Abstract
Objectives:
To assess how outcomes associated with participation in a family-based weight management intervention (MEND 7–13, Mind, Exercise, Nutrition..Do it!) for childhood overweight or obesity implemented at scale in the community vary by child, family, neighbourhood and MEND programme characteristics.
Methods/Subjects:
Intervention evaluation using prospective service level data. Families (N=21 132) with overweight children are referred, or self-refer, to MEND. Families (participating child and one parent/carer) attend two sessions/week for 10 weeks (N=13 998; N=9563 with complete data from 1788 programmes across England). Sessions address diet and physical activity through education, skills training and motivational enhancement. MEND was shown to be effective in obese children in a randomised controlled trial (RCT). Outcomes were mean change in body mass index (BMI), age- and sex-standardised BMI (zBMI), self-esteem (Rosenberg scale) and psychological distress (Strengths and Difficulties Questionnaire) after the 10-week programme. Relationships between the outcome and covariates were tested in multilevel models adjusted for the outcome at baseline.
Results:
After adjustment for covariates, BMI reduced by mean 0.76 kg m−2 (s.e.=0.021, P<0.0001), zBMI reduced by mean 0.18 (s.e.=0.0038, P<0.0001), self-esteem score increased by 3.53 U (s.e.=0.13, P<0.0001) and psychological distress score decreased by 2.65 U (s.e.=0.31, P<0.0001). Change in outcomes varied by participant, family, neighbourhood and programme factors. Generally, outcomes improved less among children from less advantaged backgrounds and in Asian compared with white children. BMI reduction under service conditions was slightly but not statistically significantly less than in the earlier RCT.
Conclusions:
The MEND intervention, when delivered at scale, is associated with improved BMI and psychosocial outcomes on average, but may work less well for some groups of children, and so has the potential to widen inequalities in these outcomes. Such public health interventions should be implemented to achieve sustained impact for all groups.
Similar content being viewed by others
Introduction
Childhood overweight (including obesity) is prevalent in many countries1 and associated with poorer physical and psychosocial health across the life course.2,3 Furthermore, overweight is not distributed evenly across the population and varies by ethnicity, socioeconomic circumstances, gender and age.4,5 The high prevalence and associated burden of childhood overweight necessitates treatment as well as prevention.
A recent Cochrane review and meta-analysis of family-based interventions targeting overweight or obese children concluded that such interventions may deliver ‘clinically relevant’ reductions in body mass index (BMI).6 However, most studies in this review were based on small, homogeneous samples and restricted research settings. This raises concerns about generalisability across all population groups (for example, low socioeconomic circumstances and minority ethnic groups) and implementation contexts, leaving the questions of ‘what works for whom and in what circumstances?’ largely unanswered.6 This is important because interventions have the potential to maintain, reduce or generate health inequalities.7
Weight management interventions for children have been implemented widely across England,8 but there is little information about their performance in service settings. Adoption and implementation of these interventions at scale might be associated with loss of effectiveness.9 In addition, obesogenic environments implicated in the aetiology and maintenance of overweight10 may moderate the effects of interventions,11 but this has been little studied. We address these gaps using observational data from the MEND (Mind, Exercise, Nutrition..Do it!) 7-13 programme, a family-based community intervention implemented at scale under service conditions. We assess whether the biological and psychosocial outcomes associated with participation in the intervention differ by participant, family, programme and neighbourhood characteristics. We also compare changes in BMI observed under service conditions with those observed under research conditions.
Materials and methods
MEND 7–13 is a multi-component family-based community intervention that aims to support families of overweight or obese children to adopt and sustain healthier lifestyles. The intervention addresses diet and physical activity through education, skills training and motivational enhancement. Because of the importance of family involvement for behaviour change, the intervention requires a parent or carer to attend all 20 sessions (over 10 weeks). The MEND 7–13 intervention was developed to be delivered in community settings such as schools or leisure centres12 and delivered by a wide range of health, physical activity and social care professionals. Children are eligible if they are between 7 and 13 years old and overweight or obese (hereafter referred to as overweight, defined as exceeding the 91st centile of the UK 1990 BMI reference). MEND 7–13 was demonstrated in a randomised controlled trial (RCT) to be effective in reducing BMI of obese children at 6 months from baseline.12
Between 2007 and 2010, the MEND 7–13 intervention was implemented on a large scale, with MEND programmes (hereafter ‘programmes’) rolled out across all regions of England. The intervention was delivered by local community-based ‘delivery partner’ organisations. Intervention content and training were provided to delivery partners by MEND Central, a social enterprise.
