Abstract
Objective:
To compare the failure rates between Jet continuous positive airway pressure device (J-CPAP-variable flow) and Bubble continuous positive airway device (B-CPAP) in preterm infants with respiratory distress.
Study design:
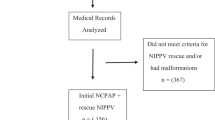
Preterm newborns <34 weeks gestation with onset of respiratory distress within 6 h of life were randomized to receive J-CPAP (a variable flow device) or B-CPAP (continuous flow device). A standardized protocol was followed for titration, weaning and removal of CPAP. Pressure was monitored close to the nares in both the devices every 6 hours and settings were adjusted to provide desired CPAP. The primary outcome was CPAP failure rate within 72 h of life. Secondary outcomes were CPAP failure within 7 days of life, need for surfactant post-randomization, time to CPAP failure, duration of CPAP and complications of prematurity. An intention to treat analysis was done.
Results:
One-hundred seventy neonates were randomized, 80 to J-CPAP and 90 to B-CPAP. CPAP failure rates within 72 h were similar in infants who received J-CPAP and in those who received B-CPAP (29 versus 21%; relative risks 1.4 (0.8 to 2.3), P=0.25). Mean (95% confidence intervals) time to CPAP failure was 59 h (54 to 64) in the Jet CPAP group in comparison with 65 h (62 to 68) in the Bubble CPAP group (log rank P=0.19). All other secondary outcomes were similar between the two groups.
Conclusion:
In preterm infants with respiratory distress starting within 6 h of life, CPAP failure rates were similar with Jet CPAP and Bubble CPAP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Gregory GA, Kitterman JA, Phibbs RH, Tooley WH, Hamilton WK . Treatment of the idiopathic respiratory-distress syndrome with continuous positive airway pressure. N Engl J Med. 1971; 284 (24): 1333–1340.
Finer NN, Carlo WA, Walsh MC, Rich W, Gantz MG, Laptook AR et al. Early CPAP versus surfactant in extremely preterm infants. N Engl J Med 2010; 362 (21): 1970–1979.
Dunn MS, Kaempf J, de Klerk A, de Klerk R, Reilly M, Howard D et al. Randomized trial comparing 3 approaches to the initial respiratory management of preterm neonates. Pediatrics 2011; 128 (5): e1069–e1076.
De Paoli AG, Davis PG, Faber B, Morley CJ . Devices and pressure sources for administration of nasal continuous positive airway pressure (NCPAP) in preterm neonates. Cochrane Database Syst Rev. 2008, Issue 1. Art No.: CD002977. doi:10.1002/14651858.CD002977.pub2.
Benveniste D, Pedersen JE . A valve substitute with no moving parts, for artificial ventilation in newborn and small infants. Br J Anaesth 1968; 40 (6): 464–470.
Theilade D . Nasal CPAP employing a jet device for creating positive pressure. Intensive Care Med 1978; 4 (3): 145–148.
Klausner JF, Lee AY, Hutchison AA . Decreased imposed work with a new nasal continuous positive airway pressure device. Pediatr Pulmonol 1996; 22 (3): 188–194.
Pandit PB, Courtney SE, Pyon KH, Saslow JG, Habib RH . Work of breathing during constant- and variable-flow nasal continuous positive airway pressure in preterm neonates. Pediatrics 2001; 108 (3): 682–685.
Mazzella M, Bellini C, Calevo MG, Campone F, Massocco D, Mezzano P et al. A randomised control study comparing the Infant Flow Driver with nasal continuous positive airway pressure in preterm infants. Arch Dis Child Fetal Neonatal Ed 2001; 85 (2): F86–F90.
Liptsen E, Aghai ZH, Pyon KH, Saslow JG, Nakhla T, Long J et al. Work of breathing during nasal continuous positive airway pressure in preterm infants: a comparison of bubble vs variable-flow devices. J Perinatol. 2005; 25 (7): 453–458.
Ahluwalia JS, White DK, Morley CJ . Infant Flow Driver or single prong nasal continuous positive airway pressure: short-term physiological effects. Acta Paediatr 1998; 87 (3): 325–327.
Wald M, Kribs A, Jeitler V, Lirsch D, Pollak A, Kirchner L . Variety of expiratory resistance between different continuous positive airway pressure devices for preterm infants. Artif Organs 2011; 35 (1): 22–28.
Bober K, Swietlinski J, Zejda J, Kornacka K, Pawlik D, Behrendt J et al. A multicenter randomized controlled trial comparing effectiveness of two nasal continuous positive airway pressure devices in very low birth weight infants. Pediatr Crit Care Med 2012; 13: 191–196.
Jaile JC, Levin T, Wung JT, Abramson SJ, Ruzal-Shapiro C, Berdon WE . Benign gaseous distension of the bowel in premature infants treated with nasal continuous airway pressure: a study of contributing factors. AJR Am J Roentgenol 1992; 158 (1): 125–127.
Richardson DK, Corcoran JD, Escobar GJ, Lee SK . SNAP-II and SNAPPE-II: simplified newborn illness severity and mortality risk scores. J Pediatr 2001; 138 (1): 92–100.
Downes JJ, Vidyasagar D, Boggs TR Jr, Morrow GM 3rd . Respiratory distress syndrome of newborn infants. I. New clinical scoring system (RDS score) with acid-base and blood-gas correlations. Clin Pediatr (Phila) 1970; 9: 325–331.
Gupta S, Sinha SK, Tin W, Donn SM . A randomized controlled trial of post-extubation bubble continuous positive airway pressure versus Infant Flow Driver continuous positive airway pressure in preterm infants with respiratory distress syndrome. J Pediatr 2009; 154 (5): 645–650.
Koti J, Murki S, Gaddam P, Reddy A, Reddy MD . Bubble CPAP for respiratory distress syndrome in preterm infants. Indian Pediatr 2010; 47 (2): 139–143.
Yagui AC, Vale LA, Haddad LB, Prado C, Rossi FS, Deutsch AD et al. Bubble CPAP versus CPAP with variable flow in newborns with respiratory distress: a randomized controlled trial. J Pediatr (Rio J) 2011; 87 (6): 499–504.
Stefanescu B, Murphy WP, Hansell BJ, Fuloria M, Morgan TM, Aschner JL . A randomized, controlled trial comparing two different continuous positive airway pressure systems for the successful extubation of extremely low birth weight infants. Pediatrics 2003; 112: 1031–1038.
Pillow JJ, Travadi JN . Bubble CPAP: is the noise important? An in vitro study. Pediatr Res 2005; 57 (6): 826–830.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bhatti, A., Khan, J., Murki, S. et al. Nasal Jet-CPAP (variable flow) versus Bubble-CPAP in preterm infants with respiratory distress: an open label, randomized controlled trial. J Perinatol 35, 935–940 (2015). https://doi.org/10.1038/jp.2015.98
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2015.98
This article is cited by
-
Systematic rotation versus continuous application of ‘nasal prongs’ or ‘nasal mask’ in preterm infants on nCPAP: a randomized controlled trial
European Journal of Pediatrics (2023)
-
Noninvasive Respiratory Support in Neonates: A Review of Current Evidence and Practices
Indian Journal of Pediatrics (2021)
-
Predictors of CPAP Failure – 10 years’ Data of Multiple Trials from a Single Center: A Retrospective Observational Study
The Indian Journal of Pediatrics (2020)
-
Nasal injury and comfort with jet versus bubble continuous positive airway pressure delivery systems in preterm infants with respiratory distress
European Journal of Pediatrics (2017)