2007; 143: 64–68.
Chelikani P, Haver A, Reidelberger R . Ghrelin attenuates the inhibitory effects of glucagon-like peptide-1 and peptide YY(3-36) on food intake and gastric emptying in rats. Diabetes 2006; 55: 3038–3046.
Damdindorj B, Dezaki K, Kurashina T, Sone H, Rita R, Kakei M et al. Exogenous and endogenous ghrelin counteracts GLP-1 action to stimulate cAMP signaling and insulin secretion in islet beta-cells. FEBS Lett 2012; 586: 2555–2562.
Bohdjalian A, Langer FB, Shakeri Leidenmuhler S, Gfrerer L, Ludvik B, Zacherl J et al. Sleeve gastrectomy as sole and definitive bariatric procedure: 5-year results for weight loss and ghrelin. Obes Surg 2010; 20: 535–540.
Gregg EW, Chen H, Wagenknecht LE, Clark JM, Delahanty LM, Bantle J et al. Association of an intensive lifestyle intervention with remission of type 2 diabetes. JAMA 2012; 308: 2489–2496.
Balducci S, Zanuso S, Nicolucci A, De Feo P, Cavallo S, Cardelli P et al. Effect of an intensive exercise intervention strategy on modifiable cardiovascular risk factors in subjects with type 2 diabetes mellitus: a randomized controlled trial: the Italian Diabetes and Exercise Study (IDES). Arch Intern Med 2010; 170: 1794–1803.
Malin SK, Gerber R, Chipkin SR, Braun B . Independent and combined effects of exercise training and metformin on insulin sensitivity in individuals with prediabetes. Diabetes Care 2012; 35: 1–6.
Solomon TPJ, Malin SK, Karstoft K, Haus JM, Kirwan JP . Hyperglycemia blunts the therapeutic effect of exercise on glycemic control in type 2 diabetes. JAMA 2013; 173: 1834–1836.
Dirksen C, Jorgensen NB, Bojsen Moller KN, Jacobsen SH, Hansen DL, Worm D et al. Mechanisms of improved glycaemic control after Roux-en-Y gastric bypass. Diabetologia 2012; 55: 1890–1901.
Hagobian TA, Braun B . Physical activity and hormonal regulation of appetite: sex differences and weight control. Exerc Sport Sci Rev 2010; 38: 25–30.
Acknowledgements
SKM, KW and SRK share responsibility for the integrity of analysis. All authors contributed to data collection and organization. Sarah Neale from the Cleveland Clinic Preventive Research Lab performed blood analysis. The Cleveland Clinic Coordinating Center for Clinical Research provided the database and statistical analysis. SKM wrote the manuscript and all authors provided edits. We thank the CRU and bariatric surgery nursing staff for their outstanding assistance and all the participants for their efforts. This research was supported by Ethicon endo-surgery EESIIS 19900 (PRS), American Diabetes Association clinical translational award 1-11-26 CT (SRK), NIH RO1-DK089547 (PRS, SRK, JPK), and the National Institutes of Health National Center for Research Resources, 1UL1RR024989, Cleveland, OH, USA. SKM was supported by a T32 DK007319 Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
SRK obtained research grants from Ethicon Endo-surgery, National Institutes of Health and American Diabetes Association. DLB—Advisory Board: Medscape Cardiology; Board of Directors: Boston VA Research Institute, Society of Chest Pain Centers; Chair: American Heart Association Get With The Guidelines Science Subcommittee; Honoraria: American College of Cardiology (Editor, Clinical Trials, Cardiosource), Duke Clinical Research Institute (clinical trial steering committees), Slack Publications (Chief Medical Editor, Cardiology Today Intervention) and WebMD (CME steering committees); research grants: Amarin, AstraZeneca, Bristol-Myers Squibb, Eisai, Ethicon, Medtronic, Sanofi Aventis and The Medicines Company; unfunded research: PLx Pharma and Takeda. PRS obtained research grants from Ethicon Endo-surgery, National Institutes of Health and Bard-Davol; educational grants from Stryker Endoscopy, Gore, Baxter, Covidien and Allergan: honoraria from Ethicon Endo-surgery as scientific advisory board member, consultant and speaker. He has been a consultant/advisory board member for RemedyMD, StrykerEndoscopy, Bard-Davol, Gore, Barosense, Surgiquest and Carefusion. SAB receives honoraria from Ethicon Endo-Surgery as scientific advisory board member, consultant and speaker and honoraria from Covidien for speaking. SN has consulted with Orexigen and Vivus. JPK receives grant funding from the National Institutes of Health, Nestle Inc. and ScottCare. All the other authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Malin, S., Samat, A., Wolski, K. et al. Improved acylated ghrelin suppression at 2 years in obese patients with type 2 diabetes: effects of bariatric surgery vs standard medical therapy. Int J Obes 38, 364–370 (2014). https://doi.org/10.1038/ijo.2013.196
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2013.196
Keywords
This article is cited by
-
The role of the gastric fundus in glycemic control
Hormones (2023)
-
Gastric ghrelin cells in obese patients are hyperactive
International Journal of Obesity (2021)
-
Effect of sleeve gastrectomy, Roux-en-Y gastric bypass, and ileal transposition on myocardial ischaemia–reperfusion injury in non-obese non-diabetic rats
Scientific Reports (2021)
-
Physiologic Mechanisms of Type II Diabetes Mellitus Remission Following Bariatric Surgery: a Meta-analysis and Clinical Implications
Journal of Gastrointestinal Surgery (2020)
-
Gastric Bypass Improves Obesity and Glucose Tolerance Independent of Gastric Pouch Size
Obesity Surgery (2020)