Abstract
Objective:
The automated reticulocyte parameters (absolute reticulocyte count, immature reticulocyte fraction (IRF) and reticulocyte hemoglobin content (RET-He)) are of value in managing adults and older children with a variety of hematological disorders. However, the lack of reference intervals for these parameters in neonates and young infants has limited their application to that population.
Study Design:
During a span of 12 months (29 May 2014 to 5 May 2015), a convenience sample of reticulocyte parameters were run from clinically ordered complete blood counts (CBCs) of infants within the first 90 days after birth. Measuring the reticulocyte parameters as a research-only adjunct to the CBC did not require any additional blood or generate a patient charge, and the reticulocyte results were not reported to the provided and did not appear in the clinical records. Values from neonates who had a transfusion or a diagnosis of anemia were subsequently excluded from the reference data set.
Results:
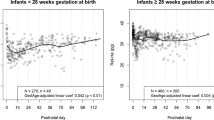
Nine Intermountain Healthcare clinical laboratories contributed 8438 CBCs to the initial reticulocyte parameter database. From these, 1806 were excluded because of a transfusion or a diagnosis of anemia, leaving 6632 in the reference interval database. The parameters charted over the first 90 days after birth were: (1) blood hemoglobin concentration (g dl−1), (2) mean corpuscular volume (fL), (3) reticulocyte count (x103 per μl), (4) IRF (%) and (5) RET-He (pg).
Conclusions:
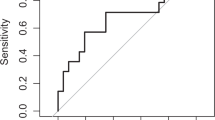
The new reference interval charts can help clinicians identify abnormalities in the reticulocyte parameters. This information could be of value in identifying and following neonates with various hematological problems including hemolytic disorders, occult hemorrhage, or iron deficiency or other limitations of erythrocyte production.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Christensen RD, Henry E, Jopling J, Wiedmeier SE . The CBC: reference ranges for neonates. Semin Perinatol 2009; 33 (1): 3–11.
Henry E, Christensen RD . Reference intervals in neonatal hematology. Clin Perinatol 2015; 42 (3): 483–497.
Al-Ghananim R, Nalbant D, Schmidt RL, Cress GA, Zimmerman MB, Widness JA . Reticulocyte hemoglobin content during the first month of life in critically ill very low birth weight neonates differs from term infants, children, and adults. J Clin Lab Anal 2015; 29: 1–9.
Lorenz L, Peter A, Poets CF, Franz AR . A review of cord blood concentrations of iron status parameters to define reference ranges for preterm infants. Neonatology 2013; 104 (3): 194–202.
Mäkelä E, Takala TI, Suominen P, Matomäki J, Salmi TT, Rajamäki A et al. Hematological parameters in preterm infants from birth to 16 weeks of age with reference to iron balance. Clin Chem Lab Med 2008; 46 (4): 551–557.
Schiza V, Giapros V, Pantou K, Theocharis P, Challa A, Andronikou S . Serum transferrin receptor, ferritin, and reticulocyte maturity indices during the first year of life in 'large' preterm infants. Eur J Haematol 2007; 79 (5): 439–446.
Christensen RD, Yaish HM, Henry E, Bennett ST . Red blood cell distribution width: reference intervals for neonates. J Matern Fetal Neonatal Med 2014; 17: 1–6.
Christensen RD, Henry E, Andres RL, Bennett ST . Reference ranges for blood concentrations of nucleated red blood cells in neonates. Neonatology 2011; 99 (4): 289–294.
Jopling J, Henry E, Wiedmeier SE, Christensen RD . Reference ranges for hematocrit and blood hemoglobin concentration during the neonatal period: data from a multihospital health care system. Pediatrics 2009; 123 (2): e333–e337.
Christensen RD, Jopling J, Henry E, Wiedmeier SE . The erythrocyte indices of neonates, defined using data from over 12,000 patients in a multihospital health care system. J Perinatol 2008; 28 (1): 24–28.
Piva E, Brugnara C, Spolaore F, Plebani M . Clinical utility of reticulocyte parameters. Clin Lab Med 2015; 35 (1): 133–163.
Wong EC . Hematology analyzers: special considerations for pediatric patients. Clin Lab Med 2015; 35 (1): 165–181.
Zaizov R, Matoth Y . Red cell values on the first postnatal day during the last 16 weeks of gestation. Am J Hematol 1976; 1 (2): 275–278.
Stockman JA 3rd, Oski FA . RBC values in low-birth-weight infants during the first seven weeks of life. Am J Dis Child 1980; 134 (10): 945–946.
Kling PJ, Schmidt RL, Roberts RA, Widness JA . Serum erythropoietin levels during infancy: associations with erythropoiesis. J Pediatr 1996; 128 (6): 791–796.
