Abstract
About 0.75 million neonates die every year in India, the highest for any country in the world. The neonatal mortality rate (NMR) declined from 52 per 1000 live births in 1990 to 28 per 1000 live births in 2013, but the rate of decline has been slow and lags behind that of infant and under-five child mortality rates. The slower decline has led to increasing contribution of neonatal mortality to infant and under-five mortality. Among neonatal deaths, the rate of decline in early neonatal mortality rate (ENMR) is much lower than that of late NMR. The high level and slow decline in early NMR are also reflected in a high and stagnant perinatal mortality rate. The rate of decline in NMR, and to an extent ENMR, has accelerated with the introduction of National Rural Health Mission in mid-2005. Almost all states have witnessed this phenomenon, but there is still a huge disparity in NMR between and even within the states. The disparity is further compounded by rural–urban, poor–rich and gender differentials. There is an interplay of different demographic, educational, socioeconomic, biological and care-seeking factors, which are responsible for the differentials and the high burden of neonatal mortality. Addressing inequity in India is an important cross-cutting action that will reduce newborn mortality.
Similar content being viewed by others
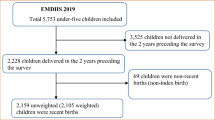
Background
The neonatal period—the first 28 days of life—carries the highest risk of mortality per day than any other period during the childhood. The daily risk of mortality in the first 4 weeks of life is ~30-fold higher than the post-neonatal period, that is, from 1 month to 59 months of age. Still, newborn health did not receive the commensurate attention it deserved until during the past decade. This has resulted in a slow decline in neonatal mortality rate (NMR) in most countries including India, and has hampered their achieving the Millennium Development Goal-4 (MDG 4) by year 2015. This article provides an overview of the burden, trends and causes of neonatal mortality, burden of common morbidities, and coverage of key interventions in India. Table 1 enlists the common terminologies used in the article and their definitions.
Neonatal mortality: the challenge
India contributes to one-fifth of global live births and more than a quarter of neonatal deaths. Nearly, 0.75 million neonates died in India in 2013, the highest for any country in the world.1 The current NMR is 28 per 1000 live births.2 Given the infant and under-five child mortality rates of 40 and 49 per 1000 live births, respectively, 70% of total infant deaths and more than half of under-five deaths fall in the neonatal period. Indeed, with the early NMR of 22 per 1000 live births, deaths in the first week alone account for ~45% of total under-five deaths.2 Obviously, the ‘Committing to Child Survival: A Promise Renewed’ goal of reducing under-five mortality to 20 or less per 1000 live births by 2035 will not be attained without specific efforts to reduce newborn mortality.
Neonatal mortality: burden over the years
There has been a significant reduction in the quantum of neonatal and child deaths in the past two decades. The annual burden of neonatal deaths has reduced from 1.35 million in 1990 to 0.75 million in 2013 (Table 1).1, 3 But the rate of decline in the neonatal and child mortality rates has accelerated only in the past decade—for example, neonatal deaths reduced by 33% in the period from 2000 to 2013 compared with 17% from 1990 to 2000 (Table 2).
Neonatal mortality: trends and projections
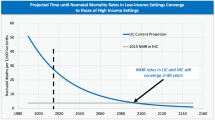
The NMR has declined from 44 per 1000 live births in 2000 to 28 per 1000 live births in 2013. But this rate of decline has nevertheless lagged behind that of infant mortality rate (Figure 1). The average annual rate of reduction (AARR) of NMR was only modest—at ~3.5%—in this period, compared with the rate of reduction of infant mortality rate (IMR) during the same period (4.0%). The higher AARR of post-neonatal infant deaths, that is, deaths in infants aged 1–12 months, compared with deaths during the neonatal period is the reason for this discrepancy. The slower decline in NMR has led to increasing contribution of neonatal mortality to infant mortality. Among neonatal deaths, the rate of decline in the ENMR was much lower than in the late NMR—AARR of 2.8% and 5.8%, respectively.