Delivery partners recorded attendance of participants at each session, and measured height and weight to the nearest 0.1 cm and 0.1 kg using electronic scales following standardised procedures.
Self-esteem was reported by participants on a modified Rosenberg Self-Esteem scale.13 Designed for adolescents, the 10 scale items13 were modified to suit the younger age group (for example, wording such as ‘satisfied’ was clarified with ‘happy’ in brackets). Responses were on a four-point agree–disagree scale (coding in brackets); a lot like me (0), a bit like me (1), not like me (2) and not at all like me (3).
Participant psychological distress was reported by parents on the Strengths and Difficulties questionnaire (SDQ).14 The score comprises 25 items making up five subscales: peer problems, conduct, hyperactivity, anxiety and pro-social behaviour.
Parents also reported the participant’s ethnicity (white, Asian, black or other) and family socioeconomic circumstances including: family structure (lone parent/carer or couple parents/carers); housing tenure (owner occupied, social rented or private rented); and employment status of the ‘primary earner’ (employed or unemployed).
Delivery partners recorded data in an online database collated by MEND Central. For this study, a copy of the database for the period January 2007 to December 2010 was transferred to UCL Institute of Child Health (ICH) for analysis. The UCL Ethics Committee granted approval for the study in October 2010 (REF: 2677/002).
Height and weight data were cleaned to remove implausible values (those exceeding 7 s.d. from the mean and further outliers identified graphically). We calculated BMI (weight height−2) and its derived z-score (zBMI), standardised for age and sex using the UK 1990 BMI growth reference.15,16 Self-esteem items were coded and summed as recommended,13 a high value indicating high self-esteem (score range=0–30). Total psychological distress was calculated following authors’ guidelines by summing twenty items (the pro-social subscale is not included); a high value indicated high psychological distress (score range =0–40).14
For our analyses, outcomes were change in BMI, zBMI, self-esteem and SDQ, calculated as baseline (first session of the programme) subtracted from follow-up (penultimate (19th) session). Therefore, negative values for change indicated a fall in BMI and zBMI; a fall in self-esteem (Rosenberg self-esteem); and a fall in psychological distress (SDQ).
Participants’ residential postcodes were assigned Lower Super Output Area (LSOA) codes, representing small areas with a mean population of 1500 across England. LSOA codes were then used to attach a measure of neighbourhood deprivation (deciles of the Income Deprivation Affecting Children Index (IDACI) 2007),17 urban/rural status (urban, suburban or rural),18 the density of local fast food outlets per LSOA19 and the built environment (based on factor analysis of the percentage of the LSOA made up of roads and green space).20 We counted how many children attended each programme at baseline (hereafter referred to as ‘programme group size’) and the number of programmes that a local programme manager had managed as at the start of each programme. Approximately 80% of measured heights were rounded to whole or half centimetres. We derived a variable indicating if more than 20% of the height measures for a programme were rounded and included this in models to adjust for possible effects of data quality. We also derived a similar measure for weight rounding, where values were rounded to the nearest 0.5 kg. We categorised those attending fewer than 25% of sessions as non-completers, 25–75% as partial completers and more than 75% as completers.
Data were imputed for ethnicity (33% missing), family structure (36%), housing tenure (35%), employment status (63%) and percentage of sessions attended (42%). A multilevel (participants nested in programmes) multiple imputation model (N=13 998) was used to adjust for between-programme variation in missingness in MEND 7–13 programmes. The model assumed that data were missing at random—that missingness on variables was associated with other variables included in the multiple imputation model. Ten imputed data sets were produced and analysis results were combined using Rubin’s rules.21 We followed the guidelines of Sterne et al.22 for the analysis and reporting of missing data and multiple imputation (available on request). To test whether our findings were influenced by using imputed data, we also conducted sensitivity analyses, including analysis using complete case data with and without the variable describing parental employment status, as missingness was relatively high for this variable (data provided in Supplementary Information).
We also used unpublished data from participants in the intervention arm (N=47) of the RCT of MEND 7–1312 to compare change in BMI under trial and service conditions. Height and weight were measured in the first and penultimate sessions of the trial as in the service data. Age, sex, baseline BMI, ethnicity and housing tenure were also measured.