Saleh MI, Nalbant D, Widness JA, Veng-Pedersen P . Population pharmacodynamic analysis of erythropoiesis in preterm infants for determining the anemia treatment potential of erythropoietin. Am J Physiol Regul Integr Comp Physiol 2013; 304 (9): R772–R781.
Maisels MJ, Kring E . The contribution of hemolysis to early jaundice in normal newborns. Pediatrics 2006; 118: 276–279.
Christensen RD, Lambert DK, Henry E, Yaish HM, Prchal JT . End-tidal carbon monoxide as an indicator of the hemolytic rate. Blood Cells Mol Dis 2015; 54 (3): 292–296.
Song J, Yoon D, Christensen RD, Horvathova M, Thiagarajan P, Prchal JT . HIF mediates increased ROS from reduced mitophagy and decreased catalase causes neocytolysis. J Molecular Med 2015; 93 (8): 857–866.
Perrone S, Tataranno ML, Stazzoni G, Del Vecchio A, Buonocore G . Oxidative injury in neonatal erythrocytes. J Matern Fetal Neonatal Med 2012; 25 (Suppl 5): 104–108.
Kasper DC, Widness JA, Haiden N, Berger A, Hayde M, Pollak A et al. Characterization and differentiation of iron status in anemic very low birth weight infants using a diagnostic nomogram. Neonatology 2009; 95 (2): 164–171.
Christensen RD . Reference ranges in neonatal hematology In: deAlarcon PA, Werner EJ, Christensen RD (eds). Neonatal Hematology, 2nd edn. Cambridge University Press: Cambridge UK, 2013, pp 385–391.
Janus J, Moerschel SK . Evaluation of anemia in children. Am Fam Physician 2010; 81 (12): 1462–147.
Urrechaga E, Borque L, Escanero JF . Erythrocyte and reticulocyte indices in the assessment of erythropoiesis activity and iron availability. Int J Lab Hematol 2013; 35 (2): 144–149.
Watanabe K, Kawai Y, Takeuchi K, Shimizu N, Iri H, Ikeda Y et al. Reticulocyte maturity as an indicator for estimating qualitative abnormality of erythropoiesis. Clin Pathol 1994; 47: 736–739.
Bukhari KT, Zafar H . Reference values of reticulocyte counts in five age groups of healthy infants at Rawalpindi, Pakistan. J Pak Med Assoc 2013; 63 (9): 1108–1111.
Torsvik IK, Markestad T, Ueland PM, Nilsen RM, Midttun O, Bjørke Monsen AL . Evaluating iron status and the risk of anemia in young infants using erythrocyte parameters. Pediatr Res 2013; 73 (2): 214–220.
Brugnara C, Schiller B, Moran J . Reticulocyte hemoglobin equivalent (Ret He) and assessment of iron-deficient states. Clin Lab Haematol 2006; 28 (5): 303–308.
Acknowledgements
We thank Dr Jolanta Kunicka, Elizabeth Wiet and Lance Kocherhans of the Sysmex America, and Dr Larry D Eggert, Intermountain Healthcare, for helpful discussions; Diane K Lambert, RN, Intermountain Healthcare, for assistance with IRB communications and laboratory staff members Robert Childs, Dereck Daniels, Rachael Ethington, Lauri Jeffs, Jennessa Jessop, Heather Kuusela, Chris Partington, Brooke Qi, Lauralyn Ragin, Aba Saunders, Alicia Simon, Thomas Taylor and Ashley Windsor for extracting data from the hematology analyzers. The study was supported by a research grant from Intermountain Research and Medical Foundation, Murray, Utah, 84157, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Christensen, R., Henry, E., Bennett, S. et al. Reference intervals for reticulocyte parameters of infants during their first 90 days after birth. J Perinatol 36, 61–66 (2016). https://doi.org/10.1038/jp.2015.140
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2015.140
This article is cited by
-
A “Gold Standard” Test for Diagnosing and Quantifying Hemolysis in Neonates and Infants
Journal of Perinatology (2023)
-
Hyperferritinemia among very-low-birthweight infants in Thailand: a prospective cohort study
Journal of Perinatology (2023)
-
Neonatal hematological parameters: the translational aspect of developmental hematopoiesis
Annals of Hematology (2023)
-
Serum ferritin values in neonates <29 weeks’ gestation are highly variable and do not correlate with reticulocyte hemoglobin content
Journal of Perinatology (2023)
-
The Reference Intervals of Whole Blood Copper, Zinc, Calcium, Magnesium, and Iron in Infants Under 1 Year Old
Biological Trace Element Research (2022)