The projected NMRs for 2017 and 2020, based on the AARR from 2000 to 2012, are 24 and 22 per 1000 live births, respectively. The projected rates for ENMR for 2017 and 2020 are 20 and 18 per 1000 live births, whereas that for late NMR are 4 and 4 per 1000 live births, respectively. The projected rates are likely to be overestimates because the rate of decline in IMR and NMR has accelerated with the introduction of the National Rural Health Mission (NRHM) in mid-2005. For example, the AARR for NMR was 0 in the pre-NRHM (2003–2005) epoch, but had increased to 2.8% per year in the peri-NRHM epoch (2006–2008), when the program was being rolled out in a phased manner across the country. It further increased to 4.6% per year in the period between 2009 and 2011 when the program had been fully implemented. The NMRs in 2017 and 2020 may therefore be lower than the projected rates.
Neonatal mortality: causes
A systematic analysis of global, regional and national causes of child mortality in 2013 identified preterm birth complications and infections to be the two major causes of neonatal deaths in India (Figure 2).1, 4 The review, which included the data from the Million Death Study from India,5 found perinatal asphyxia and malformations to be the other two significant causes of neonatal mortality. These findings are very similar to the overall global pattern.4
Timing of neonatal deaths
A pooled analysis of the data from three studies on the timing of neonatal deaths indicates that about three-fourths of total neonatal deaths occur in the first week of life.6, 7, 8 The first 24 h account for more than one-third (36.9%) of the deaths that occur in the entire neonatal period.
A recent prospective study by Baqui et al.6 provided data on the timing of cause-specific neonatal deaths: almost all deaths (97.8%) due to asphyxia occur in the first week of life, with 70% of them occurring within the first 24 h (day 0). About three-fourth of deaths due to prematurity (74.8%) occur in the first week of life, with 30% in the first 24 h (day 0) <50% of neonatal deaths secondary to sepsis occur in the first week of life. About 30% of sepsis-related deaths occur in the second week, whereas around one-fifth in weeks 3–4. Three-fourth of the deaths due to malformations occur in the first week of life, with day 0 alone contributing to nearly half of these deaths. 6
Neonatal mortality: determinants
In India, inequities with corresponding underlying axes of caste, class, gender and geographical differences define a very large segment of the population. A High-Level Expert Group appointed by the Planning Commission of India observed that considering the health inequality and social inequality interface, the poorest and most disadvantaged have a higher risk for diseases. This includes the urban and rural poor, women and children, specially abled persons, and traditionally marginalized and excluded communities such as adivasis, or STs, dalits, or SCs, and ethnic and religious minorities. They also have a higher probability of being excluded from the health services. The neonates born in these populations are expected to be the most vulnerable to morbidity and mortality.9
Geographical variations
The NMR is not uniform across the country. Although Kerala and Tamil Nadu have low NMRs (<20 per 1000 live births), Odisha, Madhya Pradesh and Uttar Pradesh have very high NMRs (35 or more per 1000 live births; Figure 3)2 Four states—Uttar Pradesh, Madhya Pradesh, Bihar and Rajasthan—alone contribute to ~55% of total neonatal deaths in India2, 10 and to ~15% of global neonatal deaths that occur every year.
Wide disparities are also observed in survival rates across districts within states. It is evident that within a given state, NMR may be more than twice as high in the ‘worst’ districts as in the ‘best’ one.11
Rural–urban, poor–rich differences
There are important rural–urban and socioeconomic differences in the NMR. The NMR in rural areas is twice that in urban areas (31 vs 15 per 1000 live births). The discrepancy is more marked—difference of 60% or more—in Andhra Pradesh, Assam, Jharkhand and Kerala.2
Gender differences
Although recent sex-differentiated NMR estimates are not available, given the gender-based differences in care seeking in India, the NMR estimates for females are likely to be higher than those for males. A close proxy of NMR, the IMR, reaffirms this—39 for males and 42 for females (per 1000 live births).2 The annual rate of IMR decline from 2007 to 2012 is also higher for males—5.9%,0 compared with 4.8% for females. The sex differential rate of decline is more marked in some states—Andhra Pradesh, Delhi, Karnataka, Kerala and Madhya Pradesh.
