Abstract
The risk of death by suicide in individuals with obsessive–compulsive disorder (OCD) is largely unknown. Previous studies have been small and methodologically flawed. We analyzed data from the Swedish national registers to estimate the risk of suicide in OCD and identify the risk and protective factors associated with suicidal behavior in this group. We used a matched case–cohort design to estimate the risk of deaths by suicide and attempted suicide in individuals diagnosed with OCD, compared with matched general population controls (1:10). Cox regression models were used to study predictors of suicidal behavior. We identified 36 788 OCD patients in the Swedish National Patient Register between 1969 and 2013. Of these, 545 had died by suicide and 4297 had attempted suicide. In unadjusted models, individuals with OCD had an increased risk of both dying by suicide (odds ratio (OR)=9.83 (95% confidence interval (CI), 8.72–11.08)) and attempting suicide (OR=5.45 (95% CI, 5.24–5.67)), compared with matched controls. After adjusting for psychiatric comorbidities, the risk was reduced but remained substantial for both death by suicide and attempted suicide. Within the OCD cohort, a previous suicide attempt was the strongest predictor of death by suicide. Having a comorbid personality or substance use disorder also increased the risk of suicide. Being a woman, higher parental education and having a comorbid anxiety disorder were protective factors. We conclude that patients with OCD are at a substantial risk of suicide. Importantly, this risk remains substantial after adjusting for psychiatric comorbidities. Suicide risk should be carefully monitored in patients with OCD.
Similar content being viewed by others
Introduction
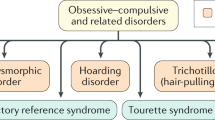
Suicide is a major public health problem with an estimated global burden of more than 800 000 deaths per year, accounting for 1.4% of all deaths worldwide.1 Individuals with mental health conditions are at high risk of dying by suicide and attempting suicide,2, 3 with about 90% of people who kill themselves considered to suffer from a psychiatric disorder.4 Surprisingly, little attention has been paid to the risk of suicide in obsessive–compulsive disorder (OCD), one of the most common and disabling mental disorders.5 OCD has a lifetime prevalence of approximately 2% in the general population,5 often runs a chronic course and is associated with substantial reductions in quality of life.6 OCD is generally accompanied by other psychiatric disorders, with comorbidity rates as high as 90%,5 that further contribute to the burden associated with the disorder.7
Historically, patients with OCD have been considered to be at a relatively low risk of dying by suicide.8, 9, 10 However, this appreciation derives from a small number of modestly sized studies, generally conducted in specialist clinics, which were not only underpowered to study deaths by suicide (a relatively rare event) but also subject to potential selection biases (patients with OCD seen in specialist clinics are typically more severe).11, 12 In addition, these studies have typically included short follow-up times,12 probably insufficient to detect the true risk of suicide in OCD. A meta-analysis established the suicide risk in OCD to be 10 times higher than expected, but these conclusions were based on two single studies including a combined total of three deaths by suicide.13 A recent epidemiological study concluded that individuals with OCD (n=10 155) were three times more likely to die by suicide than population controls.14 However, this figure was also based on a small number of suicide cases (44 cases of unnatural causes of death were reported, including deaths by suicide, accidents and homicides). Therefore, more accurate and unbiased estimates of death by suicide in OCD are needed.
