Abstract
Objectives:
To provide oscillometric blood pressure (BP) reference values in European non-overweight school children.
Design:
Cross-sectional analysis from the IDEFICS study (www.ideficsstudy.eu) database.
Methods:
Standardised BP and anthropometric measures were obtained from children aged 2 to 10.9 years, participating in the 2007–2008 and 2009–2010 IDEFICS surveys. Age- and height-specific systolic and diastolic pressure percentiles were calculated by GAMLSS, separately for boys and girls, in both the entire population (n=16 937) and the non-overweight children only (n=13 547). The robustness of the models was tested by sensitivity analyses carried out in both population samples.
Results:
Percentiles of BP distribution in non-overweight children were provided by age and height strata, separately for boys and girls. Diastolic BP norms were slightly higher in girls than in boys for similar age and height, while systolic BP values tended to be higher in boys starting from age 5 years. Sensitivity analysis, comparing BP distributions obtained in all children with those of non-overweight children, showed that the inclusion of overweight/obese individuals shifted the references values upward, in particular systolic BP in girls at the extreme percentiles.
Conclusions:
The present analysis provides updated and timely information about reference values for BP in children aged 2 to <11 years that may be useful for monitoring and planning population strategies for disease prevention.
Similar content being viewed by others
Introduction
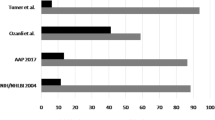
Measuring blood pressure (BP) during physical examination in paediatric clinical practice was quite unusual until a few years ago. As a result, BP distributions for children have only been published recently. In particular, this gap has been filled by the publication of the Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents1 by the National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (NHBPEP), who provided systolic (SBP) and diastolic (DBP) pressure percentiles stratified by sex and height from a large US representative population aged 1–17 years.
BP in children is determined by both height and, as for adults,2 weight; however, in the paediatric age group, the portion attributable to height may be physiological, whereas that contributed by excess weight may not be. Indeed the NHBPEP percentiles were stratified by height, but also included overweight and obese children.1 Accordingly, the increased prevalence of paediatric hypertension previously reported3 could be explained partly by the increased prevalence of overweight and obesity in children.4 However, the inclusion of overweight individuals in the normative BP values might lead to values as high as those that are used to define higher-than-normal BP in adults (for example, >120/80 mm Hg),2 being considered as ‘normal BP’ for a child. For these reasons, Rosner et al.5 first calculated normative BP values in non-overweight children only and, for this purpose, re-analysed the NHBPEP data;1 thus, reference BP values in childhood and adolescence are available for the US population in both the entire population1 and non-overweight individuals.5
In Europe, normative BP values are available from several population samples6, 7, 8, 9 in which overweight and obese children were included; BP norms for non-overweight children and adolescents are available from European studies only referring to single countries, namely Germany10 and Poland.11
The present study aims to provide age-, height-, and sex-stratified SBP and DBP reference values in non-overweight European children, 2.0–10.9 years old, participating in the IDEFICS study. Further, the study compared these normative values with those obtained from the entire sample of children participating in the study by including overweight and obese children in the analysis.
Participants and methods
The IDEFICS study (Identification and prevention of Dietary- and lifestyle-induced health EFfects In Children and infantS) is an epidemiological multi-centre European project, funded by the European Commission within the Sixth Framework Program, that aimed to identify nutritional and lifestyle-associated aetiological factors linked to childhood obesity and related morbidities. A cohort of 16 228 children aged 2–9 years (51% of the eligible sample), recruited from eight European countries (Germany, Hungary, Italy, Cyprus, Spain, Estonia, Sweden and Belgium), was examined at baseline between September 2007 and May 2008, according to a standardised protocol.12 A follow-up survey was carried out from September 2009 to May 2010, during which an additional 2517 children, who did not participate in the baseline survey, were included (newcomers). Parents, or legal guardians, provided written informed consent to participate in the full programme or in a selected set of examination modules. For each survey centre, the approval of the local ethics committee was obtained.