Gender discrimination at each stage of the female life cycle contributes to gender-based health disparities including sex-selective abortions, neglect in care of the female child, and poor access to healthcare for girls.12, 13, 14, 15, 16 Recent data for admissions in special newborn care units have also demonstrated differential care seeking for males and females. At the district level, newborn care units typically admit ~30% less females than male neonates.17 A study conducted in Uttar Pradesh (UP) demonstrates that while the overall use of health-care providers is similar across gender, the average expenditure for healthcare during the neonatal period is nearly fourfold higher in households with male newborns compared with those with female newborns. Households with female newborns use cheaper public care providers, whereas those with males prefer to use private providers who are perceived to deliver more satisfactory care.18
Per capita GDP
An inverse relationship exists between the per capita net state domestic product and NMR—states with a high NMR usually have a low per capita GDP.19 But there are a few exceptions—Haryana and Gujarat have a similar or higher per capita GDP than Tamil Nadu, but almost double the NMR.
Social status
In India’s caste-based social hierarchy, the scheduled castes (SCs), dalits, adivasis and scheduled tribes (STs) are the most backward and disadvantaged. A recent study has documented a higher vulnerability of SC children as compared with ST children: the odds of neonatal mortality among STs are lower by 28% as compared with SC communities in rural areas.20 Family characteristics contribute significantly in determining the status of newborn health. Upadhyay et al.21 found that low educational status of parents (odds ratio (OR) 2.1, 95% CI; 1.4, 3.3), father’s occupation (OR 1.8, 95% CI; 1.0, 3.0) and caste (OR 2.0, 95% CI; 1.2, 3.4) appears to explain a major fraction (45.7%) of neonatal deaths in Haryana.
Environment conditions
In contrast to children born in families with better financial resources, poorer children are more at risk for diseases due to inadequate water and sanitation, indoor air pollution, crowding and poor housing conditions.22 Access to clean water supply, and sanitation and good hygienic practices, especially at delivery points, is crucial for a safe delivery, and prevention of maternal and newborn mortality and morbidity. Creating conditions for better hygiene and reduced exposure to contamination makes children less susceptible to diseases and infections that may lead to death.20, 23, 24
Maternal factors
Maternal factors including age at birth, educational and nutritional status, and parity influence the neonatal survival to a great extent. The median maternal age at first childbirth in India is 19.9 years; ~30% of girls give birth before the age of 20 and account for 21% of all deliveries.25 It is estimated that the risks of neonatal mortality and low birth weight (LBW) are increased by almost 50% if maternal age at childbirth is <20 years. It is also estimated that shifting age at childbirth to above 20 years would reduce overall NMR by 9.4%.26, 27, 28, 29, 30
Evidence demonstrates that improving maternal education is the most effective and proven strategy to improve neonatal survival, as it improves preventive behaviors and increases the utilization of maternal and neonatal health-care services.31, 32, 33 Kerala’s achievement of stabilizing population growth and low levels of infant and neonatal mortality is partly attributed to its high female education levels.25
Utilization of health services
The heterogeneity in health service coverage has a significant role in producing inequitable health outcomes. A recently published systematic review on inequity in maternal health in India highlighted the fact that women of some population groups remained systematically and consistently disadvantaged in terms of access to and use of maternal and reproductive health services, including safe delivery and antenatal care services.34 Program initiatives based on average performance achievements of states rather than on deprived groups increases disadvantages for vulnerable populations within high achieving states.35, 36, 37 In addition, inadequate funding, poor infrastructure and insufficient manpower at health facilities, and poor governance pose major challenges to equitable access to free or affordable health services, often forcing poor households to make high out-of-pocket expenditures on healthcare, which is often of poor quality.
Perinatal mortality and stillbirth rate
The current perinatal mortality rate (PMR) of India (2013) is 26 per 1000 births.2 It ranges from 16 per 1000 births in urban areas to 28 per 1000 births in rural areas. As with NMR, the PMR is not uniform across the country—the PMR of Kerala is only 9 per 1000 births, whereas that of Odisha is 35 per 1000 births.2 The stillbirth rate (SBR) is estimated at four per 1000 births.2 The estimated values of both SBR and PMR are likely to be underestimates, as stillbirths are extremely difficult to capture and may be misclassified Interestingly, the estimated SBR of India for year 2009 is 22.1 per 1000 births;38 in contrast, the SBR as reported by sample registration system for year 2010 was 7 per 1000 births.
