Abstract
Objective:
Vitamin D deficiency is associated with asthma and reactive airway disease in childhood but its potential contribution to bronchopulmonary dysplasia (BPD) in preterm infants is unknown. Preterm infants have lower levels of 25-hydroxyvitamin D (25(OH)D) at birth and are at risk for nutritional deficiencies after birth. The objective of the study was to evaluate the association of 25(OH)D concentrations at birth and at 36 weeks’ corrected gestational age with BPD in preterm infants born before 29 completed weeks of gestation.
Study Design:
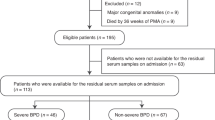
We collected umbilical cord blood samples from 44 preterm infants (gestational age <29 weeks) delivered at Brigham and Women’s Hospital in Boston. In addition, with parental consent we collected venous samples at 36 weeks’ corrected age from 20 preterm infants born before 29 weeks’ gestation (including 6 infants with previously collected cord blood). Samples were frozen at −80 °C until subsequent measurement of 25(OH)D levels by chemiluminescence. We used multivariable logistic models to adjust for gestational age and considered other confounding variables, including maternal race, age, mode of delivery and infant sex.
Results:
Among 44 infants, 41 (93.2%) survived and 3 (6.8%) died before 36 weeks’ corrected age. Median 25(OH)D levels at birth were 30.4 ng ml−1 in preterm infants who subsequently died or developed BPD and 33.8 ng ml−1 in infants who survived without BPD (P=0.6). Median 25(OH)D levels at corrected age of 36 weeks were 59.0 ng ml−1 among survivors without BPD and 64.2 ng ml−1 among survivors with BPD (P=0.9). Neither cord blood nor 36 weeks’ corrected 25(OH)D levels were associated with odds of death or BPD (adjusted odds ratio (OR) 1.00, 95% confidence interval (CI): 0.73 to 1.37; and OR 0.93, 95% CI: 0.61 to 1.43, respectively).
Conclusions:
Among this population of extremely preterm infants neither cord blood nor the 36 weeks’ corrected age 25(OH)D levels were associated with development of BPD. Notably, at the current level of supplementation, all extremely preterm infants in our cohort had achieved 25(OH)D levels >30 ng ml−1 by 36 weeks’ corrected age, which is thought to represent sufficiency in adult and pediatric populations.
Similar content being viewed by others
Introduction
Bronchopulmonary dysplasia (BPD) is the most prevalent long-term morbidity among surviving extremely preterm infants and has a multifactorial etiology.1 BPD is associated with later risk of reactive airways disease, such as asthma,2 post neonatal mortality and adverse neurodevelopmental outcomes.1 BPD affects ~20% of preterm infants, and up to 60% of extremely preterm infants who are born before 26 completed weeks of gestation.2 An estimated 10 000 to 15 000 infants are affected in the United States each year and this has substantial medical and socioeconomic implications.2, 3
Accumulating epidemiologic evidence suggests that vitamin D deficiency or insufficiency is associated with respiratory disease in children. Camargo et al.4 demonstrated that lower maternal intake of vitamin D during pregnancy is associated with recurrent wheezing and asthma in their offspring during early childhood. Brehm et al.5, 6 showed that asthma symptoms are more severe among children with lower serum 25D levels and this effect was independent of race. Some features of BPD, including clinical signs (for example, respiratory distress and wheezing), radiographic findings (for example, hyperinflation) and pathology (for example, excessive airway muscularization), share similarities with asthma. In addition, animal studies support the hypothesis that vitamin D status might affect the risk of BPD given that both vitamin D and the vitamin D receptor (VDR) have important roles in perinatal lung development.7, 8 Thus, we speculated that vitamin D deficiency might predispose to and/or have a role in the pathogenesis of BPD. In addition, preterm infants are at high risk for nutritional deficiencies.9 Specifically, we previously reported in a cohort of 471 newborn infants, that preterm birth before 32 completed weeks of gestation is an independent risk factor for low 25-hydroxyvitamin D (25(OH)D) levels at birth.10 In this study we sought to evaluate whether there is an association between 25(OH)D concentrations at birth and at 36 weeks’ corrected gestational age with BPD in preterm infants born before 29 completed weeks of gestation. In addition, we evaluated whether the current practice of providing 400 IU per day 25(OH)D is sufficient to achieve adequate serum levels (>30 ng ml−1) at 36 weeks’ corrected age.
