Abstract
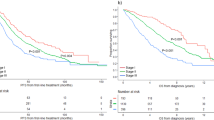
The association of genetic lesions detected by fluorescence in situ hybridization (FISH) with survival was analyzed in 1069 patients with newly presenting myeloma treated in the Medical Research Council Myeloma IX trial, with the aim of identifying patients associated with the worst prognosis. A comprehensive FISH panel was performed, and the lesions associated with short progression-free survival and overall survival (OS) in multivariate analysis were +1q21, del(17p13) and an adverse immunoglobulin heavy chain gene (IGH) translocation group incorporating t(4;14), t(14;16) and t(14;20). These lesions frequently co-segregated, and there was an association between the accumulation of these adverse FISH lesions and a progressive impairment of survival. This observation was used to define a series of risk groups based on number of adverse lesions. Taking this approach, we defined a favorable risk group by the absence of adverse genetic lesions, an intermediate group with one adverse lesion and a high-risk group defined by the co-segregation of >1 adverse lesion. This genetic grouping was independent of the International Staging System (ISS) and so was integrated with the ISS to identify an ultra-high-risk group defined by ISS II or III and >1 adverse lesion. This group constituted 13.8% of patients and was associated with a median OS of 19.4 months.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Greipp PR, San Miguel J, Durie BG, Crowley JJ, Barlogie B, Blade J et al. International staging system for multiple myeloma. J Clin Oncol 2005; 23: 3412–3420.
Shaughnessy Jr JD, Zhan F, Burington BE, Huang Y, Colla S, Hanamura I et al. A validated gene expression model of high-risk multiple myeloma is defined by deregulated expression of genes mapping to chromosome 1. Blood 2007; 109: 2276–2284.
Decaux O, Lode L, Magrangeas F, Charbonnel C, Gorand W, Jezequel P et al. Prediction of survival in multiple myeloma based on gene expression profiles reveals cell cycle and chromosomal instability signatures in high-risk patients and hyperdiplod signatures in low risk patients: a study of the Intergroupe Francophone du Myelome. J Clin Oncol 2008; 26: 4798–4805.
Dickens NJ, Walker BA, Leone PE, Johnson DC, Brito JL, Zeisig A et al. Homozygous deletion mapping in myeloma samples identifies genes and an expression signature relevant to pathogenesis and outcome. Clin Cancer Res 2010; 16: 1856–1864.
Keats JJ, Reiman T, Maxwell CA, Taylor BJ, Larratt LM, Mant MJ et al. In multiple myeloma, t(4;14)(p16;q32) is an adverse prognostic factor irrespective of FGFR3 expression. Blood 2003; 101: 1520–1529.
Fonseca R, Blood E, Rue M, Harrington D, Oken MM, Kyle RA et al. Clinical and biologic implications of recurrent genomic aberrations in myeloma. Blood 2003; 101: 4569–4575.
Chang H, Sloan S, Li D, Zhuang L, Yi QL, Chen CI et al. The t(4;14) is associated with poor prognosis in myeloma patients undergoing autologous stem cell transplant. Br J Haematol 2004; 125: 64–68.
Gertz MA, Lacy MQ, Dispenzieri A, Greipp PR, Litzow MR, Henderson KJ et al. Clinical implications of t(11;14)(q13;q32), t(4;14)(p16.3;q32), and -17p13 in myeloma patients treated with high-dose therapy. Blood 2005; 106: 2837–2840.
Zhan F, Huang Y, Colla S, Stewart JP, Hanamura I, Gupta S et al. The molecular classification of multiple myeloma. Blood 2006; 108: 2020–2028.
Avet-Loiseau H, Attal M, Moreau P, Charbonnel C, Garban F, Hulin C et al. Genetic abnormalities and survival in multiple myeloma: the experience of the Intergroupe Francophone du Myelome. Blood 2007; 109: 3489–3495.
Neben K, Jauch A, Bertsch U, Heiss C, Hielscher T, Seckinger A et al. Combining information regarding chromosomal aberrations t(4;14) and del(17p13) with the International Staging System classification allows stratification of myeloma patients undergoing autologous stem cell transplantation. Haematologica 2010; 95: 1150–1157.
