Abstract
Objective:
We evaluated electrical velocimetry, a noninvasive method for continuous cardiac output measurement, in very-low and low birth weight infants and the influence of patent ductus arteriosus (PDA) and ventilators on this method.
Study design:
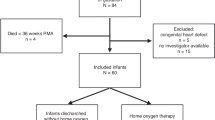
This prospective study compared 81 pairs of simultaneous cardiac output measurements by electrical velocimetry and transthoracic echocardiography in 28 patients. Data were compared by correlation, Bland–Altman analysis and two-way analysis of variance.
Results:
The two methods exhibited a high correlation (r=0.859, P<0.0001). The bias (mean difference of the methods) and percent error (100 × 1.96 × s.d./mean cardiac output) were −6 ml min−1 and 29.2%, respectively. PDA significantly affected the bias (P=0.0004), but ventilators did not (P=0.14). Hemodynamically significant PDA had a larger bias (−36 ml min−1) and higher percent error (38.6%).
Conclusions:
Although influenced by PDA, electrical velocimetry was generally interchangeable with transthoracic echocardiography even using ventilators.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Lobo SM, Lobo FR, Polachini CA, Patini DS, Yamamoto AE, de Oliveira NE et al. Prospective, randomized trial comparing fluids and dobutamine optimization of oxygen delivery in high-risk surgical patients [ISRCTN42445141]. Crit Care 2006; 10 (3): R72.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001; 345 (19): 1368–1377.
Pearse R, Dawson D, Fawcett J, Rhodes A, Grounds RM, Bennett ED . Early goal-directed therapy after major surgery reduces complications and duration of hospital stay. A randomised, controlled trial [ISRCTN38797445]. Crit Care 2005; 9 (6): R687–R693.
Fakler U, Ch Pauli, Balling G, Lorenz HP, Eicken A, Hennig M et al. Cardiac index monitoring by pulse contour analysis and thermodilution after pediatric cardiac surgery. J Thorac Cardiovasc Surg 2007; 133 (1): 224–228.
Raue W, Swierzy M, Koplin G, Schwenk W . Comparison of electrical velocimetry and transthoracic thermodilution technique for cardiac output assessment in critically ill patients. Eur J Anaesthesiol 2009; 26 (12): 1067–1071.
Osthaus WA, Huber D, Beck C, Winterhalter M, Boethig D, Wessel A et al. Comparison of electrical velocimetry and transpulmonary thermodilution for measuring cardiac output in piglets. Paediatr Anaesth 2007; 17 (8): 749–755.
Zoremba N, Bickenbach J, Krauss B, Rossaint R, Kuhlen R, Schälte G . Comparison of electrical velocimetry and thermodilution techniques for the measurement of cardiac output. Acta Anaesthesiol Scand 2007; 51 (10): 1314–1319.
Norozi K, Beck C, Osthaus WA, Wille I, Wessel A, Bertram H . Electrical velocimetry for measuring cardiac output in children with congenital heart disease. Br J Anaesth 2008; 100 (1): 88–94.
Schmidt C, Theilmeier G, Van Aken H, Korsmeier P, Wirtz SP, Berendes E et al. Comparison of electrical velocimetry and transoesophageal Doppler echocardiography for measuring stroke volume and cardiac output. Br J Anaesth 2005; 95 (5): 603–610.
Mertens L, Seri I, Marek J, Arlettaz R, Barker P, McNamara P et al. Targeted Neonatal Echocardiography in the Neonatal Intensive Care Unit: practice guidelines and recommendations for training. Writing Group of the American Society of Echocardiography (ASE) in collaboration with the European Association of Echocardiography (EAE) and the Association for European Pediatric Cardiologists (AEPC). J Am Soc Echocardiogr 2011; 24 (10): 1057–1078.
Raaijmakers E, Faes TJ, Scholten RJ, Goovaerts HG, Heethaar RM . A meta-analysis of three decades of validating thoracic impedance cardiography. Crit Care Med 1999; 27 (6): 1203–1213.
Critchley LA, Critchley JA . A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput 1999; 15 (2): 85–91.
Bland JM, Altman DG . Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1 (8476): 307–310.
Cecconi M, Rhodes A, Poloniecki J, Della Rocca G, Grounds RM . Bench-to-bedside review: the importance of the precision of the reference technique in method comparison studies -with specific reference to the measurement of cardiac output. Crit Care 2009; 13 (1): 201.
Mekis D, Kamenik M, Starc V, Jeretin S . Cardiac output measurements with electrical velocimetry in patients undergoing CABG surgery: a comparison with intermittent thermodilution. Eur J Anaesthesiol 2008; 25 (3): 237–242.
Grollmuss O, Demontoux S, Capderou A, Serraf A, Belli E . Electrical velocimetry as a tool for measuring cardiac output in small infants after heart surgery. Intensive Care Med 2012; 38 (6): 1032–1039.
Noori S, Drabu B, Soleymani S, Seri I . Continuous non-invasive cardiac output measurements in the neonate by electrical velocimetry: a comparison with echocardiography. Arch Dis Child Fetal Neonatal Ed 2012; 97 (5): F340–F343.
Tomaske M, Knirsch W, Kretschmar O, Woitzek K, Balmer C, Schmitz A et al. Cardiac output measurement in children: comparison of Aesculon cardiac output monitor and thermodilution. Br J Anaesth 2008; 100 (4): 517–520.
Futier E, Robin E, Jabaudon M, Guerin R, Petit A, Bazin JE et al. Central venous O2 saturation and venous-to-arterial CO2 difference as complementary tools for goal-directed therapy during high-risk surgery. Crit Care 2010; 14 (5): R193.
Vijlbrief DC, Benders MJ, Kemperman H, van Bel F, de Vries WB . Cardiac biomarkers as indicators of hemodynamic adaptation during postasphyxial hypothermia treatment. Neonatology 2012; 102 (4): 243–248.
Ehrenkranz RA, Younes N, Lemons JA, Fanaroff AA, Donovan EF, Wright LL et al. Longitudinal growth of hospitalized very low birth weight infants. Pediatrics 1999; 104 (2 Pt 1): 280–289.
Shaffer SG, Quimiro CL, Anderson JV, Hall RT . Postnatal weight changes in low birth weight infants. Pediatrics 1987; 79 (5): 702–705.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Torigoe, T., Sato, S., Nagayama, Y. et al. Influence of patent ductus arteriosus and ventilators on electrical velocimetry for measuring cardiac output in very-low/low birth weight infants. J Perinatol 35, 485–489 (2015). https://doi.org/10.1038/jp.2014.245
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2014.245
This article is cited by
-
Prediction of respiratory distress severity and bronchopulmonary dysplasia by lung ultrasounds and transthoracic electrical bioimpedance
European Journal of Pediatrics (2022)
-
Electrical cardiometry in monitoring percutaneous closure of ductus arteriosus in preterm infants: a case study on five patients
European Journal of Pediatrics (2022)
-
Accuracy and precision of non-invasive cardiac output monitoring by electrical cardiometry: a systematic review and meta-analysis
Journal of Clinical Monitoring and Computing (2020)
-
Electrical velocimetry for non-invasive monitoring of the closure of the ductus arteriosus in preterm infants
European Journal of Pediatrics (2018)
-
Thoracic fluid content by electric bioimpedance correlates with respiratory distress in newborns
Journal of Perinatology (2017)