Abstract
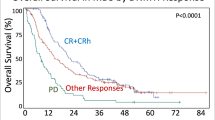
Children with Down syndrome (DS) and acute lymphoblastic leukemia (ALL) have an inferior prognosis compared with non-DS ALL patients. We reviewed methotrexate (MTX)/mercaptopurine (6MP) maintenance therapy data for children with DS treated according to the Nordic Society of Pediatric Hematology and Oncology (NOPHO) ALL92 or the NOPHO ALL2000 protocols between 1992 and 2007. The 5-year event-free survival probability (pEFS5 yr) for the 66 DS patients was inferior to the 2602 non-DS patients (0.50±0.07 vs 0.77±0.01 (P<0.001)). The 48 DS patients in first remission at the beginning of maintenance therapy had pEFS10 yr below that of the 522 non-DS control patients (pEFS10 yr: 0.58 (95% confidence interval (CI) 0.43–0.77) vs 0.83 (95% CI 0.80–0.86), respectively (P<0.0001)). The DS patients received lower median doses of MTX (median: 11.8 vs 15.4 (P<0.0001)) and 6MP (median: 43.6 vs 59.4 (P<0.0001)). In Cox regression analysis, male gender, presence of DS and high median maintenance therapy white blood cell levels (mWBC) were associated with increased risk for relapse. DS-ALL patients with mWBC above or below 3.5 × 109/l (protocol target) had pEFS10 yr of 0.31 and 0.72 (P=0.02), and the mWBC hazard ratio for DS-ALL patients was 2.0 (P<0.0005). We conclude that insufficient treatment intensity during maintenance therapy of DS-ALL patients may contribute to their poor prognosis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Hasle H . Pattern of malignant disorders in individuals with Down’s syndrome. Lancet Oncol 2001; 2: 429–436.
Roizen NJ, Amarose AP . Hematologic abnormalities in children with Down syndrome. Am J Med Genet 1993; 46: 510–512.
Lange B . The management of neoplastic disorders of haematopoiesis in children with Down’s syndrome. Br J Haematol 2000; 110: 512–524.
Malinge S, Izraeli S, Crispino JD . Insights into the manifestations, outcomes, and mechanisms of leukemogenesis in Down syndrome. Blood 2009; 113: 2619–2628.
Zeller B, Gustafsson G, Forestier E, Abrahamsson J, Clausen N, Heldrup J et al. Acute leukaemia in children with Down syndrome: a population-based Nordic study. Br J Haematol 2005; 128: 797–804.
Bassal M, La MK, Whitlock JA, Sather HN, Heerema NA, Gaynon PS et al. Lymphoblast biology and outcome among children with Down syndrome and ALL treated on CCG-1952. Pediatr Blood Cancer 2005; 44: 21–28.
Chessells JM, Harrison G, Richards SM, Bailey CC, Hill FG, Gibson BE et al. Down’s syndrome and acute lymphoblastic leukaemia: clinical features and response to treatment. Arch Dis Child 2001; 85: 321–325.
Levitt GA, Stiller CA, Chessells JM . Prognosis of Down’s syndrome with acute leukaemia. Arch Dis Child 1990; 65: 212–216.
Maloney KW, Carroll WL, Carroll AJ, Devidas M, Borowitz MJ, Martin PL et al. Down syndrome childhood acute lymphoblastic leukemia has a unique spectrum of sentinel cytogenetic lesions that influences treatment outcome: a report from the Children’s Oncology Group. Blood 2010; 116: 1045–1050.
Rabin KR, Whitlock JA . Malignancy in children with trisomy 21. Oncologist 2009; 14: 164–173.
Shah N, Al-Ahmari A, Al-Yamani A, Dupuis L, Stephens D, Hitzler J . Outcome and toxicity of chemotherapy for acute lymphoblastic leukemia in children with Down syndrome. Pediatr Blood Cancer 2009; 52: 14–19.
Whitlock JA, Sather HN, Gaynon P, Robison LL, Wells RJ, Trigg M et al. Clinical characteristics and outcome of children with Down syndrome and acute lymphoblastic leukemia: a Children’s Cancer Group study. Blood 2005; 106: 4043–4049.
Zwaan CM, Reinhardt D, Hitzler J, Vyas P . Acute leukemias in children with Down syndrome. Hematol Oncol Clin N Am 2010; 24: 19–34.