Compared with deaths by suicide, suicide attempts have been more extensively studied in the OCD literature. In a large epidemiological study in the United States (n=18 571), Hollander and colleagues15 reported that OCD sufferers without psychiatric comorbidity (n=140) had a significantly higher rate of self-reported lifetime suicide attempts compared with individuals without a mental disorder (3.6 vs 0.9%, odds ratio (OR)=3.2), while OCD cases with psychiatric comorbidity (n=266) had an even higher rate of lifetime suicide attempts than individuals with other mental disorders (15.0 vs 7.0%; OR=2.2). Torres and colleagues16 identified 114 individuals with OCD in the British National Psychiatric Morbidity Survey of 2000—comprising 8580 individuals—and observed that 25% of OCD cases had self-reported at least one previous suicide attempt. In addition, studies conducted in specialist clinics have reported rates of suicide attempts ranging from 3 to 27%.12, 17, 18, 19 However, as concluded in a recent meta-analysis, the methodological quality of the previous literature on suicidal behavior in OCD has generally been poor.20
In an attempt to provide more accurate estimates of risks of suicide and attempted suicide in OCD, we analyzed data from the Swedish national registers, including more than 36 000 individuals diagnosed with OCD over four decades (1969–2013). Specifically, we aimed to (i) determine the risk of deaths by suicide and attempted suicide in individuals with OCD, compared with population-matched controls; (ii) determine whether OCD itself is associated with suicidal behavior, after adjusting for comorbid psychiatric disorders; and (iii) identify predictors associated with suicidal behavior among individuals with OCD.
Materials and Methods
The study was approved by the Regional Ethical Review Board in Stockholm (reference number 2013/862-31/5). The requirement for informed consent was waived because the study was register-based and the included individuals were not identifiable at any time.
National registers
Using the unique national identification numbers assigned to Swedish citizens as key,21 we linked several Swedish nationwide population-based registers. The National Patient Register (NPR) includes diagnostic information on individuals admitted to a Swedish hospital since 1969. From 2001, the NPR also contains data on outpatient consultations in specialized care.22 Diagnoses are based on the International Classification of Diseases (ICD), eighth (ICD-8; 1969–1986), ninth (ICD-9; 1987–1996) and tenth (ICD-10; 1997–2013) revisions. The Cause of Death Register contains a record of all deaths in Sweden since 1952, with compulsory reporting nationwide. Each record contains the date of death and codes for causes of death, also in accordance to ICD codes. The Cause of Death Register covers more than 99% of all deaths in Swedish residents, including those occurring abroad, resulting in minimal loss of information.23 Demographic and socioeconomic data were derived from the Swedish Register of Total Population with supplementy data from the Education Register.
Variables
Patients with an OCD diagnosis were identified from the NPR (ICD-8 code 300.3; ICD-9 code 300D; ICD-10 code F42) by having at least one record of inpatient or outpatient care between 1 January 1969 and 31 December 2013. Patients with at least one inpatient record were classed as inpatients, while the remaining were classed as outpatients. ICD codes for OCD have been previously validated by comparing registered diagnoses and information in clinical records. ICD-10 codes have excellent inter-rater reliability and validity, with a positive predictive value of 0.91–0.96. ICD-8 and ICD-9 codes for OCD have moderate validity (positive predictive value=0.55 and 0.64, respectively).24 Information on other lifetime psychiatric disorders was also obtained from the NPR. Comorbid diagnoses were grouped into affective disorders, psychotic disorders, personality disorders, substance use disorders, anxiety disorders and ‘other disorders’ (including reaction to severe stress, adjustment, dissociative, somatoform and other neurotic disorders; for specific ICD codes, see Supplementary Material).
Suicidal behavior was defined as a record of death by suicide (identified through the Cause of Death Register) or lifetime suicide attempts (hospital admissions or outpatient consultations in specialized care due to suicide attempts identified through the NPR). To avoid underestimation of suicidal behavior rates and be consistent with recent suicide research,25, 26 we included both certain and undetermined causes in our definitions of death by suicide and attempted suicide as follows: ‘suicide and self-inflicted injury’ (ICD-8 and ICD-9 codes E950-E959); ‘intentional self-harm’ (ICD-10 codes X60-X84); ‘injury undetermined whether accidental or purposely inflicted’ (ICD-8 and ICD-9 codes E980-E989) and ‘events of undetermined intent’ (ICD-10 codes Y10-Y34). Methods of death by suicide and attempted suicide were classified according to ICD grouping codes (for specific ICD codes, see Supplementary Material). Further, methods were classified into self-poisoning (poisoning) and self-injury (remaining methods).27
Parental education level was used as a proxy for the participants’ socioeconomic status.28 The highest attained education among the parents of patients and controls was categorized into three groups: elementary education (⩽9 years), secondary education (10–12 years) and higher education (>12 years).