Methods
Vitamin D analysis
We conducted a prospective observational study with institutional review board approval at Brigham and Women’s Hospital. We collected umbilical cord blood at the time of delivery from 44 extremely preterm infants (<29 weeks of gestation) born at Brigham and Women’s Hospital, a high-risk tertiary care center in Boston, Massachusetts, between 2010 and 2013. These samples were collected under a ‘discarded materials and medical record review’ protocol with a waiver of parental consent. Thirty-four of these samples were included in our prior publication of cord blood levels and their relationship to gestational age10 but their clinical outcomes were not previously reported. In addition, with written parental consent, we obtained venous blood samples at ~36 weeks’ corrected gestational age at the time of a medically indicated blood draw from 20 infants also born before 29 completed weeks of gestation. There were 6 subjects for which we had both cord blood and venous blood at 36 weeks. We refrigerated and centrifuged the blood samples and stored plasma aliquots at −80 °C. We measured 25(OH)D levels, a combination of 25(OH)D2 and 25(OH)D3, which represent the best analytes for overall vitamin D status11 using DiaSorin Liaison (DiaSorin, Stillwater, MN, USA), which uses a chemiluminescence immunoassay12 to determine plasma concentrations of 25(OH)D. For quality control, the laboratory used the US National Institute of Standards and Technology level 1. Interassay coefficient of variation was 9.6%. We report 25(OH)D levels in ng ml−1, which can be multiplied by 2.496 to convert to nmol l−1.
Clinical and demographic data ascertainment
We extracted clinical outcome and demographic data from the medical records. We calculated gestational age in weeks at birth based on the best obstetrical estimate using the date of last menstrual period with confirming first trimester ultrasounds. Primary outcome was a composite of death or BPD (defined as oxygen use at 36 weeks’ corrected age). As there is no agreement on the best definition of BPD in the literature,13, 14 we also collected information on respiratory support in the first 28 days of life in order to re-analyze our data using the National Institutes of Health consensus definition of BPD.15 We collected information on potential confounding variables, including antenatal steroid exposure, surfactant administration and need for any respiratory support. Additional clinical outcomes included culture-proven sepsis, necrotizing enterocolitis, retinopathy of prematurity, intraventricular hemorrhage and periventricular leukomalacia. We collected cord blood samples from 44 preterm infants, and venous blood at 36 weeks’ corrected age from a separate group of 20 preterm infants. There were a total of 6 subjects for whom we collected both, cord blood and venous blood and measured 25(OH)D levels.
Statistical analyses
We used generalized estimated equations for the comparison of the 25(OH)D levels between the cord blood samples and the venous samples at 36 weeks’ corrected age to appropriately control for infants who had blood at both time points. We used Wilcoxon rank sum test to compare 25(OH)D levels between infants with the composite outcome of BPD or death and infants who survived without BPD. Logistic regression models using generalized estimating equations to cluster by mother among multiples were used to evaluate the association between 25(OH)D and odds of death or BPD. The odds ratio for death or BPD was calculated per every 10 ng ml−1 increment of 25(OH)D at birth and at 36 weeks’ gestational age in unadjusted and adjusted for gestational age models. We performed all analyses using SAS 9.3 (Cary, NC, USA).
Results
Demographic information is shown in Table 1. We had 44 subjects born before 29 completed weeks of gestation who had cord blood levels of 25(OH)D measured, and 20 who had their 25(OH)D levels measured at 36 weeks’ corrected age. There were no significant differences in birth characteristics (gestational age, birth weight, sex, ethnicity and mode of delivery) between our two cohorts. Levels of 25(OH)D were significantly higher at 36 weeks’ corrected age compared with cord blood levels (median (interquartile range): 61.6 (53.2 to 78.8) vs 31.4 (22.0 to 38.3) ng ml−1). We found that 45% (20/44) of infants had levels of 25(OH)D under 30 ng ml−1, and 18% (8/44) had levels of 25(OH)D under 20 ng ml−1 at birth while all infants at 36 weeks’ corrected age had 25(OH)D levels above 30 ng ml−1 (Table 1).
