Abstract
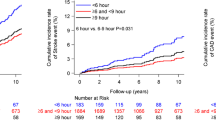
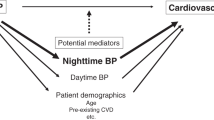
Diagnosis of hypertension and clinical decisions regarding its treatment are typically based upon daytime clinic blood pressure (BP) measurements, occasionally supplemented by wake-time patient self-assessment. Yet, correlation between BP level and target organ damage, cardiovascular disease (CVD) risk, and long-term prognosis is higher for ambulatory BP monitoring (ABPM) measurements. Numerous studies consistently reveal CVD events are better predicted by the asleep than awake or 24 h BP means. In addition, when the asleep BP mean is adjusted by the awake mean, only the former is a significant independent predictor of outcome. Endogenous circadian rhythms explain statistically and clinically significant ingestion time differences in efficacy, duration of action, safety and/or effects on the daily BP pattern of most hypertension medications and their combinations. Bedtime versus morning-time ingestion of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, independent of drug terminal half-life, both better reduces asleep BP and normalizes the daily BP profile into a more normal dipper pattern. The recently completed prospective outcome MAPEC Study verifies therapeutic restoration of the normal sleep-time BP decline, a novel therapeutic goal most effectively achieved by ingestion of the entire daily dose of ⩾1 conventional hypertension medications at bedtime, best decreases CVD morbidity and mortality. Our findings indicate around-the-clock ABPM is a clinical necessity to accurately detect abnormal sleep-time BP and assess CVD risk, and that hypertension ought to be managed by a bedtime therapeutic strategy, preferably one including medication that antagonizes the activities and actions of the renin–angiotensin–aldosterone system.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013; 31 (7): 1281–1357.
Clement DL, De Buyzere ML, De Bacquer DA, de Leeuw PW, Duprez DA, Fagard RH et al. Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med 2003; 348 (24): 2407–2415.
Hermida RC, Ayala DE, Mojón A, Fernández JR . Decreasing sleep-time blood pressure determined by ambulatory monitoring reduces cardiovascular risk. J Am Coll Cardiol 2011; 58 (11): 1165–1173.
Hermida RC, Smolensky MH, Ayala DE, Portaluppi F, Crespo JJ, Fabbian F et al. 2013 ambulatory blood pressure monitoring recommendations for the diagnosis of adult hypertension, assessment of cardiovascular and other hypertension-associated risk, and attainment of therapeutic goals. Joint recommendations from the International Society for Chronobiology (ISC), American Association of Medical Chronobiology and Chronotherapeutics (AAMCC), Spanish Society of Applied Chronobiology, Chronotherapy, and Vascular Risk (SECAC), Spanish Society of Atherosclerosis (SEA), and Romanian Society of Internal Medicine (RSIM). Chronobiol Int 2013; 30 (3): 355–410.
Hermida RC, Ayala DE, Portaluppi F . Circadian variation of blood pressure: The basis for the chronotherapy of hypertension. Adv Drug Deliv Rev 2007; 59 (9-10): 904–922.
Fabbian F, Smolensky MH, Tiseo R, Pala M, Manfredini R, Portaluppi F . Dipper and non-dipper blood pressure 24-hour patterns: circadian rhythm-dependent physiologic and pathophysiologic mechanisms. Chronobiol Int 2013; 30 (1-2): 17–30.
Lakatua DJ, Haus E, Halberg F, Halberg E, Wendt HW, Sackett-Lundeen LL et al. Circadian characteristics of urinary epinephrine and norepinephrine from healthy young women in Japan and U.S.A. Chronobiol Int 1986; 3 (3): 189–195.
Angeli A, Gatti G, Masera R . Chronobiology of the hypothalamic-pituitary-adrenal and renin-angiotensin-aldosterone systems. In: Touitou Y, Haus E (eds) Biologic Rhythms in Clinical and Laboratory Medicine. Springer-Verlag: Berlin, 1992 pp 292–314.