Statistical analyses
We used a matched case–cohort design to estimate the risk of suicidal behavior in individuals diagnosed with OCD, compared with general population controls. Each OCD patient in the cohort was matched on sex, birth year and county of residence at the time of the first OCD diagnosis with up to 10 general population controls from the Swedish Register of Total Population who had never been diagnosed with OCD by the date of the corresponding cohort member’s date of first diagnosis.
Conditional logistic regression analyses were used to estimate the association between OCD and suicidal behavior and other variables of interest expressed as OR with 95% confidence intervals (CI). In adjusted models, we controlled for parental level of education and different groups of psychiatric comorbidities. For the main outcomes, analyses were stratified by sex, setting (inpatients and outpatients) and ICD version of the first OCD diagnosis received. The specific methods of death by suicide and attempted suicide were also described and frequencies in both cohorts were compared using OR and the corresponding 95% CI.
To study predictors of suicidal behavior, individuals in the OCD cohort were followed-up from the date of the first diagnosis of OCD to the date of the outcomes of interest (death by suicide and attempted suicide), death other than suicide, emigration or end of follow-up (31 December 2013), whichever came first. Cox regression models were used to compute hazard ratios with 95% CI, taking time at risk into account.
All analyses were performed using SAS, version 9.4 for Windows (SAS Institute, Cary, NC, USA).
Results
Descriptive variables
We identified a total of 36 788 cases (20 791 women; 56.52%) diagnosed with OCD in the NPR during the 44-year study period. Of those, 87.00% (n=32 005) were diagnosed with an ICD-10 code. As expected, individuals with OCD had higher rates of other lifetime psychiatric disorders, compared with the general population (Table 1). A total of 76.40% (n=26 634) of the OCD cases had at least one comorbid psychiatric disorder, as compared with 12.09% (n=44 486) of the control group (OR=22.15 (95% CI, 21.53–22.79)). Parents of individuals with OCD and parents of control cases had a similar level of education (Table 1).
Risk of death by suicide and attempted suicide
In the 44-year study period, 545 individuals (1.48%) from the OCD cohort had died by suicide, and 4297 (11.68%) had attempted suicide at least once. Individuals with OCD had an increased risk of both dying by suicide and attempting suicide compared with the matched controls (OR=9.83 (95% CI, 8.72–11.08) and OR=5.45 (95% CI, 5.24–5.67), respectively; Table 1). When adjusting for psychiatric comorbidities, the risk of dying by suicide was slightly reduced—especially when substance use disorders and affective disorders were taken into account—but remained substantial (ORs ranging from 7.49 to 9.23). On the other hand, the risk of attempted suicide was substantially reduced, although not eliminated, when adjusting for comorbidities (ORs ranging from 1.90 to 4.21). Adjusting for parental level of education did not change the risk estimates (Table 2).
Two hundred and thirty-seven (43.49%) of the individuals from the OCD cohort who died by suicide did not have any other recorded psychiatric comorbidity. Conversely, only 4.14% (n=178) of the OCD cases who had attempted suicide did not have any other registered psychiatric diagnosis. The percentage of recorded comorbidities in those individuals who died by suicide or attempted suicide in the OCD cohort is graphically shown in Figure 1. The risk of dying by suicide for those OCD cases without any recorded comorbidities (n=10 154) was similar to that for the full cohort (OR=13.18 (95% CI, 10.76–16.16)), but their risk for attempted suicide was significantly lower (OR=1.59 (95% CI, 1.36–1.87)).