The overall sample (Figure 1) included 16 937 children (baseline survey plus newcomers at the follow-up survey) aged 2.0–10.9 years after the exclusion of 1808 participants (boys=50.8%; age=5.2±1.9 years; body mass index (BMI)=16.3±2.3 kg m−2, mean (M)±s.d.) for whom BP data were missing, who were on average slightly younger than those included. For the purposes of the present analysis, the subgroup of non-overweight children (n=13 547) was selected for the main analysis.
Physical examination
Children underwent physical examination in a quiet and warm room, according to a standardised procedure with validated intra- and inter-observer reliability for all the measurements.13,14 Body weight was measured, with participants fasting and wearing underwear, using a prototype of the TANITA BC 420 SMA digital scale (TANITA Europe GmbH, Sindelfingen, Germany) specifically adapted for children. Height was measured by a stadiometer (seca 225, seca, Birmingham, UK), with children standing with feet slightly apart and back touching the vertical board and with head in a Frankfort plane. As for the weight measurement, the children were wearing underwear only, with all hair ornaments removed and all braids undone. For the purpose of the present analysis, sex-specific height percentiles were calculated for each 1-year age step.
BMI was calculated as weight in kilograms divided by the square of the height in meters. Participants were classified as normal weight, overweight or obese according to the standard criteria adopted by the International Childhood Obesity Task Force, recently updated by Cole and Lobstein.15 The present analysis was carried out in both the entire population and non-overweight children only.
BP was measured with an automated oscillometric device (Welch Allyn 4200B-E2, Welch Allyn Inc., Skaneateles Falls, NY, USA),16 according to a standardised procedure. Briefly, the right arm was commonly used, unless it was injured. For the choice of the appropriate cuff size, arm circumference measurement was taken; the length of the upper arm was determined by measuring (with a SECA 200 band) the distance between the acromion and the olecranon along the lateral side of the upper arm with the participant standing upright, with the elbow flexed to 90° with the palm facing superiorly. The midpoint was marked on the lateral side of the arm. With the arm relaxed and the elbow extended with the palm facing the observer, the tape was placed around the arm without compressing the tissues, perpendicularly to the long axis of the arm at the marked midpoint, and the circumference recorded to the nearest 0.1 cm. The cuff length for BP measurement was chosen according to the arm circumference and positioned with the bottom edge ~2 cm above the cubital fossa.1
Children were asked to sit for at least 5 min before measurement, with pre-school children seated preferably on their parent’s lap. Older children were asked to sit in a chair supporting the back and feet with legs uncrossed. A pillow was used, if necessary, to support the arm while the measurement was taken. Two recordings were taken, with a 2-min interval between each, plus a further measurement in case of a >5% difference in BP between the first two readings. The average of the two (or three) measurements was used for statistical analysis.
Databases included automated plausibility checks. All numerical variables were entered twice, independently. Inconsistencies identified by additional plausibility checks were rectified by the study centres.
BP percentile calculation
To calculate percentile curves for the whole study sample and non-overweight children, we used the General Additive Model for Location Scale and Shape (GAMLSS) that was developed by Rigby and Stasinopoulos.16 This method is an extension of the LMS method to model the distribution of SBP and DBP depending on multiple covariates while accounting for dispersion, skewness,and particularly the kurtosis of this distribution.17,18
We calculated percentile curves of SBP and DBP as a function of the covariates age and height stratified by sex using the GAMLSS method as extension of the LMS method. The LMS method models three parameters: the skewness (L) accounts for the deviation from a normal distribution using a Box–Cox transformation, the median (M) of the outcome variable is modelled depending on one explanatory variable, and the coefficient of variation (S) accounts for the variation of data points around the mean and adjusts for non-uniform dispersion. The GAMLSS method is able to particularly model the kurtosis using other distributions and to include more than one covariate. We used the GAMLSS package (version 4.1–0) of the statistical software R (version 3.0.1).19 Different distributions, that is, Box–Cox power exponential, Box–Cox Cole and Green, and Box–Cox t (BCT) distribution, were fitted to the observed distributions of SBP as well as DBP. Moreover, the influence of age and height on parameters of the considered distributions were modelled as a constant, as a linear function or as a cubic spline of the covariates. Worm plots were used as a diagnostic tool to assess whether adjustment for kurtosis was required.20 Goodness of fit was assessed by the Bayesian Information Criterion and by Q–Q plots to select the final model including the fitted distribution of SBP and DBP and the influence of covariates on distribution parameters. Finally, age- and height-dependent curves for the 1st, 3rd, 10th, 25th, 50th, 75th, 90th, 97th and 99th percentiles were calculated based on the model that showed the best goodness of fit,18,19 separately for boys and girls.