Forestier E, Izraeli S, Beverloo B, Haas O, Pession A, Michalova K et al. Cytogenetic features of acute lymphoblastic and myeloid leukemias in pediatric patients with Down syndrome: an iBFM-SG study. Blood 2008; 111: 1575–1583.
Hasle H, Clemmensen IH, Mikkelsen M . Risks of leukaemia and solid tumours in individuals with Down’s syndrome. Lancet 2000; 355: 165–169.
Taub JW, Ge Y . Down syndrome, drug metabolism and chromosome 21. Pediatr Blood Cancer 2005; 44: 33–39.
Forestier E, Schmiegelow K . The incidence peaks of the childhood acute leukemias reflect specific cytogenetic aberrations. J Pediatr Hematol Oncol 2006; 28: 486–495.
Blink M, Buitenkamp TD, van den Heuvel-Eibrink MM, Danen-van Oorschot AA, de HV, Reinhardt D et al. Frequency and prognostic implications of JAK 1-3 aberrations in Down syndrome acute lymphoblastic and myeloid leukemia. Leukemia 2011; 25: 1365–1368.
Hertzberg L, Vendramini E, Ganmore I, Cazzaniga G, Schmitz M, Chalker J et al. Down syndrome acute lymphoblastic leukemia, a highly heterogeneous disease in which aberrant expression of CRLF2 is associated with mutated JAK2: a report from the International BFM Study Group. Blood 2010; 115: 1006–1017.
Buitenkamp TD, Mathot RA, de HV, Pieters R, Zwaan CM . Methotrexate-induced side effects are not due to differences in pharmacokinetics in children with Down syndrome and acute lymphoblastic leukemia. Haematologica 2010; 95: 1106–1113.
Schmiegelow K, Bjork O, Glomstein A, Gustafsson G, Keiding N, Kristinsson J et al. Intensification of mercaptopurine/methotrexate maintenance chemotherapy may increase the risk of relapse for some children with acute lymphoblastic leukemia. J Clin Oncol 2003; 21: 1332–1339.
Bohnstedt C, Taskinen M, Zeller B, Bjorgvinsdottir H, Hafsteinsdottir S, Schmiegelow K . Poor treatment compliance in children with Down syndrome and acute lymphoblastic leukemia. J Pediatr Hematol Oncol 2009; 31: 79–80.
Gustafsson G, Schmiegelow K, Forestier E, Clausen N, Glomstein A, Jonmundsson G et al. Improving outcome through two decades in childhood ALL in the Nordic countries: the impact of high-dose methotrexate in the reduction of CNS irradiation. Nordic Society of Pediatric Haematology and Oncology (NOPHO). Leukemia 2000; 14: 2267–2275.
Schmiegelow K, Forestier E, Hellebostad M, Heyman M, Kristinsson J, Soderhall S et al. Long-term results of NOPHO ALL-92 and ALL-2000 studies of childhood acute lymphoblastic leukemia. Leukemia 2010; 24: 345–354.
Martinussen TaSTH. Dynamic Regression Models for Survival Data. Springer: Berlin, 2006.
Lin DY, Wei LJ, Ying Z . Model-checking techniques based on cumulative residuals. Biometrics 2002; 58: 1–12.
Schmiegelow K, Heyman M, Kristinsson J, Mogensen UB, Rosthoj S, Vettenranta K et al. Oral methotrexate/6-mercaptopurine may be superior to a multidrug LSA2L2 maintenance therapy for higher risk childhood acute lymphoblastic leukemia: results from the NOPHO ALL-92 study. J Pediatr Hematol Oncol 2009; 31: 385–392.
Davidsen ML, Dalhoff K, Schmiegelow K . Pharmacogenetics influence treatment efficacy in childhood acute lymphoblastic leukemia. J Pediatr Hematol Oncol 2008; 30: 831–849.
Schmiegelow K . Advances in individual prediction of methotrexate toxicity: a review. Br J Haematol 2009; 146: 489–503.
Arico M, Baruchel A, Bertrand Y, Biondi A, Conter V, Eden T et al. The seventh international childhood acute lymphoblastic leukemia workshop report: Palermo, Italy, January 29–30, 2005. Leukemia 2005; 19: 1145–1152.
Schmiegelow K, Pulczynska MK . White-cell counts in childhood acute lymphoblastic leukemia. Eur J Haematol 1990; 44: 72–74.