Number of recorded comorbidities1 in the cohort of patients with obsessive–compulsive disorder (OCD) who died by suicide (left) or attempted suicide (right) during the study period. Note that although most suicide attempters had at least one psychiatric comorbidity, over 40% of patients with OCD who completed suicide did not have any recorded psychiatric comorbidity.1 Six groups of comorbidities are considered: namely, affective disorders, psychotic disorders, personality disorders, substance use disorders, anxiety disorders and ‘other disorders’ (including reaction to severe stress, adjustment, dissociative, somatoform and other neurotic disorders).
Risk in women and men with OCD
Both women and men with OCD had a significantly higher risk of dying by suicide than women and men from the general population. However, this risk was more pronounced for women than men with OCD (ORs=12.25 vs 8.44, respectively; P-value for χ2=0.002). This was also the case when considering suicide attempts; women in the OCD cohort had a higher risk as compared with men (ORs=5.99 vs 4.67, respectively; P-value for χ2<0.0001); this difference was driven by women being more likely to attempt suicide than men in the OCD group, but not in the general population cohort (Table 1). Patients with OCD were approximately 3 years younger than controls at the time of suicide (42.55 vs 45.45 years; P-value for t-test=0.003). On the other hand, patients with OCD were approximately 2 years older than controls when they first attempted suicide (30.31 vs 28.56 years; P-value for t-test<0.001) (Table 1). Individuals with OCD were more likely to have repeated attempts (more than two) than their matched controls (30.30% vs 16.03%, respectively; OR=2.07) (Table 1).
Additional subgroup analyses
As expected, the risk of dying by suicide and attempting suicide in those patients who had been admitted as inpatients at least once (OR=12.05 (95% CI, 10.46–13.88) and OR=10.73 (95% CI, 10.03–11.49), respectively) was significantly higher than in the outpatient group (OR=5.88 (95% CI, 4.65–7.44) and OR=3.90 (95% CI, 3.71–4.10), respectively). The risk of death by suicide was similar across ICD versions (OR ICD-8=10.44 (95% CI, 8.60–12.67); OR ICD-9=9.34 (95% CI, 6.57–13.27); OR ICD-10=9.61 (95% CI, 8.12–11.38)). However, the risk of attempted suicide was higher for those individuals who had received an OCD diagnosis based on ICD-9 codes (ORs=7.60 (95% CI, 6.23–9.26)), compared with those receiving an ICD-8 or an ICD-10 code (OR=4.14 (95% CI, 3.14–5.02) and OR=5.45 (95% CI, 5.23–5.67), respectively).
Methods of suicide and attempted suicide
Among those who died by suicide, the specific methods used differed between the OCD and the control cohorts (Table 3). Although self-poisoning was the most common method of suicide in both groups, it was significantly more frequent in the OCD cohort (OR=4.00 (95% CI, 1.13–4.17)), while self-injury methods were more frequent in the control cohort (OR=0.25 (95% CI, 0.07–0.89)). Similarly, the most common method among those attempting suicide in both groups was also self-poisoning which, again, was significantly more frequent in the OCD cohort (OR=2.33 (95% CI, 1.90–2.87)).
Methods of suicide and attempted suicide were generally similar across genders. However, for the attempts, the magnitude of the effects was different in women and men. For example, self-poisoning was more frequent in OCD vs controls in both genders, but this was more prominent in men (OR=3.49 (95% CI, 2.46–4.96)) than it was in women (OR=1.81 (95% CI, 1.39–2.35)). On the other hand, self-injury was more frequent in both men and women controls, but this difference was only significant for the men (OR=0.50 (95% CI, 0.37–0.68); Supplementary Table S1).
Predictors of death by suicide and suicide attempts
Among the patients in the OCD cohort, 179 of the 545 (32.84%) who died by suicide had record of a previous suicide attempt. A previous suicide attempt was the variable that most increased the risk of subsequent death by suicide (hazard ratio=4.68 (95% CI, 3.65–6.01)). In addition, a comorbid substance use disorder or a personality disorder also increased the risk of death by suicide (hazard ratios=1.82 and 1.40, respectively). Higher parental education, being a woman, a comorbid anxiety disorder or a comorbid disorder from the ‘other disorders’ category were protective factors. Regarding attempted suicides, all examined predictors were found to increase the risk, particularly the comorbidity with substance use disorders (Table 4).
