Abstract
Innate cells are responsible for the rapid recognition of infection and mediate essential mechanisms of pathogen elimination, and also facilitate adaptive immune responses. We review here the numerous intricate interactions among innate cells that initiate protective immunity. The efficient eradication of pathogens depends on the coordinated actions of multiple cells, including innate cells and epithelial cells. Rather than acting as isolated effector cells, innate cells are in constant communication with other responding cells of the immune system, locally and distally. These interactions are critically important for the efficient control of primary infections as well for the development of 'trained' innate cells that facilitate the rapid elimination of homologous or heterologous infections.
Similar content being viewed by others
Main
Host defense in vertebrates utilizes an array of receptors on cells of the immune system to recognize invading pathogens. These include antigen-specific receptors, expressed by B cells and T cells, which detect specific epitopes (antigens). In addition, specific groups of pathogens are recognized via pattern-recognition receptors (PRRs) expressed chiefly by cells of the innate immune system. PRRs act as sensors of microbes, detecting conserved microbe-associated molecular patterns (MAMPs). Well-characterized PRRs include TLRs and CLRs, as well as cytoplasmic NLRs. Danger-associated molecular patterns (DAMPs) released by damaged host cells also bind PRRs and contribute to the overall immune response. Although less well characterized, identified DAMPs include TFF2 (ref. 1) and adenosine2, which, upon binding to their respective PRR, can trigger the release of alarmins, including interleukin 33 (IL-33)1,2, a potent inducer of type 2 immune responses3. Chitinase-like proteins released by damaged epithelial cells can also function as DAMPs, triggering the production of IL-17, which contributes to the type 2 immune response4. These two levels of specificity, antigen-dependent and PRR, are essential for the induction of protective immunity. PRR signaling is particularly important in determining the initiation of specific immunological modules and thereby tailors the response to the particular group of pathogens invading the host. For example, certain microbial pathogens, including many viruses, bacteria and intracellular parasites, trigger type 1 immunity, with elevations in the expression of specific cytokines, including IL-17 and interferon-γ (IFN-γ). In contrast, multicellular pathogens, including helminths, stimulate a type 2 response, with elevations in IL-4 and IL-13 (ref. 3). As the specific ligand recognized by cells of the innate immune system does not have to be processed or presented by antigen-presenting cells, the innate response develops more quickly than the adaptive response does. Thus, the type of immune response that develops during infection is often determined before the activation of T cells and B cells. Therefore, the events in specific tissue microenvironments that initiate an innate immune response, including interactions between cells of the innate immune system, are critical for understanding the nature of the immune response. Here we discuss the initiating events in specific tissue microenvironments that determine the nature of the innate immune response. We focus on key interactions involving myeloid cell lineages and also innate lymphoid cells (ILCs) in the setting of bacterial, fungal and parasitic infections, but we exclude the topic of viral diseases, which has already been reviewed elsewhere5,6,7,8,9,10.
Coordinating innate immune responses
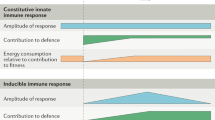
Cells of the innate immune system include both myeloid cells and ILCs. Like T cells and B cells, ILCs, including natural killer (NK) cells, develop from common lymphoid progenitor cells. However, they do not express antigen-specific receptors. Mature ILCs include group 1, group 2 and group 3 ILCs11. Myeloid cells include monocytes, macrophages, dendritic cells and granulocytes (eosinophils, basophils, and neutrophils). Although historically macrophages and neutrophils were associated with microbial infections, and basophils, mast cells and eosinophils were associated with helminth infections, it is increasingly clear that each of these different cell types is often activated in response to a broad range of microbial and multicellular pathogens. For example, macrophages are classically activated (M1) in response to many microbial pathogens but are alternatively activated (M2) in response to helminths. In fact, macrophages can exhibit an even broader spectrum of activation depending on the particular stimuli12. It is thus important to consider both the cell lineage and the specific activation state when assessing the function of a cell of the immune system in response to a specific pathogen. Different cell lineages have distinct chromatin signatures, which helps to define their function. However, during infection, signaling through specific cell sensors, including PRRs, affects transcription and can also have epigenetic effects. In addition to transcriptional regulation, post-transcriptional regulatory controls are also involved at specific checkpoints, such as protein translation and the splicing, polyadenylation and stability of mRNA13. All of these probably contribute to the specificity of immunological gene regulation in innate cell lineages following their activation during infection. Therefore, both the cell lineage and the specific signaling pathways that trigger activation in response to a particular pathogen need to be considered. It can be misleading to consider one cell population of the innate immune system as having a predominant effect during the response to a pathogen or group of related pathogens. Instead, an emerging model suggests that the innate immune response functions more like an orchestra, with distinct cell lineages of the innate immune system undergoing differential activation, which thereby allows different responses tailored to specific groups of pathogens (Fig. 1).
