Abstract
Objective:
To investigate whether antibiotic exposure during the first year of life is associated with increased childhood body mass index (BMI).
Design:
Secondary analysis from a multi-centre, multi-country, cross-sectional study (The International Study of Asthma and Allergies in Childhood Phase Three).
Subjects:
A total of 74 946 children from 31 centres in 18 countries contributed data on antibiotic use in the first 12 months of life and current BMI.
Methods:
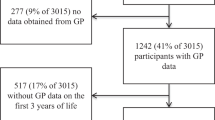
Parents/guardians of children aged 5–8 years completed questionnaires that included questions about their children’s current height and weight, and whether in the child’s first 12 months of life, they had received any antibiotics, paracetamol, were breastfed or the mother/female guardian smoked cigarettes, and whether the child had wheezed in the past 12 months. A general linear mixed model was used to determine the association of antibiotic exposure with BMI, adjusting for age, sex, centre, BMI measurement type (self-reported or measured), maternal smoking, breastfeeding, paracetamol use, gross national income and current wheeze.
Results:
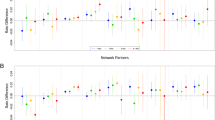
There was a significant interaction between sex and early-life antibiotic exposure. Early-life antibiotic exposure was associated with increased childhood BMI in boys (+0.107 kg m−2, P<0.0001), but not in girls (−0.008 kg m−2, P=0.75) after controlling for age, centre and BMI measurement type. The association remained in boys (+0.104 kg m−2, P<0.0007), after adjustment for maternal smoking, breastfeeding, paracetamol use and current wheeze. There was no interaction between age, maternal smoking, breastfeeding, paracetamol use, gross national income and current wheeze in the association between early antibiotic exposure and BMI.
Conclusions:
Exposure to antibiotics during the first 12 months of life is associated with a small increase in BMI in boys aged 5–8 years in this large international cross-sectional survey. By inference this provides additional support for the importance of gut microbiota in modulating the risk of obesity, with a sex-specific effect.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet 2011; 377: 557–567.
Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M . Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011; 378: 815–825.
Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB . Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med 2011; 364: 2392–2404.
Speliotes EK, Willer CJ, Berndt SI, Monda KL, Thorleifsson G, Jackson AU et al. Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat Genet 2010; 42: 937–948.
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI . An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 2006; 444: 1027–1031.
Backhed F, Ding H, Wang T, Hooper LV, Koh GY, Nagy A et al. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci USA 2004; 101: 15718–15723.
Koenig JE, Spor A, Scalfone N, Fricker AD, Stombaugh J, Knight R et al. Succession of microbial consortia in the developing infant gut microbiome. Proc Natl Acad Sci USA 2011; 108 (Suppl 1): 4578–4585.
Cho I, Yamanishi S, Cox L, Methe BA, Zavadil J, Li K et al. Antibiotics in early life alter the murine colonic microbiome and adiposity. Nature 2012; 488: 621–626.
Trasande L, Blustein J, Liu M, Corwin E, Cox LM, Blaser MJ . Infant antibiotic exposures and early-life body mass. Int J Obes 2013; 37: 16–23.
Ajslev TA, Andersen CS, Gamborg M, Sorensen TI, Jess T . Childhood overweight after establishment of the gut microbiota: the role of delivery mode, pre-pregnancy weight and early administration of antibiotics. Int J Obes 2011; 35: 522–529.
Butaye P, Devriese LA, Haesebrouck F . Antimicrobial growth promoters used in animal feed: effects of less well known antibiotics on gram-positive bacteria. Clin Microbiol Rev 2003; 16: 175–188.
Jukes TH . Antibiotics in animal feeds. N Engl J Med 1970; 282: 49–50.
Baumann CA . Growth-promoting effects of antibiotics. Am J Gastroenterol 1955; 24: 513–515.
Trehan I, Goldbach HS, LaGrone LN, Meuli GJ, Wang RJ, Maleta KM et al. Antibiotics as part of the management of severe acute malnutrition. N Engl J Med 2013; 368: 425–435.
Smith MI, Yatsunenko T, Manary MJ, Trehan I, Mkakosya R, Cheng J et al. Gut microbiomes of Malawian twin pairs discordant for kwashiorkor. Science 2013; 339: 548–554.
De Filippo C, Cavalieri D, Di Paola M, Ramazzotti M, Poullet JB, Massart S et al. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc Natl Acad Sci USA 2010; 107: 14691–14696.
Strachan DP, Cook DG . Health effects of passive smoking. 1. Parental smoking and lower respiratory illness in infancy and early childhood. Thorax 1997; 52: 905–914.