Discussion
In this large register-based study of individuals diagnosed with OCD in Sweden over four decades, we found that the disorder was strongly associated with suicidal behavior. The risk of dying by suicide was approximately ten times higher, and the risk of attempted suicide five times higher, than that of the general population. This risk remained substantial after adjusting for different groups of psychiatric comorbidities that are already known to be associated with suicide. In fact, 43% of the individuals from the OCD cohort who died by suicide did not have any other recorded psychiatric comorbidity. Thus, OCD is associated with an increased risk of death by suicide in its own right, a risk that was previously unappreciated. Our estimates place OCD at a comparable suicide risk with other mental disorders like schizophrenia,29 bipolar disorder30 and attention-deficit hyperactivity disorder,28 and at higher risk than posttraumatic stress disorder31 or alcohol use disorders.32
Importantly, the risk of attempted suicide was substantially reduced, though not entirely eliminated, when the models adjusted for psychiatric comorbidity. This contrasts with deaths by suicide, which were largely independent from such comorbidity. Clinicians should be aware that psychiatric comorbidity is not necessarily a reliable indicator of the actual risk of death by suicide in this group. We did find, however, that comorbid personality and substance use disorders increased the risk of suicide by 40–82%, which is consistent with the high risk associated with these disorders in their own right.2 These particular comorbidities require special attention and monitoring in OCD. In the case of suicide attempts, all psychiatric comorbidities increased the risk, especially substance use and affective disorders. Given the high rates of comorbidity in OCD,5 this becomes particularly relevant. Suicidal thoughts should be explored and frequently monitored in all OCD patients, particularly if comorbidities are present and in patients with previous attempts. A higher level of education was a protective factor for death by suicide but appeared to be a risk factor for attempting suicide. It should be borne in mind that suicide attempts are mostly based on hospitalization and attendance to specialty clinics. Thus, higher education may actually reflect greater likelihood of seeking out services rather than an actual higher risk of suicidal behavior.
Women with OCD were at higher risk of suicide compared with men with OCD, relative to women and men from the general population, respectively. This suggests that women patients with OCD may require extra monitoring and follow-up.
Overall, the methods of suicide in the OCD cohort were similar to those in the general population, with self-poisoning—a method sometimes classified as non-violent33—being the preferred method in both groups. However, the individuals in the OCD cohort, especially the men, used this method more frequently than the population controls. This is in line with a previous investigation looking at 351 consecutive suicides in an urban community34 where anxiety disorders were also associated with non-violent methods, including overdose. As approximately 85% of the patients with OCD in the Swedish national registers are on psychotropic medication,35 we speculate that the more frequent use of self-poisoning in the OCD cohort may be related to the ready availability of psychotropic medication in this group. Patients with OCD were less likely to use violent methods of suicide, which may be consistent with the particular personality profile of this patient group, typically described as ‘harm avoidant’.36
In line with the available suicide literature,2 a previous suicide attempt was the main predictor of dying by suicide in the OCD cohort, increasing the risk approximately fivefold. Patients with OCD were also more likely to attempt suicide at multiple occasions (more than two), compared with the population controls. This may provide clinicians with an opportunity to implement risk management strategies to prevent further attempts and potential deaths.
The identification and recognition of risk factors for suicidal behavior in OCD should guide the development of empirically based preventive and intervention strategies aimed at reducing suicide rates in this group. Suicide-prevention strategies, such as restricting access to means (for example, lethal drugs), encouraging self-help, increasing the likelihood of intervention by a third party or education of physicians, for example, have shown to be helpful in reducing the number of suicides.37, 38 These strategies should be tailored to the needs of patients with OCD and implemented in their care plan.