With regard to the complete sample, the final models for both SBP and DBP in boys and girls were based on a BCT distribution. With regard to SBP, in both samples log(μ) for boys and μ for girls were modelled as a linear function of age and height, and log(σ), ν and log(τ) as constant for both sexes with one exception: in non-overweight girls ν was linearly dependent on age. With regard to DPB, in both samples μ was modelled as a linear function of age and height for girls and non-overweight boys, but in the overall sample of boys log(μ) was modelled as a linear function of age and height. In all DBP models the parameters log(σ), ν and log(τ) were considered as constant.
BP percentiles (for SBP and DBP) of the resulting curves in both non-overweight children only and the entire population were reported stratified by 1-year age steps from 2.0 to 10.9 years and by seven age-specific height percentiles (3rd, 10th, 25th, 50th, 75th, 90th and 97th).
For sensitivity analyses, we compared the 1st, 10th, 25th, 50th, 75th, 90th and 99th percentile curves based on the whole study sample with the percentile curves based on non-overweight children for both SBP and DBP.
Results
Table 1 shows the characteristics of the population under investigation, either as a whole (panel A) or restricted to non-overweight children (panel B). The sample was equally composed of boys and girls (girls=49.6% and 48.8% in the entire population and in non-overweight children, respectively). The prevalence of overweight/obesity was 21% for girls and 19% for boys. However, differences in prevalence were observed across age categories, with overweight and obesity being less common among kindergarten children in comparison with older participants (Table 1).
Table 2 shows the age- and height-stratified SBP distribution in non-overweight children participating in the IDEFICS study; in particular, the 1st, 3rd, 10th, 25th, 50th, 75th, 90th, 97th and 99th SBP percentiles are shown separately for boys and girls. Similarly, Table 3 shows the same DBP percentiles in non-overweight children by age and height.
BP showed a significant positive age and height trend. It seems as though this trend is more pronounced for height (Supplementary Figures A and B) in the age range under investigation. SBP percentiles tended to be higher in girls than in boys up to the age of 5 years; subsequently the trend was reversed, with higher BP values in boys than in girls; as depicted in Table 2, the older the child, the greater the difference between sexes. DBP, in contrast, showed a different pattern (Table 3), being higher in girls than in boys at any age under investigation.
The corresponding age- and height-specific SBP and DBP percentiles from the population as a whole are provided, separately for boys and girls, in Supplementary Tables A and B.
In Figure 2, BP percentiles (1st, 3rd, 10th, 25th, 50th, 75th, 90th, 97th and 99th) are depicted in non-overweight girls (left) and boys (right); in particular, SBP (top panels) and DBP (bottom panels) at median height were obtained from age 2 to 10.9 years. The plots show, in both girls and boys, a steeper increase of SBP than DBP; further, as expected, a trend to higher DBP values in girls than in boys was observed in the age range under investigation.
Systolic (top panels) and diastolic (bottom panels) blood pressure percentiles at median height by age in non-overweight girls (left, n=6609) and boys (right, n=6938) participating in the IDEFICS study. DBP, diastolic blood pressure; SBP, systolic blood pressure. Non-overweight children included thin and normal weight children according to Cole and Lobstein.15
Figure 3 shows the same data as in Figure 2, but referring to the entire population, thus also including overweight and obese children: in this case, differences between sexes, in particular higher DBP values at the same age and height, were even more apparent. Further, in this sample, 12.7% and 9.0% of children showed SBP and DBP values, respectively, above the 97th percentile calculated in non-overweight children.