Among 44 infants born before 29 weeks, 23 infants (52%) survived without BPD, 3 (7%) died and 18 (41%) developed BPD. As shown in Table 2, median 25(OH)D levels at birth were 30.4 ng ml−1 in preterm infants who subsequently died or developed BPD and 33.8 ng ml−1 in infants who survived without BPD, and there were no statistically significant differences in 25(OH)D cord blood levels between these two groups (P=0.6). Cord blood levels of 25(OH)D <20 or <30 ng ml−1 were not associated with the outcome of death or BPD (Table 3). Among the 20 infants born before 29 weeks for which a blood sample at 36 weeks’ corrected age was analyzed, 13 infants (65%) had BPD and 7 (35%) did not. Median 25(OH)D levels at corrected age of 36 weeks were 59.0 ng ml−1 among survivors without BPD and 64.2 ng ml−1 among survivors with BPD (P=0.9) (Table 2).
Logistic regression analysis (adjusted for gestational age) showed no significant associations between 25(OH)D levels at birth and at 36 weeks and the odds of BPD or death (odds ratio 1.00, 95% confidence interval: 0.73 to 1.37; and odds ratio 0.93, 95% confidence interval: 0.61 to 1.43, respectively) per 10 ng ml−1 increment of 25(OH)D (Table 3).
In addition, we re-analyzed our data using the National Institutes of Health consensus definition of BPD and found similar results (data not shown).
Other morbidities of prematurity, including culture-proven sepsis, necrotizing enterocolitis, retinopathy of prematurity, intraventricular hemorrhage and periventricular leukomalacia were not associated with cord blood or 36 weeks’ corrected age 25(OH)D levels in our study cohort (Table 1).
Discussion
In this prospective study of cord blood 25(OH)D levels, we found that although a large percentage (45%) of preterm infants born before 29 weeks of gestation had cord blood plasma 25(OH)D levels under 30 ng ml−1, cord blood 25(OH)D levels were not associated with the odds of death or BPD. Nor were cord blood 25(OH)D levels predictive of other common morbidities of prematurity. Moreover, with current supplementation practices, levels of 25(OH)D are significantly increased by 36 weeks’ corrected age such that all infants had levels above 30 ng ml−1, and levels at 36 weeks in this cohort were not associated with BPD.
Our study is in agreement with a study by Onwuneme et al.16 in which, in a cohort of 94 preterm infants (<32 weeks’ gestation), there was no association with BPD or other morbidities of prematurity although the authors found an association between vitamin D status and acute respiratory morbidity (as defined by differences in duration of positive pressure ventilation and highest oxygen concentration required in the delivery room and the odds of requiring assisted ventilation). Similarly, a recent interventional trial of three dosing regimens for vitamin D supplementation in extremely preterm infants found no association between vitamin D status and respiratory outcomes. 17
The importance of vitamin D status in pediatric respiratory health is supported by large epidemiologic studies of term infants showing an association between suboptimal vitamin D status and wheezing.4, 18 In addition, animal studies demonstrate an important biologic role for vitamin D in lung development and maturation, including differentiation of type II pneumocytes, surfactant phospholipid synthesis and secretion,19 as well as an immunomodulatory role in epithelial cells, neutrophils and macrophages. Finally, interventional animal and human studies provide strong evidence for a beneficial role of vitamin D supplementation in pulmonary outcomes.7, 20
The role of vitamin D status in the development of BPD remains incompletely understood. Mandel et al.7 reported a protective role for vitamin D in a rodent model of neonatal lung injury induced by in utero exposure to endotoxin. Backstrom et al.21 conducted a randomized trial of 39 preterm infants (<33 weeks) to 200 vs 960 IU of vitamin D per day for 3 months and observed, as a secondary outcome, a reduced need for assisted ventilation in the high-dose group. An observational study conducted by Ataseven et al.22 demonstrated a very high prevalence of suboptimal 25(OH)D levels in a cohort of 152 preterm infants (29 to 35 weeks) born in Turkey and, in unadjusted analyses, a significantly higher incidence of respiratory distress syndrome in infants with 25(OH)D levels <10 ng ml−1. Similarly, Cetinkaya et al.23 reported that by univariate analysis lower cord blood 25(OH) levels were associated with BPD in a cohort of 100 preterm infants (<32 weeks) born in Turkey. However, the multivariate regression analysis in the same study did not show an independent association between cord blood 25(OH)D levels and BPD.