Strengths of this study include the use of a very large population-based cohort of patients with OCD and a four-decade study period long enough to capture the outcomes of interest. There were, however, some limitations. First, because suicide is a sensitive issue, it is likely that it is underreported. Suicide may be misclassified as an accident or another cause of death, especially in those who have not been previously diagnosed with a mental disorder. However, in line with previous studies,25, 39 we tried to minimize this issue by including also the events diagnosed as undetermined causes. Second, whereas ICD-10 codes for OCD have excellent validity and reliability, ICD-8 and ICD-9 codes are somewhat less reliable.24 However, only 13% of our patient cohort were diagnosed using these older codes, and stratified analysis showed that the results were largely comparable across the different ICD editions. Third, because outpatient data were only introduced in the Swedish registers in 2001, during years 1969–2000 the cohort only included individuals whose attempted suicide led to inpatient care, potentially leaving out attempts of lower lethality. In addition, patients with OCD included in the NPR register may not be representative of all OCD cases in the population as the register is biased towards inpatients and only includes specialist care visits and not patients seen in general practitioner clinics. In the same way, the NPR does not include patients diagnosed by professionals other than physicians. These limitations also apply to the identification of the comorbid psychiatric conditions. Finally, despite the large dataset, some of the specific methods of suicidal behavior were rare. Thus, these comparisons based on small numbers should be cautiously interpreted.
Conclusions
OCD is associated with a substantial risk of suicide, which is largely independent from psychiatric comorbidities. Clinicians should be aware that many patients with OCD may successfully complete suicide even in the absence of other psychiatric comorbidities. A previous suicide attempt was the strongest predictor of dying by suicide in individuals with OCD. Poisoning was the most frequent method used, perhaps because of the availability of prescription drugs. OCD should be added to the list of psychiatric disorders that are known to increase the risk of suicide in their own right. Suicide risk needs to be carefully monitored in these patients, particularly in those who have previously attempted suicide. Our results represent a first step towards the design of preventive and interventional strategies aiming to prevent fatal consequences in this group.
References
World Health Organization. Preventing Suicide: A Global Imperative. World Health Organization: Luxembourg, 2014.
Hawton K, van Heeringen K . Suicide. Lancet 2009; 373: 1372–1381.
Nock MK, Hwang I, Sampson NA, Kessler RC . Mental disorders, comorbidity and suicidal behavior: results from the National Comorbidity Survey Replication. Mol Psychiatr 2010; 15: 868–876.
Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM . Psychological autopsy studies of suicide: a systematic review. Psychol Med 2003; 33: 395–405.
Ruscio AM, Stein DJ, Chiu WT, Kessler RC . The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatr 2010; 15: 53–63.
Moritz S . A review on quality of life and depression in obsessive-compulsive disorder. CNS Spectr 2008; 13: 16–22.
Lochner C, Fineberg NA, Zohar J, van Ameringen M, Juven-Wetzler A, Altamura AC et al. Comorbidity in obsessive-compulsive disorder (OCD): a report from the International College of Obsessive-Compulsive Spectrum Disorders (ICOCS). Compr Psychiat 2014; 55: 1513–1519.
Coryell W . Obsessive-compulsive disorder and primary unipolar depression. Comparisons of background, family history, course, and mortality. J Nerv Ment Dis 1981; 169: 220–224.
Goodwin DW, Guze SB, Robins E . Follow-up studies in obsessional neurosis. Arch Gen Psychiat 1969; 20: 182–187.
Kringlen E . Obsessional neurotics: a long-term follow-up. Brit J Psychiat 1965; 111: 709–722.
Hay P, Sachdev P, Cumming S, Smith JS, Lee T, Kitchener P et al. Treatment of obsessive-compulsive disorder by psychosurgery. Acta Psychiat Scand 1993; 87: 197–207.
Alonso P, Segalas C, Real E, Pertusa A, Labad J, Jimenez-Murcia S et al. Suicide in patients treated for obsessive-compulsive disorder: a prospective follow-up study. J Affect Disorders 2010; 124: 300–308.