Neonatal morbidities
Neonatal morbidities constitute a huge burden to the health system and society in general. The SEARCH study by Bang et al (1995–1996) provided a detailed insight into the burden of common morbidities in rural community settings.39 A recent study conducted in Lucknow among the urban poor reported upper respiratory tract infection, diarrhea, septicemia and pneumonia to be the most common morbidities during follow-up until 6 weeks of age.40
LBW/preterm birth
Nearly 30% of neonates—7.5 million—are born with a LBW (<2500 g) in India.41 This accounts for 42% of the global burden, the largest for any country. About 60% of the LBW infants are born at term after fetal growth restriction, whereas the remaining 40% are born preterm.42 The prevalence of SGA is 46.9%, higher than all but two countries in the world (Pakistan and Mauritania have a marginally higher prevalence at 47.0%).41 Each year, ~3.5 million preterm (<38 weeks of gestation) neonates are born in India.41 Community-based studies indicate that the LBW infants are at 11–13 times increased risk of dying than NBW infants.43 Indeed, >80% of total neonatal deaths occur among LBW/preterm neonates.26, 44
Neonatal sepsis
The burden of neonatal sepsis is huge in the country. Hospital-based studies suggest an incidence of 30 per 1000 live births,42 whereas community-based studies indicate an incidence of 2.7–17% of all live births.42, 43 Nearly, one-fifth of neonates with sepsis die in the hospital; the figure rises to up to 50% for those with culture proven sepsis (Delhi Neonatal Infection Study Group; personal communication). They stay longer in the hospital, consume more resources and are also at a high risk of major neurodevelopmental disabilities at a later age.
Perinatal asphyxia
Intrapartum-related conditions or perinatal asphyxia not only leads to neonatal deaths, but also accounts for a significant proportion of stillbirths. It is difficult to estimate the true burden of asphyxia because of the different definitions used in the studies. The reported incidence varies from 2 to 16.2% in community-based studies,45 with the reported case fatality rates ranging from 38.5 to 74%. About 2.8 and 5.6% of all live births had moderate and severe asphyxia, respectively, in a large hospital-based study; the case fatality rate was relatively low at ~8.7%.42
Coverage of key interventions in antenatal, natal and post-neonatal periods
The coverage evaluation survey in 2009 (CES 2009) assessed the coverage of key interventions in antenatal, intrapartum and postnatal periods that can influence neonatal health.46 Only a quarter of pregnant women had full antenatal check-up, that is, three or more antenatal checkups, at least one tetanus toxoid injection and at least 100+ iron and folic acid tablets during pregnancy. About 73% of women had institutional deliveries.46, 47 Only one-third of neonates were breastfed within 1 h after birth.46 Less than half of the neonates received three postnatal visits by health-care providers in the first 10 days of life.48, 49, 50, 51, 52, 53, 54
Although several initiatives, such as Janani Suraksha Yojana and Janani Shishu Suraksha Karyakram, have attempted to address these gaps, their impact remains limited due to poor governance, shortage of health workers in primary health-care facilities and lack of preparedness of health-care facilities.55, 56
Ensuring equitable access to health services requires a clear understanding of the multiple levels of inequity across many sectors. It is important that all public policies have synergy with health policies and programs. International organizations, national and state governments, civil society, and research and academic institutions have a major role to have in ensuring equitable service delivery and improved health governance. The inter-sectoral approaches need to be promoted within and between departments. Improving access to safe water and sanitation, providing adequate food security, and poverty alleviation measures complemented by an equitable health system can ensure better health outcomes for every neonate in India.57
Conclusions
India has witnessed a significant improvement in neonatal health after the introduction of NRHM. Apart from the JSY, the country has launched several new initiatives to improve neonatal care. Notwithstanding this newfound focus on neonatal health, the annual rate of reduction in NMR and ENMR still lags behind IMR and U5MR. There is an interplay of different demographic, educational, socioeconomic, biological and care-seeking factors, which are responsible for the disparities and the high burden of neonatal mortality. The country has to increase the coverage of key interventions and also improve the quality of care in health facilities on an urgent basis.