Finally, sensitivity analyses were carried out (Figure 4) at 1st, 10th, 25th, 50th, 75th, 90th and 99th SBP (top panels) and DBP (bottom panels) in girls (left) and boys (right) in order to compare the plots between the whole sample and non-overweight children only. There was an apparently more pronounced positive age trend of SBP values in girls than in boys at the extreme percentiles of the distribution when overweight and obese children were included in the analysis. Sensitivity analysis did not show differences in DBP plots between the entire sample and overweight/obese children only, for both boys and girls.
Comparison (sensitivity analysis) between systolic (top panels) and diastolic (bottom panels) blood pressure percentiles by age and median height in non-overweight children only (continuous line) and all participants (dotted line) in the IDEFICS study. Data are shown separately for girls (left) and boys (right). DBP, diastolic blood pressure; SBP, systolic blood pressure. Non-overweight children included thin and normal weight children according to Cole and Lobstein.15
Discussion
The present study provides normative age- and height-specific SBP and DBP values drawn from a large sample of European girls and boys in the age range 2.0–10.9 years participating in the IDEFICS study. BP percentiles were calculated in non-overweight children and in the entire population and then sensitivity analyses were carried out to test the robustness of our models.
The study shows that, among non-overweight children, SBP is higher in girls than in boys up to the age of 5 years, a trend that is reversed in older children, while DBP distribution is shifted to the right in girls, in comparison with boys, at any age and percentile of height. Differences in BP between boys and girls (with higher values in the latter) have been previously documented in the age range 2–11 years, both in the general population21, 22, 23, 24 and in selected samples of non-overweight children adopting the GAMLSS method.5,10
The study also provides a comparison between BP norms obtained in a large sample of school children either including or excluding overweight or obese participants. It is apparent from this analysis that differences between sexes appear to be more pronounced in the population including overweight and obese children at an older age and at the extremes of the distribution. Previous studies have consistently shown that sex differences are more pronounced during pre-puberty21, 22, 23, 24 that usually occurs in girls earlier than in boys. The BP sexual dimorphism we observed in the population as a whole is a well-documented phenomenon in adults.25 Our findings could be explained by the earlier occurrence of biological changes leading to sexual maturation in girls. Alternatively, the overall higher prevalence of overweight and obesity observed in girls in the IDEFICS sample might be responsible.
The sensitivity analysis also provided insight regarding the possibility that determining reference BP values in children including overweight and obese individuals may be subject to bias.5 Body weight and height are the most important determinants of BP in children, as BP increases linearly with both anthropometric factors. In fact, differences exist between the two factors in their association with BP: while changes in BP associated with changes in height may be considered the consequence of a physiological process, the relationship between body weight and BP is, at least in part, a physiopathological deviation from normality.5,10,21,26,27 Indeed, adult prehypertension, that is, SBP ⩾120 and/or DBP ⩾80 mm Hg, was documented in our sample in 0.8% and 2.1% overweight/obese children, respectively, in the age groups 2–6 and 6–11 years. Only ⩽0.4% non-overweight participants had an SBP of at least 120 mm Hg. In practice, calculating the BP norms for a general population would keep children within the norms although they would be included in an ‘at-risk’ category if they were adults.28