Harris EC, Barraclough B . Suicide as an outcome for mental disorders - A meta-analysis. Brit J Psychiat 1997; 170: 205–228.
Meier SM, Mattheisen M, Mors O, Schendel DE, Mortensen PB, Plessen KJ . Mortality among persons with obsessive-compulsive disorder in Denmark. JAMA Psychiatry 2016; 73: 268–274.
Hollander E, Greenwald S, Neville D, Johnson J, Hornig CD, Weissman MM . Uncomplicated and comorbid obsessive-compulsive disorder in an epidemiologic sample. Depress Anxiety 1996; 4: 111–119.
Torres AR, Prince MJ, Bebbington PE, Bhugra D, Brugha TS, Farrell M et al. Obsessive-compulsive disorder: prevalence, comorbidity, impact, and help-seeking in the British National Psychiatric Morbidity Survey of 2000. Am J Psychiatry 2006; 163: 1978–1985.
Koran LM, Thienemann ML, Davenport R . Quality of life for patients with obsessive-compulsive disorder. Am J Psychiatry 1996; 153: 783–788.
Kamath P, Reddy YC, Kandavel T . Suicidal behavior in obsessive-compulsive disorder. J Clin Psychiatry 2007; 68: 1741–1750.
Torres AR, de Abreu Ramos-Cerqueira AT, Torresan RC, de Souza Domingues M, Hercos AC, Guimaraes AB . Prevalence and associated factors for suicidal ideation and behaviors in obsessive-compulsive disorder. CNS Spectr 2007; 12: 771–778.
Angelakis I, Gooding P, Tarrier N, Panagioti M . Suicidality in obsessive compulsive disorder (OCD): a systematic review and meta-analysis. Clin Psychol Rev 2015; 39: 1–15.
Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, Ekbom A . The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol 2009; 24: 659–667.
Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C et al. External review and validation of the Swedish national inpatient register. BMC Public Health 2011; 11: 450.
Socialstyrelsen. Cause of Death. 2013. Retrieved from http://www.socialstyrelsen.se/statistics/statisticaldatabase/help/causeofdeath. Accessed April 5th 2016.
Rück C, Larsson KJ, Lind K, Perez-Vigil A, Isomura K, Sariaslan A et al. Validity and reliability of chronic tic disorder and obsessive-compulsive disorder diagnoses in the Swedish National Patient Register. BMJ Open 2015; 5: e007520.
Neeleman J, Wessely S . Changes in classification of suicide in England and Wales: time trends and associations with coroners' professional backgrounds. Psychol Med 1997; 27: 467–472.
Runeson B, Tidemalm D, Dahlin M, Lichtenstein P, Langstrom N . Method of attempted suicide as predictor of subsequent successful suicide: national long term cohort study. BMJ 2010; 341: c3222.
Runeson B, Haglund A, Lichtenstein P, Tidemalm D . Suicide risk after nonfatal self-harm: A National Cohort Study, 2000–2008. J Clin Psychiatry 2015; 77: 240–246.
Ljung T, Chen Q, Lichtenstein P, Larsson H . Common etiological factors of attention-deficit/hyperactivity disorder and suicidal behavior: a population-based study in Sweden. JAMA Psychiatry 2014; 71: 958–964.
Heila H, Haukka J, Suvisaari J, Lonnqvist J . Mortality among patients with schizophrenia and reduced psychiatric hospital care. Psychol Med 2005; 35: 725–732.
Osborn D, Levy G, Nazareth I, King M . Suicide and severe mental illnesses. Cohort study within the UK general practice research database. Schizophr Res 2008; 99: 134–138.
Gradus JL, Qin P, Lincoln AK, Miller M, Lawler E, Sorensen HT et al. Posttraumatic stress disorder and completed suicide. Am J Epidemiol 2010; 171: 721–727.