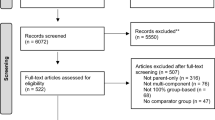
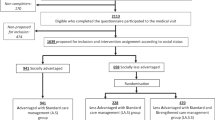
Following the Sterne guidelines,22 analysis outcomes were included in the multiple imputation model where they were missing to ensure that covariates were imputed correctly. However, analysis data sets excluded cases where outcomes were not completely observed at both baseline and follow-up. Sample sizes of the four data sets for analysis of change in BMI, zBMI, self-esteem and SDQ, respectively, are given in Figure 1.
Four sets of two-stage analyses were conducted, one for each outcome. In the first stage, relationships between the outcome and each covariate were tested in multilevel models adjusted for the outcome measured at baseline (‘baseline-adjusted’ models). If the relationship between the covariate and the outcome was statistically significant, the covariate was carried forward to a multilevel multivariable model. The intercept of the multivariable model describes the mean change in the outcome for a given ‘reference group’, which for categorical variables was the largest group, whereas for continuous variables were grand mean centred (allowing the intercept of the model to be interpreted as the mean change). Coefficients in the model describe the amount and direction of change per unit change in the covariates, relative to the reference group.
The random intercept terms estimate variations in outcomes between participants and between programmes. Random slopes were also assessed for age, sex and ethnicity to examine whether the random intercept varied by those factors. A priori-specified interaction terms were also tested for: each outcome at baseline and age, sex and ethnicity, for lone parent family status and the built environment, and for age and sex. Models with random slopes or interaction terms were judged an improvement on models with no additional terms if the Bayesian Information Criterion was more than four points smaller.23
Change in BMI in the service data was also compared with the RCT data, with the service data for this analysis being restricted to obese children to match the RCT. This multilevel model was based on complete case data, adjusted for covariates measured in both data sets (age, sex, ethnicity and housing tenure), to account for potential differences in sample composition.
The multilevel multiple imputation model was estimated using REALCOM-IMPUTE.24 All analyses were conducted using Stata version 12.1 software,25 and multilevel models were fitted in MLwiN 26 using the Stata programme runmlwin.27 Statistical significance was set at the 5% level.
Results
Families (21 132) were referred to the intervention, of which 18 289 had complete data for age, sex and residential postcode (Figure 1). Of these, 13 998 attended a MEND 7–13 programme, 9563 had complete data for change in BMI and zBMI (‘BMI sample’), 5078 had complete data for change in self-esteem (‘self-esteem sample’) and 8127 had complete data for change in SDQ (‘SDQ sample’).
Descriptive statistics (Table 1) were estimated using the BMI sample. As statistics were similar for the self-esteem and SDQ samples, they are not reported here (available on request). Most participants were obese rather than overweight, exceeding the 98th UK 1990 centile. The average age of participants was 10, there were more girls than boys and most children were white. Two-thirds of parents were couples, over half were owner occupiers and three-quarters of households had an employed primary earner. Compared with all LSOAs in England, families lived in LSOAs that were: more income deprived (England mean IDACI 2007=0.21); more likely to be urban (England urban LSOAs=80.6%); and more built up (England built environment score mean=0); but similar in terms of fast food outlet density (England 5+ outlets per LSOA=8%). The mean number of programmes managed previously by programme managers was six programmes, while mean programme group size was nine participants. Three-quarters completed >75% of sessions. Most programmes rounded 20% or more of height measures, whereas just over half rounded 20% or more of weight.
The density of local fast food outlets per LSOA and height/weight rounding variables were not associated with change in BMI and zBMI after adjustment for baseline values (data not shown). In addition, sex and the number of programmes per programme manager were not associated with change in zBMI. Other covariates were statistically significant and retained for multivariable models. A priori-specified interaction terms and random slopes did not improve fit and so these parameters were not retained in the BMI and zBMI models.
Change in self-esteem and SDQ were not associated with age, family structure, housing tenure, urban/rural status, programme group size or weight rounding after adjustment for baseline values. Change in self-esteem was also not associated with the built environment, sex or height rounding, whereas change in SDQ was also not associated with employment status (data not shown). Other covariates were statistically significant and retained for multivariable models as was a random slope for parental employment status in the SDQ model.
