Abstract
Objective:
Neonatal intubation is a life-saving procedural skill required by pediatricians. Trainees receive insufficient clinical exposure to develop this competency. Traditional training comprises a Neonatal Resuscitation Program (NRP) complemented by clinical experience. More recently, simulation is being used in procedural skills training. The objective of this study is to examine the impact of a simulation session, which teaches the skill of neonatal intubation by comparing pre- and post-intervention performance, and examining transferability of skill acquisition to the clinical setting.
Study Design:
First-year pediatric residents with NRP training, but no previous neonatal experience, attended a 2-h intubation education session conducted by two experienced respiratory therapists. Individual components of the skill were taught, followed by practice on a high-fidelity infant mannequin with concurrent feedback. Skills were assessed using a validated neonatal intubation checklist (CL) and a five-point global rating scale (GRS), pre- and immediately post-intervention, using the mannequin. Clinical intubations performed in the subsequent 8-week neonatal intensive-care unit (NICU) rotation were evaluated by documenting success rates, time taken to intubate, and CL and GRS scores. Performance was also compared with similar data collected on intubations performed by a historical cohort of first-year residents who did not receive the training intervention. Data were analyzed using descriptive statistics, Student's t-test and χ2-test as appropriate, and analysis of variance.
Result:
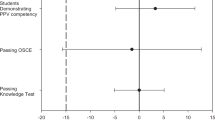
Thirteen residents participated in the educational session. Mean pre-intervention CL score was 65.4±18% (s.d.) and GRS was 3±0.7 (s.d.). Performance improved following the intervention with post-training CL score of 93±5% (P<0.0001) and GRS of 3.92±0.4 (P=0.0003). These trainees performed 40 intubations during their subsequent NICU rotation, with a success rate of 67.5% compared with 63.15% in the cohort group (NS). However, mean CL score for the study trainees during the NICU rotation was 64.6±20%, significantly lower than their post-training CL score (P<0.001), and significantly lower than the historical cohort score of 82.5±15.4% (P=0.001). In the intervention group, there were no significant differences between the pre-intervention and real-life CL scores of 65±18% and 64.63 %, respectively, and the pre-intervention and real-life GRS of 3.0±0.7 and 2.95±0.86, respectively.
Conclusion:
Trainees showed significant improvement in intubation skills immediately post intervention, but this did not translate into improved-clinical performance, with performance returning to baseline. In fact, significantly higher CL scores were demonstrated by the cohort group. These data suggest that improved performance in the simulation environment may not be transferable to the clinical setting. They also support the evidence that although concurrent feedback may lead to improved performance immediately post training intervention, this does not result in improved skill retention overall.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
de Oliveira Filho GR . The construction of learning curves for basic skills in anesthetic procedures: an application of the cumulative sum method. Anesth Analg 2002; 95 (2): 411–416.
Konrad C, Schüpfer GM, Gerber H . Learning manual skills in anesthesiology: is there a recommended number of cases for anesthetic procedures? Anesth Analg 1998; 86 (3): 635–639.
Leone TA, Rich W, Finer NN . Neonatal intubation: success of pediatric trainees. J Pediatr 2005; 146 (5): 638–641.
Falck AJ, Escobedo MB, Baillargeon JG, Villard LG, Gunkel JH . Proficiency of pediatric residents in performing neonatal endotracheal intubation. Pediatrics 2003; 112 (6 Part 1): 1242–1247.
O’Donnell CP, Kamlin CO, Davis PG, Morley CJ . Endotracheal intubation attempts during neonatal resuscitation: success rates, duration, and adverse effects. Pediatrics 2006; 117 (1): e16–e21.
Bismilla Z, Finan E, McNamara PJ, LeBlanc V, Jefferies A, Whyte H . Failure of paediatric and neonatal trainees to meet Canadian Neonatal Resuscitation Program standards for neonatal intubation. J Perinatol 2010; 30 (3): 182–187 (e-pub 2009 Oct 8).
Kattwinkel J . Textbook of Neonatal Resuscitation. 5th Ed American Academy of Pediatrics and American Heart Association: Elk Grove Village, IL, 2006.
Owen H, Plummer JL . Improving learning of a clinical skill: the first year's experience of teaching endotracheal intubation in a clinical simulation facility. Med Educ 2002; 36 (7): 635–642.
Goodwin MW, French GW . Simulation as a training and assessment tool in the management of failed intubation in obstetrics. Int J Obstet Anesth 2001; 10 (4): 273–277.
Nishisaki A, Donoghue AJ, Colborn S, Watson C, Meyer A, Brown III CA et al. Effect of just-in-time simulation training on tracheal intubation procedure safety in the pediatric intensive care unit. Anesthesiology 2010; 113 (1): 214–223.
Idzikowski C, Baddeley AD . Fear and dangerous environments In: R Hockey(ed). Stress and Fatigue in Human Performance. Wiley: Chichester, 1983, pp 123–144.
Schmidt RA, Wulf G . Continuous concurrent feedback degrades skill learning: implications for training and simulation. Hum Factors 1997; 39 (4): 509–525.
Xeroulis GJ, Park J, Moulton CA, Reznick RK, Leblanc V, Dubrowski A . Teaching suturing and knot-tying skills to medical students: a randomized controlled study comparing computer-based video instruction and (concurrent and summary) expert feedback. Surgery 2007; 141 (4): 442–449 (e-pub 2007 Jan 25).
Schmidt RA, Bjork RA . New conceptualizations of practice: Common principles in three paradigms suggest new concepts for training. Psychol Sci 1992; 3: 207–217.
Kirkpatrick DL . Evaluating Training Programs. 2nd ed Berrett Koehler: San Francisco, 1959.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Finan, E., Bismilla, Z., Campbell, C. et al. Improved procedural performance following a simulation training session may not be transferable to the clinical environment. J Perinatol 32, 539–544 (2012). https://doi.org/10.1038/jp.2011.141
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2011.141
Keywords
This article is cited by
-
Advanced neonatal procedural skills: a simulation-based workshop: impact and skill decay
BMC Medical Education (2023)
-
Predictors of successful treatment of respiratory distress with aerosolized calfactant
Journal of Perinatology (2023)
-
A tiny baby intubation team improves endotracheal intubation success rate but decreases residents’ training opportunities
Journal of Perinatology (2023)
-
Prevalence and severity of pediatric emergencies in a German helicopter emergency service: implications for training and service configuration
European Journal of Pediatrics (2023)
-
Standardisierte Handlungsanweisungen für (invasive) heilkundliche Maßnahmen durch Notfallsanitäter
Notfall + Rettungsmedizin (2020)