Chantry CJ, Howard CR, Auinger P . Full breastfeeding duration and associated decrease in respiratory tract infection in US children. Pediatrics 2006; 117: 425–432.
Foliaki S, Pearce N, Bjorksten B, Mallol J, Montefort S, von Mutius E . Antibiotic use in infancy and symptoms of asthma, rhinoconjunctivitis, and eczema in children 6 and 7 years old: International Study of Asthma and Allergies in Childhood Phase III. J Allergy Clin Immunol 2009; 124: 982–989.
Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F et al. International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir J 1995; 8: 483–491.
Ellwood P, Williams H, Ait-Khaled N, Bjorksten B, Robertson C . Translation of questions: the International Study of Asthma and Allergies in Childhood (ISAAC) experience. Int J Tuberc Lung Dis 2009; 13: 1174–1182.
Lai CK, Beasley R, Crane J, Foliaki S, Shah J, Weiland S . Global variation in the prevalence and severity of asthma symptoms: phase three of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax 2009; 64: 476–483.
Thuny F, Richet H, Casalta JP, Angelakis E, Habib G, Raoult D . Vancomycin treatment of infective endocarditis is linked with recently acquired obesity. PLoS One 2010; 5: e9074.
Miles RD, Butcher GD, Henry PR, Littell RC . Effect of antibiotic growth promoters on broiler performance, intestinal growth parameters, and quantitative morphology. Poult Sci 2006; 85: 476–485.
Feighner SD, Dashkevicz MP . Subtherapeutic levels of antibiotics in poultry feeds and their effects on weight gain, feed efficiency, and bacterial cholyltaurine hydrolase activity. Appl Environ Microbiol 1987; 53: 331–336.
Hernandez E, Bargiela R, Diez MS, Friedrichs A, Perez-Cobas AE, Gosalbes MJ et al. Functional consequences of microbial shifts in the human gastrointestinal tract linked to antibiotic treatment and obesity. Gut Microbes 2013; 4: 306–315.
Gosalbes MJ, Llop S, Valles Y, Moya A, Ballester F, Francino MP . Meconium microbiota types dominated by lactic acid or enteric bacteria are differentially associated with maternal eczema and respiratory problems in infants. Clin Exp Allergy 2013; 43: 198–211.
Vrieze A, Holleman F, Zoetendal EG, de Vos WM, Hoekstra JB, Nieuwdorp M . The environment within: how gut microbiota may influence metabolism and body composition. Diabetologia 2010; 53: 606–613.
Palmer C, Bik EM, DiGiulio DB, Relman DA, Brown PO . Development of the human infant intestinal microbiota. PLoS Biol 2007; 5: e177.
Turnbaugh PJ, Hamady M, Yatsunenko T, Cantarel BL, Duncan A, Ley RE et al. A core gut microbiome in obese and lean twins. Nature 2009; 457: 480–484.
Salminen S, Gibson GR, McCartney AL, Isolauri E . Influence of mode of delivery on gut microbiota composition in seven year old children. Gut 2004; 53: 1388–1389.
Orrhage K, Nord CE . Factors controlling the bacterial colonization of the intestine in breastfed infants. Acta Paediatr Suppl 1999; 88: 47–57.
Phillips CI . Risk of systemic toxicity from topical ophthalmic chloramphenicol. Scott Med J 2008; 53: 54–55.