San Miguel JF, Schlag R, Khuageva NK, Dimopoulos MA, Shpilberg O, Kropff M et al. Bortezomib plus melphalan and prednisone for initial treatment of multiple myeloma. N Engl J Med 2008; 359: 906–917.
Pineda-Roman M, Zangari M, Haessler J, Anaissie E, Tricot G, van Rhee F et al. Sustained complete remissions in multiple myeloma linked to bortezomib in total therapy 3: comparison with total therapy 2. Br J Haematol 2008; 140: 625–634.
Avet-Loiseau H, Leleu X, Roussel M, Moreau P, Guerin-Charbonnel C, Caillot D et al. Bortezomib plus dexamethasone induction improves outcome of patients with t(4;14) myeloma but not outcome of patients with del(17p). J Clin Oncol 2010; 28: 4630–4634.
Ross FM, Ibrahim AH, Vilain-Holmes A, Winfield MO, Chiecchio L, Protheroe RK et al. Age has a profound effect on the incidence and significance of chromosome abnormalities in myeloma. Leukemia 2005; 19: 1634–1642.
Avet-Loiseau H, Malard F, Campion L, Magrangeas F, Sebban C, Lioure B et al. Translocation t(14;16) and multiple myeloma: is it really an independent prognostic factor? Blood 2011; 117: 2009–2011.
Drach J, Ackermann J, Fritz E, Kromer E, Schuster R, Gisslinger H et al. Presence of a p53 gene deletion in patients with multiple myeloma predicts for short survival after conventional-dose chemotherapy. Blood 1998; 92: 802–809.
Chang H, Qi C, Yi QL, Reece D, Stewart AK . p53 gene deletion detected by fluorescent in situ hybridization is an adverse prognostic factor for patients with multiple myeloma following autologous stem cell transplantation. Blood 2005; 105: 358–360.
Harousseau JL, Avet-Loiseau H, Attal M, Charbonnel C, Garban F, Hulin C et al. Achievement of at least very good partial response is a simple and robust prognostic factor in patients with multiple myeloma treated with high-dose therapy: long-term analysis of the IFM 99–02 and 99–04 Trials. J Clin Oncol 2009; 27: 5720–5726.
Tricot G, Barlogie B, Jagannath S, Bracy D, Mattox S, Vesole DH et al. Poor prognosis in multiple myeloma is associated only with partial or complete deletions of chromosome 13 or abnormalities involving 11q and not with other karyotype abnormalities. Blood 1995; 86: 4250–4256.
Perez-Simon JA, Garcia-Sanz R, Tabernero MD, Almeida J, Gonzalez M, Fernandez-Calvo J et al. Prognostic value of numerical chromosome aberrations in multiple myeloma: a FISH analysis of 15 different chromosomes. Blood 1998; 91: 3366–3371.
Zojer N, Konigsberg R, Ackermann J, Fritz E, Dallinger S, Kromer E et al. Deletion of 13q14 remains an independent adverse prognostic variable in multiple myeloma despite its frequent detection by interphase fluorescence in situ hybridization. Blood 2000; 95: 1925–1930.
Chiecchio L, Protheroe RK, Ibrahim AH, Cheung KL, Rudduck C, Dagrada GP et al. Deletion of chromosome 13 detected by conventional cytogenetics is a critical prognostic factor in myeloma. Leukemia 2006; 20: 1610–1617.
Gutierrez NC, Castellanos MV, Martin ML, Mateos MV, Hernandez JM, Fernandez M et al. Prognostic and biological implications of genetic abnormalities in multiple myeloma undergoing autologous stem cell transplantation: t(4;14) is the most relevant adverse prognostic factor, whereas RB deletion as a unique abnormality is not associated with adverse prognosis. Leukemia 2007; 21: 143–150.
Hanamura I, Stewart JP, Huang Y, Zhan F, Santra M, Sawyer JR et al. Frequent gain of chromosome band 1q21 in plasma-cell dyscrasias detected by fluorescence in situ hybridization: incidence increases from MGUS to relapsed myeloma and is related to prognosis and disease progression following tandem stem-cell transplantation. Blood 2006; 108: 1724–1732.
