Abstract
Objective:
Birth is less safe than it can be. We adapted the UK-developed PROMPT™ (PRactical Obstetric Multi-Professional Training) course to local practices and initiated annual training.
Study Design:
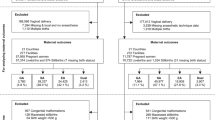
This observational study used quality assurance data from University of Kansas Hospital 2 years before and 7 years after intervention encompassing 14 309 consecutive deliveries from January 2006 through December 2014. An events/trials approach was applied to changes in proportions over time.
Result:
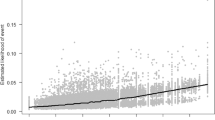
PROMPT™ was associated with progressive decreases in rates (P<0.05) of brachial plexus injury and umbilical artery pH <7.00 exclusive of catastrophic events. Reduced rates (P<0.05) of cesarean section, episiotomy and higher perception of nurse/physician communication were documented. Hypoxic ischemic encephalopathy (HIE) rates declined progressively by >50% (P=NS). These improvements occurred despite younger faculty and higher rates of complicated pregnancies (P<0.05). Estimated health-care costs avoided exceeded annual training costs.
Conclusion:
Local annual multi-professional training as provided by PROMPT™ was temporally associated with improved obstetric outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Siassakos D, Crofts JF, Winter C, Weiner CP, Draycott TJ . The active components of effective training in obstetric emergencies. BJOG 2009; 116: 1028–1032.
Walker LJ, Fetherston CM, McMurray A . Perceived changes in the knowledge and confidence of doctors and midwives to manage obstetric emergencies following completion of an Advanced Life Support in Obstetrics course in Australia. Aust NZ J Obstet Gynaecol 2013; 53: 525–531.
Woiski MD, Hermens RP, Middeldorp JM, Kremer JA, Marcus MA, Wouters MG et al. Haemorrhagia post partum; an implementation study on the evidence-based guideline of the Dutch Society of Obstetrics and Gynaecology (NVOG) and the MOET (Managing Obstetric Emergencies and Trauma-course) instructions; the Fluxim study. BMC Pregnancy Childbirth 2010; 10: 5.
Gardner R, Walzer TB, Simon R, Raemer DB . Obstetric simulation as a risk control strategy: course design and evaluation. Simul Healthc 2008; 3: 119–127.
Thanh NX, Jacobs P, Wanke MI, Hense A, Sauve R . Outcomes of the introduction of the MOREOB continuing education program in Alberta. J Obstet Gynaecol Can 2010; 32: 749–755.
Robertson B, Schumacher L, Gosman G, Kanfer R, Kelley M, DeVita M . Simulation-based crisis team training for multidisciplinary obstetric providers. Simul Healthc 2009; 4: 77–83.
MacEachin SR, Lopez CM, Powell KJ, Corbett NL . The fetal heart rate collaborative practice project: situational awareness in electronic fetal monitoring-a Kaiser Permanente Perinatal Patient Safety Program Initiative. J Perinat Neonatal Nurs 2009; 23: 314–323.
Sørensen JL, Løkkegaard E, Johansen M, Ringsted C, Kreiner S, McAleer S . The implementation and evaluation of a mandatory multi-professional obstetric skills training program. Acta Obstet Gynecol Scand 2009; 88: 1107–1117.
Inglis SR, Feier N, Chetiyaar JB, Naylor MH, Sumersille M, Cervellione KL et al. Effects of shoulder dystocia training on the incidence of brachial plexus injury. Am J Obstet Gynecol 2011; 204: 322. e1–6.
MacKenzie IZ, Shah M, Lean K, Dutton S, Newdick H, Tucker DE . Management of shoulder dystocia: trends in incidence and maternal and neonatal morbidity. Obstet Gynecol 2007; 110: 1059–1068.
Nielsen PE, Goldman MB, Mann S, Shapiro DE, Marcus RG, Pratt SD et al. Effects of teamwork training on adverse outcomes and process of care in labor and delivery: a randomized controlled trial. Obstet Gynecol 2007; 109: 48–55.
Phipps MG, Lindquist DG, McConaughey E, O'Brien JA, Raker CA, Paglia MJ . Outcomes from a labor and delivery team-training program with simulation component. Am J Obstet Gynecol 2012; 206: 3–9.
Wagner B, Meirowitz N, Shah J, Nanda D, Reggio L, Cohen P et al. Comprehensive perinatal safety initiative to reduce adverse obstetric events. J Healthc Qual 2012; 34: 6–15.
Collins K, Draycott TJ, Crofts JF, Siassakos D, Winter C, Weiner CP et al. Myths and realities of training for obstetric emergencies. Best Pract Res Clin Obstet Gynecol 2015; S1521-6934 (15): 00127–00310.
Crofts JF, Ellis D, Draycott TJ, Winter C, Hunt LP, Akande VA . Change in knowledge of midwives and obstetricians following obstetric emergency training: a randomised controlled trial of local hospital, simulation centre and teamwork training. BJOG 2007; 114: 1534–1541.
Crofts JF, Fox R, Draycott TJ, Winter C, Hunt LP, Akande VA . Retention of factual knowledge after practical training for intrapartum emergencies. Int J Gynaecol Obstet 2013; 123: 83–85.