Kool MJ, Wijnen JA, Derkx FH, Struijker Boudier HA, Van Bortel LM . Diurnal variation in prorenin in relation to other humoral factors and hemodynamics. Am J Hypertens 1994; 7 (8): 723–730.
Smolensky MH, Hermida RC, Castriotta RJ, Portaluppi F . Role of sleep-wake cycle on blood pressure circadian rhythms and hypertension. Sleep Med 2007; 8 (6): 668–680.
Hermida RC, Ayala DE, Mojón A, Fernández JR . Influence of circadian time of hypertension treatment on cardiovascular risk: results of the MAPEC study. Chronobiol Int 2010; 27 (8): 1629–1651.
Hermida RC, Ayala DE, Mojón A, Fernández JR . Influence of time of day of blood pressure-lowering treatment on cardiovascular risk in hypertensive patients with type 2 diabetes. Diabetes Care 2011; 34 (6): 1270–1276.
Hermida RC, Ayala DE, Mojón A, Fernández JR . Bedtime dosing of antihypertensive medications reduces cardiovascular risk in CKD. J Am Soc Nephrol 2011; 22 (12): 2313–2321.
Portaluppi F, Tiseo R, Smolensky MH, Hermida RC, Ayala DE, Fabbian F . Circadian rhythms and cardiovascular health. Sleep Med Rev 2012; 16: 151–166.
Verdecchia P, Porcellati C, Schillaci G, Borgioni C, Ciucci A, Battistell M et al. Ambulatory blood pressure: an independent predictor of prognosis in essential hypertension. Hypertension 1994; 24 (6): 793–801.
Kario K, Pickering TG, Matsuo T, Hoshide S, Schwartz JE, Shimada K . Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension 2001; 38 (4): 852–857.
Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens 2002; 20 (11): 2183–2189.
Dolan E, Stanton A, Thijs L, Hinedi K, Atkins N, McClory S et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension 2005; 46 (1): 156–161.
Ingelsson E, Bjorklund-Bodegard K, Lind L, Arnlov J, Sundstrom J . Diurnal blood pressure pattern and risk of congestive heart failure. JAMA 2006; 295 (24): 2859–2866.
Eguchi K, Pickering TG, Hoshide S, Ishikawa J, Ishikawa S, Schwartz J et al. Ambulatory blood pressure is a better marker than clinic blood pressure in predicting cardiovascular events in patients with/without type 2 diabetes. Am J Hypertens 2008; 21 (4): 443–450.
Salles GF, Cardoso CR, Muxfeldt ES . Prognostic influence of office and ambulatory blood pressures in resistant hypertension. Arch Intern Med 2008; 168 (21): 2340–2346.
Hermida RC, Ayala DE, Fernández JR, Mojón A . Sleep-time blood pressure: Prognostic value and relevance as a therapeutic target for cardiovascular risk reduction. Chronobiol Int 2013; 30 (1-2): 68–86.
Hermida RC, Ayala DE, Mojón A, Fernández JR . Blunted sleep-time relative blood pressure decline increases cardiovascular risk independent of blood pressure level—the ‘normotensive non-dipper’ paradox. Chronobiol Int 2013; 30 (1-2): 87–98.
Kikuya M, Ohkubo T, Asayama K, Metoki H, Obara T, Saito S et al. Ambulatory blood pressure and 10-year risk of cardiovascular and noncardiovascular mortality. The Ohasama Study. Hypertension 2005; 45 (2): 240–245.
Ben-Dov IZ, Kark JD, Ben-Ishay D, Mekler J, Ben-Arie L, Bursztyn M . Predictors of all-cause mortality in clinical ambulatory monitoring. Unique aspects of blood pressure during sleep. Hypertension 2007; 49 (6): 1235–1241.
Fagard RH, Celis H, Thijs L, Staessen JA, Clement DL, De Buyzere ML et al. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension 2008; 51 (1): 55–61.
Minutolo R, Agarwal R, Borrelli S, Chiodini P, Bellizzi V, Nappi F et al. Prognostic role of ambulatory blood pressure measurement in patients with nondialysis chronic kidney disease. Arch Intern Med 2011; 171 (12): 1090–1098.