Given that vitamin D has important roles in early lung development and innate immunity, the lack of association between vitamin D status and development of BPD supports the multifactorial etiology of and possible genetic predisposition to BPD. The association between low vitamin D levels and respiratory morbidity as seen in older children and adults may be due to different pathology than that seen in BPD, which is characterized by alveolar simplification and impaired septation. In addition, oxygen toxicity, barotrauma, volutrauma and various other factors have been shown to have a role in BPD. A variety of host factors may confer altered susceptibility to BPD in preterm infants and some of these may be genetic and related to vitamin D bioavailability that is not reflected in 25(OH)D levels. For example, common vitamin D-related polymorphisms, in vitamin D-binding protein or VDR likely alter the bioavailable levels of 25(OH)D.24 A study by Koroglu et al.25 examined the role of the VDR variant Fok 1 in BPD risk among 109 preterm neonates but did not find a significant change in the odds ratio. In addition, large-scale human studies may yield altered risk for BPD in association with vitamin D-binding protein and VDR polymorphisms. In addition, during pregnancy and early childhood, a less biologically active C3-epimer of 25(OH)D is generated within the fetal-placental unit.26, 27 Most quantitative assays of 25(OH)D, including chemiluminescence used in our study include this inactive or less active epimer and therefore introduce another limitation in the interpretation of 25(OH)D levels. This in turn may contribute to some extent to the lack of association with morbidities such as BPD.
Fetal and newborn concentrations of 25(OH)D depend on and correlate with maternal serum levels as the fetus has no endogenous production of 25(OH)D and depends on transplacental transfer.28 This occurs mainly in the third trimester and therefore, as we and others previously reported, preterm infants are at increased risk of vitamin D deficiency.10, 29 Our prior study demonstrated that birth before 32 completed weeks of gestation is an independent risk factor for low 25(OH)D levels at birth. In our current study of 44 infants born before 29 weeks’ gestation, at birth 45% had levels of 25(OH)D below 30 ng ml−1. Interventional studies by Hollis et al., Wagner et al.30, 31 and others have demonstrated that vitamin D status at birth is modifiable through maternal supplementation during pregnancy. Two recently published large intervention trials of additional vitamin D supplementation during pregnancy in the United States32 and Europe33showed trends but no significant decreases in the incidence of childhood wheezing and asthma in the first 3 years of life among the offspring. However, these studies did not address the role of vitamin D status in BPD, wheezing and asthma among preterm infants.
Current American Academy of Pediatrics guidelines34 recommend vitamin D intake of 400 IU per day for all children but there are no specific guidelines for preterm infants. The Pediatric Endocrine Society recommends targeting serum 25(OH) level of >20 ng ml−1 for children of all ages.35 At Brigham and Women’s Hospital, we aim to provide 400 IU vitamin D daily. For example, for exclusively human milk-fed infants with fortification of human milk fortifier that contains vitamin D, we additionally provide 200 units per day. For infants with a combination of human milk with fortifier, and formula, 200 units is also added until the infant is consuming a volume adequate to provide 400 units per day. With this supplementation, all of the infants in our cohort (n=20) had levels of 25(OH)D >30 ng ml−1 at 36 weeks’ corrected age.
The adequacy of current postnatal nutritional supplementation of vitamin D has recently been assessed in preterm infants in the United States and in Europe. McCarthy et al.29 reported that in a cohort of 274 preterm infants (<32 weeks) in Ireland, levels of 25(OH)D remained under 20 ng ml−1 in 78% of subjects despite 18 days on average of enteral feeding and vitamin D supplementation.29 A recent intervention trial by Fort et al.17 demonstrated that biochemical vitamin D deficiency among extremely preterm infants can be reduced by additional supplementation with 200 units of vitamin D daily, and prevented by additional supplementation with 800 units of vitamin D daily17 and these two regimens were found to be safe.