References
Liu L, Oza S, Hogan D, Perin J, Rudan I, Lawn JE et al. Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet 2015; 385 (9966): 430–440.
Registrar General of India. Sample registration system (SRS) statistical report 2013. New Delhi: 2013.
World Health Organization. WHO Data. Available at http://data.un.org/Explorer.aspx?d=WHO (accessed on 20 August 2014).
Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 2012; 379: 2151–2161.
Bassani DG, Kumar R, Awasthi S, Morris SK, Paul VK, Shet A et al. Causes of neonatal and child mortality in India: a nationally representative mortality survey. Lancet 2010; 376: 1853–1860.
Baqui AH, Darmstadt GL, Williams EK, Kumar V, Kiran TU, Panwar D et al. Rates, timing and causes of neonatal deaths in rural India: implications for neonatal health programmes. Bull World Health Organ 2006; 84: 706–713.
ICMR Young Infant Study Group. Age profile of neonatal deaths. Indian Pediatr 2008; 45: 991–994.
Bang AT, Paul VK, Reddy HM, Baitule SB . Why do neonates die in rural Gadchiroli, India? (Part I): primary causes of death assigned by neonatologist based on prospectively observed records. J Perinatol 2005; 25 (Suppl 1): S29–S34.
HLEG High Level Expert Group Report on Universal Health Coverage for India. Public Health Foundation of India: New Delhi, 2011.
Registrar General of India. Census 2011. Provisional population totals of 2011. Available at http://www.censusindia.gov.in/2011-prov-results/PPT_2.html (accessed on 20 August 2014).
Annual Health Survey. 2010-11. Office of the Registrar General & Census Commissioner, Ministry of Home Affairs, Government of India.
Fikree FF, Pasha O . Role of gender in health disparity: the South Asian context. BMJ 2004; 328 (7443): 823.
Claeson M, Bos ER, Mawji T, Pathmanathan I . Reducing child mortality in India in the new millennium. Bull World Health Organ 2000; 78: 1192–1199.
Dettrick Z, Jimenez-Soto E, Hodge A . Socioeconomic and geographical disparities in under-five and neonatal mortality in Uttar Pradesh, India. Matern Child Health J 2013; 18: 960–969.
Chatterjee M . A Report on Indian Women from Birth to Twenty. National Institute of Public Cooperation and Child Development: New Delhi, 1990.
Murthi M, Guio A-C, Dreze J . Mortality, fertility, and gender bias in India: a district-level analysis. Popul Dev Rev 1995; 21: 745–782.
Government of India. Ministry of Health & Family Welfare (MOHFW). Two-year progress of special newborn care units in India: a brief report 2013.
Willis JR, Kumar V, Mohanty S, Singh P, Singh V, Baqui AH et al. Gender differences in perception and care-seeking for illness of newborns in rural Uttar Pradesh, India. J Health Popul Nutr 2009; 27 (1): 62.
Government of India: Planning Commission. Per capita net state domestic product at current prices. Available at http://planningcommission.nic.in/data/datatable/index.php?data=datatab (accessed on 14 April 2014).
Singh A, Kumar A, Kumar A . Determinants of neonatal mortality in rural India. 2007–2008. Peer J 2013; 1: e75.
Upadhyay RP, Dwivedi PR, Rai SK, Misra P, Kalaivani M, Krishnan A . Determinants of neonatal mortality in rural Haryana: a retrospective population based study. Indian Pediatrics 2012; 49 (4): 291–294.
Victora CG, Wagstaff A, Schellenberg JA, Gwatkin D, Claeson M, Habicht JP . Applying an equity lens to child health and mortality: more of the same is not enough. Lancet 2003; 362 (9379): 233–241.