It should be clearly stated that the present paediatric reference BP values do not provide criteria to diagnose hypertension in children. In the IDEFICS study, BP measurements were taken on a single occasion, thus making it difficult to classify hypertension because of the known intrinsic variability of BP, well documented in the paediatric population,29 which in this case could lead to a possible overestimation of BP values. In the NHBPEP report,1 the criteria used to define hypertension were provided, but, in that study, BP measurements were taken on three separate occasions. The diagnosis of paediatric hypertension is not as straightforward as it is in adults, in whom the long-term impact on health of elevated BP is well documented.2,30 It is recognised that the BP in children tends to increase up to adulthood and, in general, children whose BP values are in the right part of the distribution tend to keep the same position later in life,1,2,31,32 possibly to a greater extent if co-existing with overweight or obesity.33 However, the absolute risk of cardiovascular diseases associated with elevated BP in childhood remains to be evaluated.34, 35, 36 Under these conditions, the normative BP values derived from the IDEFICS study population actually provide the cutoffs to identify those children who are at higher risk for paediatric hypertension and for whom further BP measurements should be scheduled or even a preventative, healthy lifestyle should be promoted.1
The present study is the first, to the best of our knowledge, to provide BP norms in a large multi-national European paediatric population composed of non-overweight children, thus advancing current knowledge by (i) extending the national or local data recently published6, 7, 8, 9, 10, 11,23 in European population samples and (ii) updating the former European child BP norms.37 Further strengths were the standardisation of the procedures across centres participating in the IDEFICS study12, 13, 14 that strongly limited the possibility of technical biases and increased the reliability of collected data, and the adoption of updated statistical methods to calculate reference BP percentiles.
The comparison of the present data with other data from similar studies may be possibly limited by the different BP readings obtained from different automated devices, each one with its own calculation algorithm. In spite of this limitation, however, the use of automated devices is recommended in multi-centre studies because it avoids the occurrence of any possible observer bias. This characteristic of automated devices, in addition to the standardisation of the procedures in the IDEFICS study, confers robust reliability to collected data. One other possible limitation of the study is the age range of participants, which did not provide any information from early childhood to late adolescence. Nonetheless, in view of the paucity of available data, the absence of BP norms in adolescents appears to be less relevant. However, the collection of BP data in adolescents will be one of the objectives of our ongoing I.Family study (www.ifamilystudy.eu). Finally, the present analysis did not provide criteria for the diagnosis of paediatric hypertension: this aspect was discussed above but, regardless, it would have required a different study design.
The present study provides updated and timely information that may contribute to filling a gap in knowledge that may be prospectively useful in planning population strategies for disease prevention. Further, the results of the present analysis might also support clinical practice by providing reliable reference BP values in children and thus encouraging paediatricians to include blood pressure measurement as a routine procedure during physical examination.
References
National Blood Pressure Education Working Group on High Blood Pressure in Children and Adolescents. Fourth report on the diagnosis, evaluation and treatment of high blood pressure in children and adolescents: a working group report from the National High Blood Pressure Education Program. Pediatrics 2004; 114 (Suppl): 555–576.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr et al. Joint National Committee on Prevention Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42: 1206–1252.
Falkner B . Hypertension in children and adolescents: epidemiology and natural history. Pediatr Nephrol 2010; 25: 1219–1224.
Chiolero A, Bovet P, Paradis G, Paccaud F . Has blood pressure increased in children in response to the obesity epidemic? Pediatrics 2007; 119: 544–553.
Rosner B, Cook N, Portman R, Daniels S, Falkner B . Determination of blood pressure percentiles in normal-weight children: some methodological issues. Am J Epidemiol 2008; 167: 653–666.
Menghetti E, Virdis R, Strambi M, Patriarca V, Riccioni MA, Fossali E et al. Blood pressure in childhood and adolescence: the Italian normal standards. Study Group on Hypertension of the Italian Society of Pediatrics. J Hypertens 1999; 17: 1363–1372.
Jackson LV, Thalange NK, Cole TJ . Blood pressure centiles for Great Britain [published correction appears in Arch Dis Child 2007;92:563] Arch Dis Child 2007; 92: 298–303.
Munkhaugen J, Lydersen S, Widerøe TE, Hallan S . Blood pressure reference values in adolescents: methodological aspects and suggestions for Northern Europe tables based on the Nord-Trøndelag Health Study II. J Hypertens 2008; 26: 1912–1918.