In the multivariable model, BMI in the reference group fell on average by 0.76 kg m−2 (Table 2, model 1). In absolute terms, mean BMI fell in all subgroups. Relative to the reference group, BMI fell more for children who were male and with higher baseline BMI; and less for those who were older, from Asian or Black ethnic groups (compared with white groups), living with unemployed (rather than employed) primary earners, living in more deprived neighbourhoods, participating in larger programme groups and partial- and non-completers rather than completers. In the multivariable model, zBMI fell by 0.18 U (Table 2, model 2). Results were similar to those for change in BMI, except that zBMI fell less for children with a higher baseline zBMI.
Self-esteem rose on average by 3.53, approximately half a s.d. of baseline self-esteem (Table 3, model 1), and increased across all subgroups. In relative terms, self-esteem increased less for children with higher baseline self-esteem, for children from Asian ethnic groups versus white children and for partial completers versus completers. SDQ fell on average by 2.65, a third of a s.d. of baseline SDQ (Table 3, model 2), and fell across all subgroups. In relative terms, SDQ reduced more for children with higher baseline SDQ at baseline, for Black compared with white children and those attending programmes with rounded height data; and less for boys, children living in more income-deprived neighbourhoods, where the programme manager had delivered more programmes, non-completers and partial completers rather than completers.
Sensitivity analyses showed that, in general, the direction and order of magnitude of coefficients that were significant in the models estimated using imputed data were similar in those estimated using complete case data (see Supplementary Information for data). However, the material loss of power led to some coefficients being estimated as non-significant in the complete case analyses.
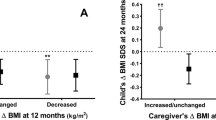
The reduction in BMI for 8–12 year old obese children was 0.79 kg m−2 (95% CI (confidence interval)=0.74, 0.84) in the service data compared with 1.04 kg m−2 (95% CI=0.79, 1.29) in the RCT (adjusted for baseline BMI, age, sex, ethnicity and housing tenure). This difference was not statistically significant.
Discussion
We found that a family-based community intervention for childhood overweight or obesity, when implemented at scale and under service conditions, was associated with improvements in BMI and in psychosocial outcomes. The reduction in BMI under service conditions was slightly but not statistically significantly less than that observed in the RCT of the same intervention. Although previous research has shown that family-based interventions for child overweight are associated with changes in adiposity6 and psychosocial28 outcomes when tested under trial conditions, to our knowledge this is the first study to show that such interventions implemented at scale and under service conditions might also be associated with changes in these outcomes.
Our results also showed that all population subgroups improved on average for all outcomes, but that improvements varied by participant, family, programme and neighbourhood factors. For example, BMI fell more in children with higher baseline BMI, or who were younger, male, white, from families with an employed primary earner or who lived in less deprived areas. BMI also fell more if the child attended more programme sessions and if the programme group was relatively small, suggesting a ‘dose’ effect. Increase in self-esteem was less for children with high baseline self-esteem, Asian children and partial completers. SDQ fell more in children with high baseline SDQ, Black compared with white children and for participants attending programmes where height data were rounded. SDQ reductions were smaller for boys, children living in more deprived neighbourhoods, children participating in programmes where the programme manager had delivered more programmes, non-completers and partial completers.
Our findings therefore show that the intervention, although benefiting all groups to some extent, may also have the potential to widen existing ethnic4 and socioeconomic5 inequalities in childhood overweight and psychosocial outcomes. Such findings may provide the potential for developing programmes such as MEND (for example, by modifying content, training and implementation) to make them more successful for groups who currently respond less well to the intervention.
Although an obesogenic environment is thought to promote the development and maintenance of childhood overweight,29 little work has assessed whether weight management interventions are moderated by features of the wider environment. We found that the outcomes associated with the MEND intervention did not vary with urban/rural characteristics or indicators of the food and built environment. However, measures of area deprivation did appear to moderate changes in BMI and SDQ associated with the intervention, independent of individual socioeconomic circumstances, and this may be capturing unmeasured environmental characteristics that impair successful weight management.
This analysis was based on a large individual-level data set collected under service conditions across all regions of England. It allowed us to estimate with adequate statistical power how outcomes of the MEND intervention varied by participant, family, neighbourhood and programme characteristics, estimates that would be underpowered in most research studies. However, in the absence of controls, such associations cannot be equated with effectiveness. We were able to compare the size of change in BMI in the service data with that observed in the RCT, and they were similar, but we had limited power to assess differences between them (there were only 47 children in the intervention arm of the RCT12). The data we analysed were collected for service provision and not for research. We used a range of techniques for improving data quality, including algorithms for data cleaning, and multiple imputation for missing data. These techniques were aimed at maximising the value of the observed data and minimising bias. We fitted models using imputation and complete case approaches and found that, other than the differences in statistical significance that are to be expected given the greater power of imputation models, findings were similar. Nevertheless, some bias may still be present.