Hermida RC, Ayala DE, Mojón A, Fernández JR . Sleep-time blood pressure and the prognostic value of isolated-office and masked hypertension. Am J Hypertens 2012; 25 (3): 297–305.
Hermida RC, Ayala DE, Fontao MJ, Mojón A, Fernández JR . Ambulatory blood pressure monitoring: importance of sampling rate and duration—48 versus 24 h—on the accurate assessment of cardiovascular risk. Chronobiol Int 2013; 30 (1-2): 55–67.
Hermida RC, Ayala DE, Fernández JR, Mojón A, Smolensky MH, Fabbian F et al. Administration-time-differences in effects of hypertension medications on ambulatory blood pressure regulation. Chronobiol Int 2013; 30 (1-2): 280–314.
Hermida RC, Ayala DE, Fernández JR, Portaluppi F, Fabbian F, Smolensky MH . Circadian rhythms in blood pressure regulation and optimization of hypertension treatment with ACE inhibitor and ARB medications. Am J Hypertens 2011; 24 (4): 383–391.
Hermida RC, Ayala DE, Mojón A, Fernández JR . Cardiovascular risk of essential hypertension: Influence of class, number, and treatment-time regimen of hypertension medications. Chronobiol Int 2013; 30 (1-2): 315–327.
Ayala DE, Hermida RC, Mojón A, Fernández JR . Cardiovascular risk of resistant hypertension: Dependence on treatment-time regimen of blood pressure-lowering medications. Chronobiol Int 2013; 30 (1-2): 340–352.
Ayala DE, Moyá A, Crespo JJ, Castiñeira C, Domínguez-Sardiña M, Gomara S et al. Circadian pattern of ambulatory blood pressure in hypertensive patients with and without type 2 diabetes. Chronobiol Int 2013; 30 (1-2): 99–115.
Hermida RC, Ayala DE, Mojón A, Fernández JR . Role of time-of-day of hypertension treatment on the J-shaped relationship between blood pressure and cardiovascular risk. Chronobiol Int 2013; 30 (1-2): 328–339.
National Institute for Health and Clinical Excellence. Hypertension: The clinical management of primary hypertension in adults. NICE Clinical Guidelines 127: Methods, evidence and recommendations. National Clinical Guidelines Centre: London, UK, 2011. http://guidance.nice.org.uk/CG/Wave2/14 Last accessed September 14, 2013.
American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care 2013; 36 (Suppl 1): S11–S66.
Acknowledgements
This research is supported by unrestricted grants from Ministerio de Ciencia e Innovación (SAF2009-7028-FEDER); Consellería de Economía e Industria, Xunta de Galicia (INCITE07-PXI-322003ES; INCITE08-E1R-322063ES; INCITE09-E2R-322099ES; IN845B-2010/114; 09CSA018322PR); European Research Development Fund and Consellería de Cultura, Educación e Ordenación Universitaria, Xunta de Galicia (CN2012/251 & CN2012/260); and Vicerrectorado de Investigación, University of Vigo (all grants awarded to RC Hermida, DE Ayala, A Mojón and JR Fernández).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest
Rights and permissions
About this article
Cite this article
Hermida, R., Ayala, D., Mojón, A. et al. Sleep-time ambulatory blood pressure as a novel therapeutic target for cardiovascular risk reduction. J Hum Hypertens 28, 567–574 (2014). https://doi.org/10.1038/jhh.2014.1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2014.1
Keywords
This article is cited by
-
On the use of actigraphy in clinical evaluation of diurnal blood pressure profile
Somnologie (2020)
-
Left atrial enlargement and blood pressure variability in untreated hypertensive patients
Hypertension Research (2016)
-
Chronotherapy with conventional blood pressure medications improves management of hypertension and reduces cardiovascular and stroke risks
Hypertension Research (2016)
-
Autonomic Dysfunction: How to Identify and When to Treat?
High Blood Pressure & Cardiovascular Prevention (2016)
-
Sleep-time BP: prognostic marker of type 2 diabetes and therapeutic target for prevention
Diabetologia (2016)