Túri S, Baráth A, Boda K, Tichy M, Károly E . Blood pressure reference tables for Hungarian adolescents aged 11-16 years. Kidney Blood Press Res 2008; 31: 63–69.
Neuhauser HK, Thamm M, Ellert U, Hense HW, Rosario AS . Blood pressure percentiles by age and height from nonoverweight children and adolescents in Germany. Pediatrics 2011; 127: e978–e988.
Kułaga Z, Litwin M, Grajda A, Kułaga K, Gurzkowska B, Góźdź M, Pan H OLAF Study Group. Oscillometric blood pressure percentiles for Polish normal-weight school-aged children and adolescents. J Hypertens 2012; 30: 1942–1954.
Ahrens W, Bammann K, Siani A, Buchecker K, De Henauw S, Iacoviello L et al. IDEFICS Consortium. The IDEFICS cohort: design, characteristics and participation in the baseline survey. Int J Obes (Lond) 2011; 35 (Suppl 1): S3–S15.
Stomfai S, Ahrens W, Bammann K, Kovács E, Mårild S, Michels N et al. IDEFICS Consortium. Intra- and inter-observer reliability in anthropometric measurements in children. Int J Obes (Lond) 2011; 35 (Suppl 1): S45–S51.
Bammann K, Sioen I, Huybrechts I, Casajús JA, Vicente-Rodríguez G, Cuthill R et al. IDEFICS Consortium. The IDEFICS validation study on field methods for assessing physical activity and body composition in children: design and data collection. Int J Obes (Lond) 2011; 35 (Suppl 1): S79–S87.
Cole TJ, Lobstein T . Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes 2012; 7: 284–294.
Alpert BS . Validation of the Welch Allyn spot vital signs blood pressure device according to the ANSI/AAMI SP10: 2002. Accuracy and cost-efficiency successfully combined. Blood Press Monit 2007; 12: 345–347.
Rigby RA, Stasinopoulos DM . Generalized additive models for location, scale and shape. J R Stat Soc Ser C (Appl Stat) 2005; 54: 507–554.
Cole TJ, Stanojevic S, Stocks J, Coates AL, Hankinson JL, Wade AM . Age-and size-related reference ranges: a case study of spirometry through childhood and adulthood. Stat Med 2009; 28: 880–898.
Stasinopoulos DM, Rigby RA . Generalized additive models for location scale and shape (GAMLSS) in R. J Stat Softw 2007; 23: 1–46.
van Buuren S, Fredriks AM . Worm plot: a simple diagnostic device for modelling growth reference curves. Stat Med 2001; 20: 1259–1277.
Barba G, Casullo C, Dello Russo M, Russo P, Nappo A, Lauria F et al. Gender-related differences in the relationships between blood pressure, age and body size in pre-pubertal children. Am J Hypertens 2008; 21: 1007–1010.
Barba G, Giacco R, Clemente G, Venezia A, Russo P, Grimaldi C et al. The BRAVO Project: screening for childhood obesity in a primary school setting. Nutr Metab Cardiovasc Dis 2001; 11 (Suppl 4): 103–108.
Barba G, Troiano E, Russo P, Strazzullo P, Siani A . Body mass, fat distribution and blood pressure in Southern Italian children: results of the ARCA project. Nutr Metab Cardiovasc Dis 2006; 16: 239–248.
Dasgupta K, O’Loughlin J, Chen S, Karp I, Paradis G, Tremblay J et al. Emergence of sex differences in prevalence of high systolic blood pressure: analysis of a longitudinal adolescent cohort. Circulation 2006; 114: 2663–2670.
Medina RA, Aranda E, Verdugo C, Kato S, Owen GI . The action of ovarian hormones in cardiovascular disease. Biol Res 2003; 36: 325–341.
Maffeis C, Pietrobelli A, Grezzani A, Provera S, Tato L . Waist circumference and cardiovascular risk factors in prepubertal children. Obes Res 2001; 9: 179–187.