There are several limitations in our study, including its small sample size, risk of selection bias and lack of data on prenatal vitamin D supplementation and maternal 25(OH)D levels. In addition, as the oxygen challenge test at 36 weeks is not routinely used in our unit,36 we relied on supplemental oxygen use (rather than need) to define BPD. However, we re-analyzed our data using the National Institutes of Health consensus definition of BPD and found similar results.15 Further, our results should be interpreted with caution given the uncertainty regarding the optimal method of measuring 25(OH)D levels.37, 38 We measured 25(OH)D using chemiluminescence.12 The laboratory used US National Institute of Standards and Technology level 1 for quality control. Finally, as in all observational studies, it is possible that our results might be affected by unidentified confounding factors.
In conclusion, we found that low 25(OH)D levels (<30 ng ml−1) are frequent and modifiable among preterm infants at birth, however, in our study samples we did not detect any association between vitamin D status and pulmonary or other morbidities of prematurity. The current practice of targeting nutritional intake of 400 IU per day vitamin D is sufficient to achieve serum 25(OH)D levels >30 ng ml−1 at 36 weeks’ corrected age. Given the limitations of a modest sample size of our study, we propose that our data combined with others for a meta-analysis may be warranted before consideration of interventional trials of vitamin D supplementation.
References
Jain D, Bancalari E . Bronchopulmonary dysplasia: clinical perspective. Birth Defects Res A Clin Mol Teratol 2014; 100 (3): 134–144.
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 2010; 126 (3): 443–456.
Woythaler MA, McCormick MC, Smith VC . Late preterm infants have worse 24-month neurodevelopmental outcomes than term infants. Pediatrics 2011; 127 (3): e622–e629.
Camargo CA Jr., Rifas-Shiman SL, Litonjua AA, Rich-Edwards JW, Weiss ST, Gold DR et al. Maternal intake of vitamin D during pregnancy and risk of recurrent wheeze in children at 3 y of age. Am J Clin Nutr 2007; 85 (3): 788–795.
Brehm JM, Celedon JC, Soto-Quiros ME, Avila L, Hunninghake GM, Forno E et al. Serum vitamin D levels and markers of severity of childhood asthma in Costa Rica. Am J Respir Crit Care Med 2009; 179 (9): 765–771.
Brehm JM, Acosta-Perez E, Klei L, Roeder K, Barmada M, Boutaoui N et al. Vitamin D insufficiency and severe asthma exacerbations in Puerto Rican children. Am J Respir Crit Care Med 2012; 186 (2): 140–146.
Mandell E, Seedorf G, Gien J, Abman SH . Vitamin D treatment improves survival and infant lung structure after intra-amniotic endotoxin exposure in rats: potential role for the prevention of bronchopulmonary dysplasia. Am J Physiol Lung Cell Mol Physiol 2014; 306 (5): L420–L428.
Mandell E, Seedorf GJ, Ryan SL, Gien J, Cramer SD, Abman SH . Antenatal endotoxin disrupts lung vitamin D receptor and 25-hydroxyvitamin D 1-alpha hydroxylase expression in the developing rat. Am J Physiol Lung Cell Mol Physiol 2015; 309 (9): L1018–L1026.
Shah MD, Shah SR . Nutrient deficiencies in the premature infant. Pediatric Clin North Am 2009; 56 (5): 1069–1083.
Burris HH, Van Marter LJ, McElrath TF, Tabatabai P, Litonjua AA, Weiss ST et al. Vitamin D status among preterm and full-term infants at birth. Pediatr Res 2014; 75 (1-1): 75–80.
Zerwekh JE . Blood biomarkers of vitamin D status. Am J Clin Nutr 2008; 87 (4): 1087S–1091.
Ersfeld DL, Rao DS, Body JJ, Sackrison JL Jr, Miller AB, Parikh N et al. Analytical and clinical validation of the 25 OH vitamin D assay for the LIAISON automated analyzer. Clin Biochem 2004; 37 (10): 867–874.