Fewtrell L, Kaufmann RB, Kay D, Enanoria W, Haller L, Colford JM Jr . Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. Lancet Infect Dis 2005; 5 (1): 42–52.
United Nations Children Fund (UNICEF) State of World Children: Maternal and Newborn Health. UNICEF: New York, USA, 2009.
Upadhyay RP, Chinnakali P, Odukoya O, Yadav K, Sinha S, Rizwan SA et al. High neonatal mortality rates in rural India: what options to explore? ISRN Pediatr 2012; 2012: 968921.
Paul VK, Sachdev HS, Mavalankar D, Ramachandran P, Sankar MJ, Bhandari N et al. Reproductive health, and child health and nutrition in India: meeting the challenge. Lancet 2011; 377: 332–349.
Conde-Agudelo A, Belizán JM, Lammers C . Maternal-perinatal morbidity and mortality associated with adolescent pregnancy in Latin America: cross-sectional study. Am J Obset Gynecol 2005; 192 (2): 342–349.
United Nations Children Fund (UNICEF) Early Marriage: Child Spouses (Innocenti Digest Innocenti Research Centre, UNICEF: Florence, Italy, 2001.
Alam N . Teenage motherhood and infant mortality in Bangladesh: maternal age-dependent effect of parity one. J Biosoc Sci 2000; 32 (02): 229–236.
Raj A, Saggurti N, Winter M, Labonte A, Decker MR, Balaiah D et al. The effect of maternal child marriage on morbidity and mortality of children under 5 in India: cross sectional study of a nationally representative sample. BMJ 2010; 340: b4258.
Agha S, Carton TW . Determinants of institutional delivery in rural Jhang, Pakistan. Int J Equity Health 2011; 10 (1): 1–12.
Navaneetham K, Dharmalingam A . Utilization of maternal healthcare services in southern India. Soc Sci Med 2002; 55 (10): 1849–1869.
Ogunlesi TA, Ogunlesi FB . Family socio-demographic factors and maternal obstetric factors influencing appropriate health-care seeking behaviours for newborn jaundice in Sagamu, Nigeria. Mater Child Health J 2012; 16 (3): 677–684.
Saxena D, Vangani R, Mavalankar DV, Thomsen S . Inequity in maternal healthcare service utilization in Gujarat: analyses of district-level health survey data. Glob Health Action 2013; 6: 1–9.
Singh PK, Rai RK, Kumar C . Equity in maternal, newborn, and child healthcare coverage in India. Global Health Action 2013; 6: 22217.
Singh Z . Universal health coverage for India by 2022: autopia or reality? Indian J Community Med 2013; 38 (2): 70.
Sanneving L, Trygg N, Saxena D, Mavalankar D, Thomsen S . Inequity in India: the case of maternal and reproductive health. Glob Health Action 2013; 6: 19145.
Cousens S, Blencowe H, Stanton C, Chou D, Ahmed S, Steinhardt L et al. National, regional, and worldwide estimates of stillbirth rates in 2009 with trends since 1995: a systematic analysis. Lancet 2011; 377 (9774): 1319–1330.
Bang AT, Reddy HM, Baitule SB, Deshmukh MD, Bang RA . The incidence of morbidities in a cohort of neonates in rural Gadchiroli, India: seasonal and temporal variation and a hypothesis about prevention. J Perinatol 2005; 25 (Suppl 1): S18–S28.
Srivastava NM, Awasthi S, Agarwal GG . Care-seeking behavior and out-of-pocket expenditure for sick newborns among urban poor in Lucknow, northern India: a prospective follow-up study. BMC Health Serv Res 2009; 9: 61.
Lee ACC, Katz J, Blencowe H, Cousens S, Kozuki N, Vogel JP et al. National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Glob Health 2013; 1: e26–e36.
National Neonatal Perinatal Database. Report for the year 2002–03. Available at http://www.newbornwhocc.org/pdf/nnpd_report_2002-03.PDF (accessed on 2 April 2016).
Bang AT, Bang RA, Baitule S, Deshmukh M, Reddy MH . Burden of morbidities and the unmet need for health care in rural neonates—a prospective observational study in Gadchiroli, India. Indian Pediatr 2001; 38: 952–965.