Acknowledgements
EA Mitchell and I Braithwaite are supported in part by Cure Kids. The authors would like to thank ISAAC Phase Three Principal Investigators and Regional and National Coordinators as listed.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Appendix
Appendix
ISAAC Steering Committee: N Aït-Khaled* (International Union Against Tuberculosis and Lung Diseases, Paris, France); HR Anderson (Division of Community Health Sciences, St Georges, University of London, London, UK); MI Asher (Department of Paediatrics: Child and Youth Health, Faculty of Medical and Health Sciences, The University of Auckland, New Zealand); R Beasley* (Medical Research Institute of New Zealand, Wellington, New Zealand); B Björkstén* (Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden); B Brunekreef (Institute of Risk Assessment Science, Universiteit Utrecht, Netherlands); J Crane (Wellington Asthma Research Group, Wellington School of Medicine, New Zealand); P Ellwood (Department of Paediatrics: Child and Youth Health, Faculty of Medical and Health Sciences, The University of Auckland, New Zealand); C Flohr (Department of Paediatric Allergy and Dermatology, St Johns Institute of Dermatology, St Thomas’ Hospital, London, UK); S Foliaki* (Centre for Public Health Research, Massey University, Wellington, New Zealand); F Forastiere (Department of Epidemiology, Local Health authority Rome, Italy); L García-Marcos (Respiratory Medicine and Allergy Units,‘Virgen de la Arrixaca’ University Children’s Hospital, University of Murcia, Spain); U Keil* (Institut für Epidemiologie und Sozialmedizin, Universität Münster, Germany); CKW Lai* (Department of Medicine and Therapeutics, The Chinese University of Hong Kong, SAR China); J Mallol* (Department of Paediatric Respiratory Medicine, University of Santiago de Chile, Chile); EA Mitchell (Department of Paediatrics: Child and Youth Health, Faculty of Medical and Health Sciences, The University of Auckland, New Zealand); S Montefort* (Department of Medicine, University of Malta, Malta), J Odhiambo* (Centre Respiratory Diseases Research Unit, Kenya Medical Research Institute, Nairobi, Kenya); N Pearce (Department of Medical Statistics, Faculty Epidemiology and Public Health, London School of Hygiene and Tropical Medicine, London, UK); CF Robertson (Murdoch Children’s Research Institute, Melbourne, Australia); AW Stewart (Population Health, Faculty of Medical and Health Sciences, The University of Auckland, New Zealand); D Strachan (Division of Community Health Sciences, St Georges, University of London, London, UK); E von Mutius (Dr von Haunerschen Kinderklinik de Universität München, Germany); SK Weiland† (Institute of Epidemiology, University of Ulm, Germany); G Weinmayr (Institute of Epidemiology, University of Ulm, Germany); H Williams (Centre for Evidence Based Dermatology, Queen’s Medical Centre, University Hospital, Nottingham, UK); G Wong (Department of Paediatrics, Prince of Wales Hospital, Hong Kong, SAR China). *Regional Coordinators; †Deceased.
ISAAC International Data Centre: MI Asher, TO Clayton, E Ellwood, P Ellwood, EA Mitchell, Department of Paediatrics: Child and Youth Health, and AW Stewart, School of Population Health, Faculty of Medical and Health Sciences, The University of Auckland, New Zealand.
ISAAC Principal Investigators: Belgium: J Weyler (Antwerp); Estonia: M-A Riikjärv* (Tallinn); Hungary: G Zsigmond* (Svábhegy); India: SN Mantri (Mumbai (29)); Indonesia: CB Kartasasmita (Bandung); Japan: H Odajima (Fukuoka); Lithuania: J Kudzyte* (Kaunas); Mexico: M Barragán-Meijueiro (Ciudad de México (3)), BE Del-Río-Navarro (Ciudad de México (1)), FJ Linares-Zapién (Toluca); Nigeria: BO Onadeko (Ibadan); Poland: A Brêborowicz (Poznan), G Lis* (Kraków); Portugal: C Nunes (Portimao); South Korea: H-B Lee* (Provincial Korea, Seoul); Spain: RM Busquets (Barcelona), I Carvajal-Urueña (Asturias), G García-Hernández (Madrid), L García-Marcos* (Cartagena), C González Díaz (Bilbao), A López-Silvarrey Varela (A Coruña), MM Morales-Suárez-Varela (Valencia); Sultanate of Oman: O Al-Rawas* (Al-Khod); Syrian Arab Republic: S Mohammad* (Tartous); Y Mohammad (Lattakia); Taiwan: J-L Huang* (Taipei); C-C Kao (Taoyuan); Thailand: M Trakultivakorn (Chiang Mai); P Vichyanond (Bangkok)*; Uruguay: MC Lapides (Paysandú). *National Coordinator.
ISAAC Phase Three National Coordinators not identified above: India: J Shah; Indonesia: K Baratawidjaja; Japan: S Nishima; Mexico: M Baeza-Bacab; Portugal: JE Rosado Pinto; Uruguay: D Holgado.
Rights and permissions
About this article
Cite this article
Murphy, R., Stewart, A., Braithwaite, I. et al. Antibiotic treatment during infancy and increased body mass index in boys: an international cross-sectional study. Int J Obes 38, 1115–1119 (2014). https://doi.org/10.1038/ijo.2013.218
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2013.218
Keywords
This article is cited by
-
Early-life antibiotic exposure increases the risk of childhood overweight and obesity in relation to dysbiosis of gut microbiota: a birth cohort study
Annals of Clinical Microbiology and Antimicrobials (2022)
-
Early childhood infections and body mass index in adolescence
International Journal of Obesity (2021)
-
Infants exposed to antibiotics after birth have altered recognition memory responses at one month of age
Pediatric Research (2021)
-
Do Antibiotics Cause Obesity Through Long-term Alterations in the Gut Microbiome? A Review of Current Evidence
Current Obesity Reports (2021)
-
Body mass index and potential correlates among elementary school children in Jordan
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2021)