Poindexter BB, Feng R, Schmidt B, Aschner JL, Ballard RA, Hamvas A et al. Comparisons and limitations of current definitions of bronchopulmonary dysplasia for the prematurity and respiratory outcomes program. Ann Am Thorac Soc 2015; 12 (12): 1822–1830.
Poindexter BB, Jobe AH . The diagnostic conundrum of bronchopulmonary dysplasia. J Pediatr 2015; 167 (3): 517–518.
Jobe AH, Bancalari E . Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001; 163 (7): 1723–1729.
Onwuneme C, Martin F, McCarthy R, Carroll A, Segurado R, Murphy J et al. The association of vitamin D status with acute respiratory morbidity in preterm infants. J Pediatr 2015; 166 (5): 1175–80 e1.
Fort P, Salas AA, Nicola T, Craig CM, Carlo WA, Ambalavanan N . A comparison of 3 vitamin D dosing regimens in extremely preterm infants: a randomized controlled trial. J Pediatr 2016; 174: 132–138.
Vo P, Bair-Merritt M, Camargo CA . The potential role of vitamin D in the link between obesity and asthma severity/control in children. Expert Rev Respir Med 2015; 9 (3): 309–325.
Clancy N, Onwuneme C, Carroll A, McCarthy R, McKenna MJ, Murphy N et al. Vitamin D and neonatal immune function. J Matern Fetal Neonatal Med 2013; 26 (7): 639–646.
Grant CC, Kaur S, Waymouth E, Mitchell EA, Scragg R, Ekeroma A et al. Reduced primary care respiratory infection visits following pregnancy and infancy vitamin D supplementation: a randomised controlled trial. Acta Paediatr 2015; 104 (4): 396–404.
Backstrom MC, Maki R, Kuusela AL, Sievanen H, Koivisto AM, Ikonen RS et al. Randomised controlled trial of vitamin D supplementation on bone density and biochemical indices in preterm infants. Arch Dis Child Fetal Neonatal Ed 1999; 80 (3): F161–F166.
Ataseven F, Aygun C, Okuyucu A, Bedir A, Kucuk Y, Kucukoduk S . Is vitamin d deficiency a risk factor for respiratory distress syndrome? Int J Vitam Nutr Res 2013; 83 (4): 232–237.
Cetinkaya M, Cekmez F, Erener-Ercan T, Buyukkale G, Demirhan A, Aydemir G et al. Maternal/neonatal vitamin D deficiency: a risk factor for bronchopulmonary dysplasia in preterms? J Perinatol 2015; 35 (10): 813–817.
Navas-Nazario A, Li FY, Shabanova V, Weiss P, Cole DE, Carpenter TO et al. Effect of vitamin D-binding protein genotype on the development of asthma in children. Ann Allergy Asthma Immunol 2014; 112 (6): 519–524.
Koroglu OA, Onay H, Cakmak B, Bilgin B, Yalaz M, Tunc S et al. Association of vitamin D receptor gene polymorphisms and bronchopulmonary dysplasia. Pediatr Res 2014; 76 (2): 171–176.
Yazdanpanah M, Bailey D, Walsh W, Wan B, Adeli K . Analytical measurement of serum 25-OH-vitamin D(3), 25-OH-vitamin D(2) and their C3-epimers by LC-MS/MS in infant and pediatric specimens. Clin Biochem 2013; 46 (13–14): 1264–1271.
Bailey D, Perumal N, Yazdanpanah M, Al Mahmud A, Baqui AH, Adeli K et al. Maternal-fetal-infant dynamics of the C3-epimer of 25-hydroxyvitamin D. Clin Biochem 2014; 47 (9): 816–822.
Weisman Y . Maternal, fetal and neonatal vitamin D and calcium metabolism during pregnancy and lactation. Endocr Dev 2003; 6: 34–49.
McCarthy RA, McKenna MJ, Oyefeso O, Uduma O, Murray BF, Brady JJ et al. Vitamin D nutritional status in preterm infants and response to supplementation. Br J Nutr 2013; 110 (1): 156–163.