Schmiegelow K, Ifversen M . Myelotoxicity, pharmacokinetics, and relapse rate with methotrexate/6-mercaptopurine maintenance therapy of childhood acute lymphoblastic leukemia. Pediatr Hematol Oncol 1996; 13: 433–441.
Prasher VP . Screening of medical problems in adults with Down syndrome. Down Syndrome Res Pract 1994; 2: 59–66.
David O, Fiorucci GC, Tosi MT, Altare F, Valori A, Saracco P et al. Hematological studies in children with Down syndrome. Pediatr Hematol Oncol 1996; 13: 271–275.
Skarby TV, Anderson H, Heldrup J, Kanerva JA, Seidel H, Schmiegelow K . High leucovorin doses during high-dose methotrexate treatment may reduce the cure rate in childhood acute lymphoblastic leukemia. Leukemia 2006; 20: 1955–1962.
Peeters MA, Megarbane A, Cattaneo F, Rethore MO, Lejeune J . Differences in purine metabolism in patients with Down’s syndrome. J Intellect Disabil Res 1993; 37 (Part 6): 491–505.
Peeters MA, Lejeune J . Beneficial effect of 6-mercaptopurine on the mitotic index of trisomy 21 lymphocytes. Implications for future research. Ann Genet 1989; 32: 21–25.
Brodsky G, Barnes T, Bleskan J, Becker L, Cox M, Patterson D . The human GARS-AIRS-GART gene encodes two proteins which are differentially expressed during human brain development and temporally overexpressed in cerebellum of individuals with Down syndrome. Hum Mol Genet 1997; 6: 2043–2050.
Hedeland RL, Hvidt K, Nersting J, Rosthoj S, Dalhoff K, Lausen B et al. DNA incorporation of 6-thioguanine nucleotides during maintenance therapy of childhood acute lymphoblastic leukaemia and non-Hodgkin lymphoma. Cancer Chemother Pharmacol 2010; 66: 485–491.
Caver TE, Slobod KS, Flynn PM, Behm FG, Hudson MM, Turner EV et al. Profound abnormality of the B/T lymphocyte ratio during chemotherapy for pediatric acute lymphoblastic leukemia. Leukemia 1998; 12: 619–622.
Nygaard U, Toft N, Schmiegelow K . Methylated metabolites of 6-mercaptopurine are associated with hepatotoxicity. Clin Pharmacol Ther 2004; 75: 274–281.
Schmiegelow M, Hertz H, Schmiegelow K, Holm K, Muller J . Insulin-like growth factor-I and insulin-like growth factor binding protein-3 during maintenance chemotherapy of acute lymphoblastic leukemia in children. J Pediatr Hematol Oncol 1999; 21: 268–273.
Gregory L, Williams R, Thompson E . Leucocyte function in Down’s syndrome and acute leukaemia. Lancet 1972; 1: 1359–1361.
Acknowledgements
This study has received financial support from: The Danish Cancer Society (Grant nos: 91-048, 92-017, 93-017, 95-100-28, R19-A984), The Otto Christensen Foundation, The Swedish Childhood Cancer Foundation (Grant nos. 53/91, 62/94, 72/96, 98/59), The Lundbeck Foundation (Grant no. 38/99) and The Danish Childhood Cancer Foundation.
Author contributions
CB designed the study, collected data, analyzed data and drafted the paper; ML drafted the paper; SR analyzed data; BZ collected data; MT collected data; SH collected data; HB collected data; MH collected data; and KS designed the study, collected data, analyzed data and drafted the paper. All authors approved the final manuscript.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bohnstedt, C., Levinsen, M., Rosthøj, S. et al. Physicians compliance during maintenance therapy in children with Down syndrome and acute lymphoblastic leukemia. Leukemia 27, 866–870 (2013). https://doi.org/10.1038/leu.2012.325
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2012.325
Keywords
This article is cited by
-
Maintenance Treatment in Acute Lymphoblastic Leukemia: A Clinical Primer
Indian Journal of Pediatrics (2024)
-
Acute lymphoblastic leukemia and down syndrome: 6-mercaptopurine and methotrexate metabolites during maintenance therapy
Leukemia (2021)
-
The biology, pathogenesis and clinical aspects of acute lymphoblastic leukemia in children with Down syndrome
Leukemia (2016)
-
Clinical and genetic features of pediatric acute lymphoblastic leukemia in Down syndrome in the Nordic countries
Journal of Hematology & Oncology (2014)