The entry of pathogens into mucosal surfaces can cause damage to epithelial cells and result in the release of DAMPs. The presence of an invading pathogen is also sensed by cell-surface and cytoplasmic PRRs that detect an array of MAMPs, as well as DAMPs. PRR signaling promotes the differential induction of cytokines by epithelial cells and cells of the innate immune system. Although helminth-specific pathogen-associated molecular patterns are yet to be well characterized, worm-specific excretory and secretory products are sensed by innate cells and contribute to the overall inflammatory milieu. The effector functions of innate cells such as neutrophils and macrophages are activated differentially by the aggregate contributions of DAMPs, pathogen-associated molecular patterns and cytokines, which lead to a tailored immune response for the efficient eradication of pathogens. In the context of type 1 responses, the early induction of IL-12 and IFN-γ induces the activation of M1 macrophages with optimal capacity to contain intracellular pathogens. Similarly, neutrophils activated in a type 1 cytokine milieu acquire a tailored N1 phenotype. In contrast, infection with helminth parasites and the associated tissue damage that they cause promote a distinct inflammatory response that facilitates the differentiation of M2 macrophages and N2 neutrophils. DC, dendritic cell.
Communication and cooperation between cells of the immune system has been understood mainly in the context of cross-regulation of the innate and adaptive immune systems. Far from the initial simplistic view of myeloid cells as simple killers, studies now suggest that a complex network of interactions regulates14 tailored responses to diverse stimulations (Fig. 2). Moreover, exciting evidence now suggests that at least one myeloid cell population, macrophages, are capable of 'memory-like' responses that assist in the rapid elimination of pathogens upon secondary challenge15,16,17.
The entry of pathogens into diverse tissues triggers the production of tissue-derived signals that include cytokines, chemokines and alarmins. These factors can be sensed locally by innate cells as well as remotely in the bone marrow (BM), where a distal response by innate cells is initiated. In a type 1 innate response, dendritic cells secrete IL-12 and thus induce IFN-γ production by NK cells. Monocyte precursor cells can be primed by this inflammatory response in the bone marrow and enter the infected tissue in a 'pre-educated' state. In the infected tissue, monocyte-derived macrophages (mo-MΦ) provide important cues to tissue-resident macrophage (TR MΦ) populations to promote the production of chemokines for the recruitment of other innate cells. Tissue-resident macrophages also engage in communication with epithelial cells, including the secretion of SOCS proteins that help maintain a balanced immune response. Epithelial cells, in turn, are an important source of alarmins and cytokines that shape the response of macrophages and other recruited innate cells, such as neutrophils. Neutrophils shape the responses of other innate cells, including NK cells, and can be a source of regulatory cytokines such as IL-10, as well as 'instructive' cytokines such as IL-1, IL-18, IL-17 and tumor-necrosis factor (TNF). During a type 2 response, similar innate cells interact to orchestrate protection and are activated differentially to produce factors that promote type 2 immunity. Epithelial cells are an important source of DAMPs such as adenosine that trigger release of cytokine alarmins, which then drive the production of type 2 cytokines by cells of the innate immune system. Epithelial cells can also release chitinase-like proteins, which drive the secretion of IL-17 by γδ T cells. IL-17 can recruit neutrophils and potentially enhance their production of type 2 cytokines. Thus, interactions among epithelial and innate cells operate locally and distally to coordinate the elicitation of a balanced, protective inflammatory response. NETs, neutrophil extracellular traps.
Macrophages
The understanding of macrophage function has undergone a major transformation fueled in part by technologies that allow lineage-specific and temporal deletion of genes and expression of specific tracking markers. Fate-mapping studies and comprehensive transcriptional profiling have provided evidence in support of the proposal of a distinct origin and function of tissue-resident macrophages18,19,20,21,22. These macrophages are derived from embryonic progenitor cells and are maintained in the periphery without contributions from bone marrow–derived monocytes21,23. They are present at important sites of primary pathogen exposure, such as the airways and intestinal mucosa, and are crucial for the initiation of an inflammatory response24. Tissue-derived macrophages can produce chemokines that recruit monocytes and neutrophils to the site of infection24,25,26. In a published study, during bacterial infection, trafficking of neutrophils within the uroepithelium was possible only after blood monocyte–derived Ly6C+ macrophages 'licensed' tissue-resident macrophages to produce the chemokine CXCL2 (ref. 25). Thus, in this model, tissue-resident macrophages act as sentinels, while recruited macrophages act as helper cells and assist in the 'licensing' of other innate cells and further recruitment of neutrophils25. Mounting evidence suggests that tissue-resident and monocyte-derived macrophages modulate the function of neutrophils by providing stimulatory or inhibitory cues27. Beyond their direct effects on monocytes and neutrophils, tissue-resident macrophages can control other innate cells indirectly via communication with epithelial cells27,28. For example, alveolar macrophages (AMs) communicate with pulmonary epithelial cells via connexin 43–containing gap-junction channels and minimize lung inflammation by limiting neutrophil recruitment28. AMs have also been found to secrete SOCS proteins that act to inhibit inflammatory signaling on airway epithelial cells27. Although the roles of these AM-and-epithelia intercommunication mechanisms in the context of pulmonary infections have yet to be explored, we are tempted to speculate that the eradication of pulmonary pathogens involves mechanisms that override such immunosuppressive signals. Collectively, these studies support a model in which continuous communication of tissue-resident macrophages with the epithelia as well as with recruited monocytes and neutrophils operates to coordinate protective immunity and tissue homeostasis (Fig. 2).