Wagner CL, McNeil R, Hamilton SA, Winkler J, Rodriguez Cook C, Warner G et al. A randomized trial of vitamin D supplementation in 2 community health center networks in South Carolina. Am J Obstetr Gynecol 2013; 208 (2): 137 e1–e13.
Hollis BW, Johnson D, Hulsey TC, Ebeling M, Wagner CL . Vitamin D supplementation during pregnancy: double-blind, randomized clinical trial of safety and effectiveness. J Bone Miner Res 2011; 26 (10): 2341–2357.
Litonjua AA, Carey VJ, Laranjo N, Harshfield BJ, McElrath TF, O'Connor GT et al. Effect of prenatal supplementation with vitamin D on asthma or recurrent wheezing in offspring by age 3 years: the VDAART randomized clinical trial. JAMA 2016; 315 (4): 362–370.
Chawes BL, Bonnelykke K, Stokholm J, Vissing NH, Bjarnadottir E, Schoos AM et al. Effect of vitamin D3 supplementation during pregnancy on risk of persistent wheeze in the offspring: a randomized clinical trial. JAMA 2016; 315 (4): 353–361.
Abrams SA . Dietary guidelines for calcium and vitamin D: a new era. Pediatrics 2011; 127 (3): 566–568.
Misra M, Pacaud D, Petryk A, Collett-Solberg PF, Kappy M . Vitamin D deficiency in children and its management: review of current knowledge and recommendations. Pediatrics 2008; 122 (2): 398–417.
Walsh MC, Wilson-Costello D, Zadell A, Newman N, Fanaroff A . Safety, reliability, and validity of a physiologic definition of bronchopulmonary dysplasia. J Perinatol 2003; 23 (6): 451–456.
Ross AC, Taylor CL, Yaktine AL, Del Valle HB, (U.S) IoM. Committee to review dietary reference intakes for vitamin D and calcium. Dietary Reference Intakes for Calcium and Vitamin D. National Academies Press: Washington, DC, USA, 2011, pp 107–111.
de la Hunty A, Wallace AM, Gibson S, Viljakainen H, Lamberg-Allardt C, Ashwell M . UK Food Standards Agency Workshop Consensus Report: the choice of method for measuring 25-hydroxyvitamin D to estimate vitamin D status for the UK National Diet and Nutrition Survey. Br J Nutr 2010; 104 (4): 612–619.
Acknowledgements
We acknowledge Dr Wenyang Mao for biostatistical support; Marcia Filip, Yvonne Sheldon, Elena Arons and Deirdre Greene for assistance with cord blood collection and processing; and Vanessa Gaines and Elisabeth Annette Scheid for data entry. This work was supported by the Gerber Foundation and the William F. Milton Fund (to HC). The project described was supported by Clinical Translational Science Award UL1RR025758 to Harvard University and Brigham and Women’s Hospital from the National Center for Research Resources. Drs Litonjua and Weiss are supported by U01 HL091528. Dr Burris was funded by the Klarman Scholars Program at Beth Israel Deaconess Medical Center and by K23 ES022242. This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Joung, K., Burris, H., Van Marter, L. et al. Vitamin D and bronchopulmonary dysplasia in preterm infants. J Perinatol 36, 878–882 (2016). https://doi.org/10.1038/jp.2016.115
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.115
This article is cited by
-
The association of serum vitamin D level and neonatal respiratory distress syndrome
Italian Journal of Pediatrics (2023)
-
Vitamin d deficiency with high parathyroid hormone levels is related to late onset SEPSIS among preterm infants
BMC Pregnancy and Childbirth (2023)
-
Vitamin D status in very low birth weight infants and response to vitamin D intake during their NICU stays: a prospective cohort study
Journal of Perinatology (2022)
-
Vitamin D in pediatric age: consensus of the Italian Pediatric Society and the Italian Society of Preventive and Social Pediatrics, jointly with the Italian Federation of Pediatricians
Italian Journal of Pediatrics (2018)
-
Vitamin D and associated perinatal–neonatal outcomes among extremely low-birth-weight infants
Journal of Perinatology (2018)