There is little research on what happens once interventions found to be effective in a research setting are implemented in practice at scale.30 We demonstrate here that the MEND intervention when delivered at scale is associated with improved BMI and psychosocial outcomes on average, while at the same time having the potential to widen inequalities in these outcomes. We do not know to what extent our findings can be generalised to other weight management programmes or to other community-based interventions. However, our findings suggest that implementation of such interventions should be accompanied by evaluation not only of sustained impact but also of equality of impact at both the individual and population level.
There is little consensus about what constitutes a clinically significant reduction in BMI31 or how much average BMI would need to be reduced in the population of overweight children to reduce the population-level burden of childhood overweight. Further research should clarify these questions. In addition, data from longer-term follow-up were not available following the service intervention (follow-up in the RCT was to 1 year) and so the estimates derived here cannot be used to comment on whether improvements in BMI and other outcomes were sustained beyond the end of the programme when delivered in service settings.
References
Han JC, Lawlor DA, Kimm SYS . Childhood obesity. Lancet 2010; 375: 1737–1748.
Butland B, Jebb S, Kopelman P, McPherson K, Thomas S, Mardell J . Foresight. Tackling Obesities: Future Choices. Project Report. Government Office for Science, UK, 2007.
Reilly JJ, Kelly J . Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes 2011; 35: 891–898.
Health Survey for England 2004. Health of Ethnic Minorities. Full Report. The Information Centre NHS, Leeds, UK, 2006.
Shrewsbury V, Wardle J . Socioeconomic status and adiposity in childhood: a systematic review of cross-sectional studies 1990-2005. Obesity 2008; 16: 275–284.
Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O'Malley C, Stolk RP et al. Interventions for treating obesity in children. Cochrane Database Syst Rev 2009; ((1)): CD001872.
Lorenc T, Petticrew M, Welch V, Tugwell P . What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Health 2013; 67: 190–193.
Aicken C, Roberts H, Arai L . Mapping service activity: the example of childhood obesity schemes in England. BMC Public Health 2010; 10: 310.
Glasgow RE, Vogt TM, Boles SM . Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999; 89: 1322–1327.
McPherson K, Marsh T, Brown M . Foresight. Tackling Obesities: Future Choices - Modelling Future Trends in Obesity and the Impact on Health. Government Office for Science, UK, 2007.
Kerr J, Norman GJ, Adams MA, Ryan S, Frank L, Sallis JF et al. Do neighborhood environments moderate the effect of physical activity lifestyle interventions in adults? Health Place 2010; 16: 903–908.
Sacher PM, Kolotourou M, Chadwick PM, Cole TJ, Lawson MS, Lucas A et al. Randomized controlled trial of the MEND program: a family-based community intervention for childhood obesity. Obesity 2010; 18: S62–S68.
Rosenberg M . Society and the Adolescent Self-image. Princeton University Press, Princeton, NJ, USA, 1965.
Goodman R . The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry 1997; 38: 581–586.
Cole TJ, Freeman JV, Preece MA . Body mass index reference curves for the UK, 1990. Arch Dis Child 1995; 73: 259.
Cole TJ, Green PJ . Smoothing reference centile curves: the LMS method and penalized likelihood. Stat Med 1992; 11: 1305–1319.
Noble M, McLennan D, Wilkinson K, Whitworth A, Dibben C, Barnes H . English Indices of Deprivation 2007. Communities and Local Government, UK, 2008.
Bibby P, Shephard J . Developing a New Classification of Urban and Rural Areas for Policy Purposes – the Methodology. DEFRA, London, UK, 2005.
Ordnance Survey. Points of Interest Database: User Guide and Technical Specification. Ordnance Survey: Southampton, UK, 2011.
Communities and Local Government. Generalised Land Use Database Statistics for England 2005. Department for Communities and Local Government: London, UK, 2007.
Rubin DB . Multiple Imputation for Nonresponse in Surveys. John Wiley and Sons, USA, 1987.
Sterne JAC, White IR, Carlin JB, Spratt M, Royston P, Kenward MG et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 2009; 29: b2393.
Raftery AE . Bayesian model selection in social research. Sociol Methodol 1995; 25: 111–163.