Chaudhari S, Bhalerao MR, Chitale A, Pandit AN, Nene U . Pune low birth weight study—a six year follow up. Indian Pediatr 1999; 36: 669–676.
Daga SR, Daga AS, Dighole RV, Patil RP, Dhinde HL . Rural neonatal care: Dahanu experience. Indian Pediatr 1992; 29 (2): 189–193.
United Nations Children Fund (UNICEF) Coverage Evaluation Survey 2009. UNICEF: New Delhi, India, 2009.
Singh PK, Rai RK, Alagarajan M, Singh L . Determinants of maternity care services utilization among married adolescents in rural India. PLOS One 2012; 7 (2): e31666.
Narang M, Kaushik JS, Sharma AK, Faridi MM . Predictors of mortality among the neonates transported to referral centre in Delhi. Indian J Public Health 2013; 57: 100–104.
Save the Children & Population Reference Bureau (PRB) Postnatal Care: Acritical Opportunity to Save Mothers and Newborns. Save the Children & PRB: Washington, DC, USA, 2007.
Baqui AH, Ahmed S, El Arifeen S, Darmstadt GL, Rosecrans AM, Mannan I et al. Effect of timing of first postnatal care home visit on neonatal mortality in Bangladesh: a observational cohort study. BMJ 2009; 339: b2826.
Pati S, Chauhan AS, Panda M, Swain S, Hussain MA . Neonatal care practices in a tribal community of Odisha, India: a cultural perspective. J Trop Pediatr 2014; 60 (3): 238–244.
Joseph N, Unnikrishnan B, Naik VA, Mahantshetti NS, Mallapur MD, Kotian SM et al, Infant rearing practices in south India: a longitudinal study. J Family Med Prim Care 2013; 2 (1): 37–43.
Patel A, Badhoniya N, Khadse S, Senarath U, Agho KE, Dibley MJ et al. Infant and young child feeding indicators and determinants of poor feeding practices in India: secondary data analysis of National Family Health Survey 2005-06. Food Nutr Bull 2010; 31 (2): 314–333.
Garcia CR, Mullany LC, Rahmathullah L, Katz J, Thulasiraj RD, Sheeladevi S et al. Breast-feeding initiation time and neonatal mortality risk among newborns in south India. J Perinatol 2011; 31 (6): 397–403.
Malini S, Tripathi RM, Khattar P, Nair KS, Tekhre YL, Dhar N et al. A rapid appraisal on functioning of Janani Suraksha Yojana in South Orissa. Health Popul Perspect Issues 2008; 31: 126 rap.
Lim SS, Dandona L, Hoisington JA, James SL, Hogan MC, Gakidou E . India's Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: an impact evaluation. Lancet 2010; 375 (9730): 2009–2023.
Balarajan Y, Selvaraj S, Subramanian S . Healthcare and equity in India. Lancet 2011; 377 (9764): 505–515.
Acknowledgements
This study was supported by Save the Children’s Saving Newborn Lives program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Sankar, M., Neogi, S., Sharma, J. et al. State of newborn health in India. J Perinatol 36 (Suppl 3), S3–S8 (2016). https://doi.org/10.1038/jp.2016.183
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.183
This article is cited by
-
Neonatal, Infant, and Child Mortality in India: Progress and Future Directions
Indian Journal of Pediatrics (2023)
-
Effect of Kangaroo Mother Care Transport in Preventing Moderate Hypothermia in Low Birth Weight Babies During Transportion to Home After Discharge: A Randomized Controlled Trial
Indian Pediatrics (2023)
-
Tele-NICU: A Possible Solution for Bridging the ‘Gap’
Indian Pediatrics (2023)
-
Fabrication, assessment, and potential anti-bacterial activity of sandalwood oil nanoemulsion and its hand rub sanitizer
Environmental Science and Pollution Research (2023)
-
Sex inequality in under-five deaths and associated factors in low and middle-income countries: a Fairlie decomposition analysis
BMC Public Health (2022)