Ellis D, Crofts JF, Hunt LP, Read M, Fox R, James M . Hospital, simulation center, and teamwork training for eclampsia management: a randomized controlled trial. Obstet Gynecol 2008; 111: 723–731.
Crofts JF, Bartlett C, Ellis D, Hunt LP, Fox R, Draycott TJ . Management of shoulder dystocia: skill retention 6 and 12 months after training. Obstet Gynecol 2007; 110: 1069–1074.
Draycott T, Sibanda T, Owen L, Akande V, Winter C, Reading S et al. Does training in obstetric emergencies improve neonatal outcome? BJOG 2006; 113: 177–182.
Draycott TJ, Crofts JF, Ash JP, Wilson LV, Yard E, Sibanda T et al. Improving neonatal outcome through practical shoulder dystocia training. Obstet Gynecol 2008; 112: 14–20.
Siassakos D, Hasafa Z, Sibanda T, Fox R, Donald F, Winter C et al. Retrospective cohort study of diagnosis-delivery interval with umbilical cord prolapse: the effect of team training. BJOG 2009; 116: 1089–1096.
Use and abuse of the APGAR score. Committee on fetus and Newborn, American Academy of Pediatrics, and Committee on Obstetric Practice, American College of Obstetrics and Gynecology. Pediatrics 1996; 98: 141–142.
US Agency for Healthcare Research and Quality, HCUPnet, Healthcare Cost and Utilization Project. Rockville, MD: AHRQ. Available at http://hcupnet.ahrq.gov/.
Centers for Disease Control and Prevention. Economic costs associated with mental retardation, cerebral palsy, hearing loss, and vision impairment—United States, 2003. MMWR Morb Mortal Wkly Rep 2004; 53: 57–59.
Grobman W . Shoulder dystocia. Obstet Gynecol Clin North Am 2013; 40: 59–67.
Ouyang L, Grosse SD, Armour BS, Waitzman NJ . Health care expenditures of children and adults with spina bifida in a privately insured U.S. population. Birth Defects Res A Clin Mol Teratol 2007; 79: 552–558.
Shoushtarian M, Barnett M, McMahon F, Ferris J . Impact of introducing Practical Obstetric Multi-Professional Training (PROMPT) into Maternity Units in Victoria, Australia. BJOG 2014; 121: 1710–1718.
Thorngren-Jerneck K, Herbst A . Low 5-minute Apgar score: a population-based register study of 1 million term births. Obstet Gynecol 2001; 98: 65–70.
NHSLA Report – An analysis of NHS Litigation, October 2012.
Stead K, Kumar S, Schultz TJ, Tiver S, Pirone CJ, Adams RJ et al. Teams communicating through STEPPS. Med J Aust 2009; 190 (11 Suppl): S128–S132.
Acknowledgements
We are grateful to all the obstetrical staff who have annually contributed their time to PROMPT and the University of Kansas Hospital leadership for their public and financial support of PROMPT. We wish to thank Dr Prabhu Parimi, Professor and Division Head of Neonatology at the University of Kansas, for reviewing each patient with a diagnosis of HIE. Finally, we thank the team at PROMPT Maternity, Bristol, UK, a registered UK charity for all of their assistance over the last decade. This project was a product of annual Quality Assessment activities conducted by the University of Kansas Hospital. Quality Assessment activities such as these are generally considered exempt from Human Subjects Committee approval.
Author contributions
CPW directs the PROMPT™ program at the University of Kansas Hospital. He conceived of the study and is the primary author of the manuscript. He was intentionally excluded from data collection and analyses. LC is the Nurse Manager of the University of Kansas Labor Suite. She participated in data collection, and has read, edited and approved the content of the final manuscript. SB is a nurse midwife who was responsible for the Quality Assessment of obstetrics at the University of Kansas Hospital. She participated in data collection, and read, edited and approved the content of the final manuscript. YD is the Division Director of Research at the University of Kansas. He offered suggestions on the approach taken, and read, edited and approved the content of the final manuscript. CLS is a faculty member in the Department of Preventative Medicine at the University of Kansas. She performed all the statistical analyses, provided interpretation of the results, and read, edited and approved the content of the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Weiner has directed without compensation PROMPT™ North America, a licensee of PROMPT Maternity, providing postgraduate multi-professional training to hospitals in the United States for obstetrical emergencies since April 2013. He has received less than $5000 per year serving as an instructor for PROMPT™ Train the Trainer courses.
Additional information
This study was presented in part and the recipient of the Prize Paper, Best Clinical Presentation at the 2014 annual meeting of the Society for Maternal Fetal Medicine.
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Weiner, C., Collins, L., Bentley, S. et al. Multi-professional training for obstetric emergencies in a US hospital over a 7-year interval: an observational study. J Perinatol 36, 19–24 (2016). https://doi.org/10.1038/jp.2015.136
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2015.136
This article is cited by
-
A systematic review of brachial plexus injuries after caesarean birth: challenging delivery?
BMC Pregnancy and Childbirth (2023)
-
Interdisziplinäre Trainingsprogramme in der Geburtshilfe
Die Gynäkologie (2023)
-
THISTLE: trial of hands-on Interprofessional simulation training for local emergencies: a research protocol for a stepped-wedge clustered randomised controlled trial
BMC Pregnancy and Childbirth (2017)