Flensborg-Madsen T, Knop J, Mortensen EL, Becker U, Sher L, Gronbaek M . Alcohol use disorders increase the risk of completed suicide - Irrespective of other psychiatric disorders. A longitudinal cohort study. Psychiatry Res 2009; 167: 123–130.
Traskman L, Asberg M, Bertilsson L, Sjostrand L . Monoamine metabolites in CSF and suicidal behavior. Arch Gen Psychiatry 1981; 38: 631–636.
McGirr A, Seguin M, Renaud J, Benkelfat C, Alda M, Turecki G . Gender and risk factors for suicide: evidence for heterogeneity in predisposing mechanisms in a psychological autopsy study. J Clin Psychiatry 2006; 67: 1612–1617.
Isomura K, Nordsletten AE, Rück C, Ivarsson T, Ljung R, Larsson H et al. Pharmacoepidemiology of obsessive-compulsive disorder: a Swedish Nationwide Cohort Study. Eur Neuropsychopharmacology 2016; 26: 693–704.
Kim SJ, Kang JI, Kim CH . Temperament and character in subjects with obsessive-compulsive disorder. Compr Psychiatry 2009; 50: 567–572.
Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A et al. Suicide prevention strategies: a systematic review. JAMA 2005; 294: 2064–2074.
Pirkis J, San Too L, Spittal MJ, Krysinska K, Robinson J, Cheung YTD . Interventions to reduce suicides at suicide hotspots: a systematic review and meta-analysis. Lancet Psychiatry 2015; 2: 994–1001.
Haglund A, Tidemalm D, Jokinen J, Langstrom N, Lichtenstein P, Fazel S et al. Suicide after release from prison: a population-based cohort study from Sweden. J Clin Psychiatry 2014; 75: 1047–1053.
Acknowledgements
We thank the board of the Swedish OCD Association (Svenska OCD Förbundet) for their endorsement of this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Fernández de la Cruz reports grants from the David and Astrid Hagelén Foundation and the Swedish Research Council for Health, Working Life and Welfare (FORTE grant number 2015-00569). Dr Rydell reports a grant from the Swedish Research Council for Health, Working Life and Welfare (FORTE grant number 2015-00075). Prof D'Onofrio reports grants from the American Foundation for Suicide Prevention and the Indiana Clinical and Translational Sciences Institute (Networks, Complex System and Health Project Development Team). Mr Brander reports a scholarship from KID-funding (Karolinska Institutet PhD stipend). Dr Rück reports a grant from the Swedish Research Council (K2013-61P-22168). Prof Lichtenstein has served as a speaker for Medice. Prof Larsson reports a grant from Shire and has served as a speaker for Eli-Lilly and Shire. Prof Runeson and Prof Mataix-Cols have nothing to disclose. Funders had no role in study design, data collection, data management, data analysis, data interpretation or writing of the report.
Additional information
Supplementary Information accompanies the paper on the Molecular Psychiatry website
Supplementary information
PowerPoint slides
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Fernández de la Cruz, L., Rydell, M., Runeson, B. et al. Suicide in obsessive–compulsive disorder: a population-based study of 36 788 Swedish patients. Mol Psychiatry 22, 1626–1632 (2017). https://doi.org/10.1038/mp.2016.115
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mp.2016.115
This article is cited by
-
General somatic health and lifestyle habits in individuals with obsessive- compulsive disorder: an international survey
BMC Psychiatry (2024)
-
A multimodal meta-analysis of regional functional and structural brain abnormalities in obsessive–compulsive disorder
European Archives of Psychiatry and Clinical Neuroscience (2024)
-
Suicidal behavior across a broad range of psychiatric disorders
Molecular Psychiatry (2023)
-
The Cost of Obsessive–Compulsive Disorder in Swedish Youth
Child Psychiatry & Human Development (2023)
-
Genetic and environmental sources of familial coaggregation of obsessive−compulsive disorder and suicidal behavior: a population-based birth cohort and family study
Molecular Psychiatry (2021)