Aguilar A, Ostrow V, De Luca F, Suarez E . Elevated ambulatory blood pressure in a multi-ethnic population of obese children and adolescents. J Pediatr 2010; 156: 930–935.
Neuhauser HK, Rosario AS, Thamm M, Ellert U . Prevalence of children with blood pressure measurements exceeding adult cut offs for optimal blood pressure in Germany. Eur J Cardiovasc Prev Rehabil 2009; 16: 195–200.
Falkner B, Gidding SS, Portman R, Rosner B . Blood pressure variability and classification of prehypertension and hypertension in adolescence. Pediatrics 2008; 122: 238–242.
Vasan RS, Larson MG, Leip MS, Evans JC, O’Donnell CJ, Kannel WB et al. Impact of high normal blood pressure on the risk of cardiovascular disease. N Engl J Med 2001; 345: 1291–1297.
Chen X, Wang Y . Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation 2008; 117: 3171–3180.
Sun SS, Grave GD, Siervogel RM, Pickoff AA, Arslanian SS, Daniels SR . Systolic blood pressure in childhood predicts hypertension and metabolic syndrome later in life. Pediatrics 2007; 119: 237–246.
Falkner B, Gidding S . Childhood obesity and blood pressure: back to the future? Hypertension 2011; 58: 754–755.
Chiolero A, Bovet P, Paradis G . Screening for elevated blood pressure in children and adolescents: a critical appraisal. JAMA Pediatr 2013; 167: 266–273.
Thompson M, Dana PT, Bougatsos C, Blazina I, Norris S . Screening for Hypertension in Children and Adolescents to Prevent Cardiovascular Disease: Systematic Review for the U.S. Preventive Services Task Force. Publication No. 13-05181-EF-1. Agency for Healthcare Research and Quality, February 2013. http://www.ncbi.nlm.nih.gov/books/NBK126735/pdf/TOC.pdf (accessed 21 November 2013).
Juonala M, Magnussen CG, Venn A, Dwyer T, Burns TL, Davis PH et al. Influence of age on associations between childhood risk factors and carotid intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study, the Childhood Determinants of Adult Health Study, the Bogalusa Heart Study, and the Muscatine Study for the International Childhood Cardiovascular Cohort (i3C) Consortium. Circulation 2010; 122: 2514–2520.
de Man SA, Andre JL, Bachmann H, Grobbee DE, Ibsen KK, Laaser U et al. Blood pressure in childhood: pooled findings of six European studies. J Hypertens 1991; 9: 109–114.
Acknowledgements
We sincerely wish to thank the parents and children who participated in the study. This work was done as part of the IDEFICS Study (www.idefics.eu). We gratefully acknowledge the financial support of the European Community within the Sixth RTD Framework Programme Contract No. 016181 (FOOD). We are also grateful to the Volkswagen Foundation that financially supported the production of this supplement.
DISCLAIMER
The information in this document reflects the authors’ views and is provided as it is.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Barba, G., Buck, C., Bammann, K. et al. Blood pressure reference values for European non-overweight school children: The IDEFICS study. Int J Obes 38 (Suppl 2), S48–S56 (2014). https://doi.org/10.1038/ijo.2014.135
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2014.135
This article is cited by
-
The compatibility of new blood pressure reference values for Korean children and adolescents with the US reference: the Korean Working Group of Pediatric Hypertension
Clinical Hypertension (2022)
-
Establishing percentiles for blood pressure based on absolute height for children and adolescents
BMC Pediatrics (2021)
-
The role of lifestyle and non-modifiable risk factors in the development of metabolic disturbances from childhood to adolescence
International Journal of Obesity (2020)
-
A comparison of clinical paediatric guidelines for hypotension with population-based lower centiles: a systematic review
Critical Care (2019)
-
Red meat and chicken consumption and its association with high blood pressure and obesity in South Korean children and adolescents: a cross-sectional analysis of KSHES, 2011–2015
Nutrition Journal (2017)