Carpenter JR, Goldstein H, Kenwood MG . REALCOM-IMPUTE software for multilevel multiple imputation with mixed response types. J Stat Softw 2011; 45: 1–14.
Stata Statistical Software. Stata Statistical Software: Release 12. StataCorp LP, College Station, TX, USA, 2011.
Rasbash J, Charlton C, Browne WJ, Healy M, Cameron B . MLwiN Version 2.1. Centre for Multilevel Modelling, University of Bristol, UK, 2009.
Leckie G, Charlton C . runmlwin: Stata Module for Fitting Multilevel Models in the MLwiN Software Package. Centre for Multilevel Modelling, University of Bristol, UK, 2011.
Griffiths LJ, Parsons TJ, Hill AJ . Self-esteem and quality of life in obese children and adolescents: a systematic review. Int J Pediatr Obes 2010; 5: 282–304.
Edwards KL, Clarke GP, Ransley JK, Cade J . The neighbourhood matters: studying exposures relevant to childhood obesity and the policy implications in Leeds, UK. J Epidemiol Community Health 2010; 64: 194–201.
Edwards N . Scaling-up health innovations and interventions in public health: a brief review of the current state-of-the-science. In: Inaugural Conference to Advance the State of the Science and Practice on Scale-up and Spread of Effective Health Programs; 6–8 July; Washington, DC, USA, 2010.
Kolsgaard M, Joner G, Brunborg C, Anderssen S, Tonstad S, Andersen L . Reduction in BMI z-score and improvement in cardiometabolic risk factors in obese children and adolescents. The Oslo Adiposity Intervention Study - a hospital/public health nurse combined treatment. BMC Pediatr 2011; 11: 47.
Acknowledgements
This paper presents independent research funded by the National Institute for Health Research (NIHR). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. The NIHR had no role in study design; the collection, analysis and interpretation of data; and the writing of the article or the decision to submit it for publication. The Centre for Paediatric Epidemiology and Biostatistics was supported in part by the Medical Research Council in its capacity as the MRC Centre of Epidemiology for Child Health (award G0400546). Research at the University College London Institute of Child Health and Great Ormond Street Hospital for Children receives a proportion of the funding from the Department of Health's National Institute for Health Research Biomedical Research Centres funding scheme. SC is supported by an NIHR Senior Fellowship. TJC is funded by MRC Research Grant MR/J004389/1.
Author Contributions
CL, SC, TJC, SM, PC and PS conceived the study and all authors contributed to the study design. JF and HL analysed and interpreted the data. JF drafted the manuscript. TJC and HG advised on aspects of the data analysis. All authors had access to data, except PS and DR due to competing interests. All authors interpreted results and commented on drafts of the manuscript. CL is a guarantor.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
All authors have completed the ICMJE uniform disclosure form (www.icmje.org/coi_disclosure.pdf; available on request from the corresponding author). PC, DR and PS were employees of MEND Central during the project, and PC and PS were also shareholders in MEND Central, PC and PS were two of the developers of the MEND 7–13 intervention. Given that results from the project might support, threaten or have no effect on MEND Central’s success, our grant application to NIHR and subsequent protocol (http://www.nets.nihr.ac.uk/projects/phr/09300505) set out governance measures to ensure that competing interests, and the interests of project stakeholders, were managed appropriately. As part of these measures, PC, PS and DR had no access to data and no role in analyses.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 3.0 Unported License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/3.0/
About this article
Cite this article
Fagg, J., Chadwick, P., Cole, T. et al. From trial to population: a study of a family-based community intervention for childhood overweight implemented at scale. Int J Obes 38, 1343–1349 (2014). https://doi.org/10.1038/ijo.2014.103
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2014.103
This article is cited by
-
Priorities among effective clinical preventive services in British Columbia, Canada
BMC Health Services Research (2022)
-
How effective are physical activity interventions when they are scaled-up: a systematic review
International Journal of Behavioral Nutrition and Physical Activity (2021)
-
Evaluation of the scale-up and implementation of mind, exercise, nutrition … do it! (MEND) in British Columbia: a hybrid trial type 3 evaluation
BMC Pediatrics (2020)
-
Dose response relationship between program attendance and children’s outcomes in a community based weight management program for children and their families
BMC Public Health (2019)
-
Addressing childhood obesity in low-income, ethnically diverse families: outcomes and peer effects of MEND 7–13 when delivered at scale in US communities
International Journal of Obesity (2019)