Fonseca R, Van Wier SA, Chng WJ, Ketterling R, Lacy MQ, Dispenzieri A et al. Prognostic value of chromosome 1q21 gain by fluorescent in situ hybridization and increase CKS1B expression in myeloma. Leukemia 2006; 20: 2034–2040.
Fonseca R, Bergsagel PL, Drach J, Shaughnessy J, Gutierrez N, Stewart AK et al. International Myeloma Working Group molecular classification of multiple myeloma: spotlight review. Leukemia 2009; 23: 2210–2221.
Morgan GJ, Davies FE, Gregory WM, Cocks K, Bell SE, Szubert AJ et al. First-line treatment with zoledronic acid as compared with clodronic acid in multiple myeloma (MRC Myeloma IX): a randomised controlled trial. Lancet 2010; 376: 1989–1999.
Nair B, van Rhee F, Shaughnessy Jr JD, Anaissie E, Szymonifka J, Hoering A et al. Superior results of total therapy 3 (2003–33) in gene expression profiling-defined low-risk multiple myeloma confirmed in subsequent trial 2006–66 with VRD maintenance. Blood 2010; 115: 4168–4173.
Ross FM, Chiecchio L, Dagrada G, Protheroe RK, Stockley DM, Harrison CJ et al. The t(14;20) is a poor prognostic factor in myeloma but is associated with long-term stable disease in monoclonal gammopathies of undetermined significance. Haematologica 2010; 95: 1221–1225.
Acknowledgements
Main financial support for the Myeloma IX clinical trial was from UK Medical Research Council, with additional funding in the form of unrestricted educational grants from Novartis, Schering Health Care, Chugai, Pharmion, Celgene and Ortho Biotech. The LLR UKMF Cytogenetics group received financial support from Leukaemia and Lymphoma Research. The Institute of Cancer Research received support from Myeloma UK, Cancer Research UK and the biological research center of the National Institute for Health Research at the Royal Marsden Hospital. The University of Leeds acted as the trial sponsor. We acknowledge the support of the National Institute for Health Research, through the National Cancer Research Network. We thank Rebecca Protheroe, David Stockley, Tim Parker, Hazel Robinson, Elisabet Dachs Cabanas and Christina Rudduck of the LLR UKMF Cytogenetics group for probe preparation and FISH scoring. We also thank staff from the Clinical Trials Research Unit, University of Leeds, for trial co-ordination and data management.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Author contributions
GJM, JAC and GHJ were chief investigators of the MRC Myeloma IX trial. KDB, BAW, CPW and GJM designed research, analyzed data and wrote the paper. JAC, GHJ and FED designed research and wrote the paper. FMR designed research, performed research, analyzed data and wrote the paper. LC, GPD and ZJC performed research. WMG, AJS, SEB and WJT analyzed data.
Supplementary Information accompanies the paper on the Leukemia website
Supplementary information
Rights and permissions
About this article
Cite this article
Boyd, K., Ross, F., Chiecchio, L. et al. A novel prognostic model in myeloma based on co-segregating adverse FISH lesions and the ISS: analysis of patients treated in the MRC Myeloma IX trial. Leukemia 26, 349–355 (2012). https://doi.org/10.1038/leu.2011.204
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2011.204
Keywords
This article is cited by
-
Fc receptor-like 5 (FCRL5)-directed CAR-T cells exhibit antitumor activity against multiple myeloma
Signal Transduction and Targeted Therapy (2024)
-
Alterations in chromosome 1q in multiple myeloma randomized clinical trials: a systematic review
Blood Cancer Journal (2024)
-
1q21+ is associated with poor prognosis in newly diagnosed multiple myeloma patients with extramedullary disease: a retrospective study
Annals of Hematology (2024)
-
Primary analysis of a prospective cohort study of Japanese patients with plasma cell neoplasms in the novel drug era (2016–2021)
International Journal of Hematology (2024)
-
Characterization and application of a lactate and branched chain amino acid metabolism related gene signature in a prognosis risk model for multiple myeloma
Cancer Cell International (2023)