Monocytes and their derivative cells
Ly6C+ inflammatory monocytes in the blood are rapidly recruited to sites of infection and give rise to monocyte-derived macrophages and dendritic cells29. The recruitment of these precursor cells depends on efficient exit from the bone marrow via engagement of the chemokine receptor CCR2 with CCL2, its chief ligand30,31. Ly6C+ inflammatory monocytes and their derivatives are crucial for defense against many pathogens and are an important source of cytokines and chemokines that further recruit neutrophils and inflammatory cells, and they also promote the function of other innate cells29,32,33. Notably, Ly6C+ inflammatory monocytes give rise to monocyte-derived macrophages during infection and can replace tissue-derived macrophages under certain conditions24,29. The cues that 'instruct' the differentiation of monocytic precursor cells into either monocyte-derived macrophages or monocyte-derived dendritic cells are poorly understood but are probably shaped by tissue-derived signals. The importance of tissue-derived signals for macrophage identity has been shown by the adoptive transfer of peritoneal macrophages into the airways, which promotes their acquisition of pulmonary transcriptional signatures34. Similarly, tissue-derived signals stimulate the differentiation of monocytic precursor cells into specific subsets of macrophages. Alternatively, monocyte precursor cells might receive initial instructive signals in the bone marrow, as has been demonstrated after infection with Toxoplasma gondii35. In this model, systemic IL-12 induces the expression of IFN-γ by NK cells that then acts on bone marrow monocyte precursor cells to 'instruct' a regulatory program in the monocytes before their entry into the intestine35. A similarly important role for NK cell–derived IFN-γ has been shown to promote the local differentiation of monocytes and replacement of tissue-resident macrophages by monocyte-derived cells36,37. Thus, innate cell communication occurs among dendritic cells, NK cells and monocytes both at the site of infection and distally in the bone marrow (Fig. 2).
Macrophage activation states and acquired resistance
Both tissue-derived macrophages and monocyte-derived macrophages seem to be able to activate distinct programs in response to infections with specific groups of pathogens. Historically, macrophages were associated mainly with microbial infections, but it is now clear that their ability to become differentially activated makes them important participants in responses to many different groups of pathogens. An essential function of M1 macrophages is phagocytosis, with the associated production of antimicrobial nitric oxide (NO) from imported arginine through the NO-synthase reaction. These highly activated cells utilize aerobic glycolysis to rapidly generate ATP14. In contrast, M2 macrophages are often stimulated during infections with multicellular parasites, with IL-4 and IL-13 being potent inducers of M2 polarization. Rather than using NO production, M2 macrophages instead utilize arginase to metabolize large quantities of arginine to ornithine and urea38. In addition to phagocytosis39,40, M2 macrophages have immunoregulatory properties that function in part through depletion of the local supply of arginine required by effector T cells41 and possibly other neighboring cells of the innate immune system that are arginine auxotrophs. Interestingly, the anti-helminth effector functions of M2 macrophages can also be arginase dependent15,42,43,44, which raises the possibility that depletion of local arginine might also impair invading parasites.
Conventionally, memory responses, the basis of acquired resistance and vaccines, were considered the hallmark of antigen-specific T cells and B cells. Increasing evidence now suggests that cells of the innate immune system can also develop memory-like responses, or so-called 'trained immunity'45,46. PRRs expressed by cells of the innate immune system provide one mechanism for the specificity, albeit not the antigen specificity, of the response. In this model, during initial exposure to the pathogen, cells of the innate immune system are activated through specific PRRs. This activation state is then preserved such that upon subsequent infections, a heightened, more rapidly developing response occurs46. In vitro studies indeed indicate that macrophages stimulated by fungal structures undergo epigenetic remodeling, which stabilizes the transcriptional programs of these memory-like macrophages17, whereas macrophages stimulated by lipopolysaccharide show prolonged epigenetic changes mediated by the transcription factor ATF7 (ref. 47). Such changes in the epigenome could help explain the persistent macrophage phenotypes that have been described in vivo (Fig. 3). In lung macrophages, a long-lived desensitized state, including hypo-responsiveness to TLR ligands, has been observed after infection with influenza virus48. Furthermore, lung macrophages activated during infection with Nippostrongylus brasiliensis can transfer accelerated resistance, as late as 45 days after primary inoculation. Functionally, the helminth-induced (M2) macrophages show enhanced binding to parasites and increased parasite killing15. In future studies, it will be important to determine whether these long-lived in vivo macrophage phenotypes require an inflammatory milieu to persist or are instead sufficiently stabilized to retain this memory-like phenotype independently. Published studies indicate that NK cells also have memory-like characteristics, with epigenetic modifications contributing to phenotype stabilization and enhanced function, which could potentially have a role in controlling the latent reactivation of virus49. 'Trained' innate immunity might also be the basis of many nonspecific effects of vaccines. Vaccination of healthy volunteers with bacillus Calmette-Guérin results in enhanced and prolonged blood monocyte cytokine production in response to unrelated bacterial and fungal pathogens, which persists as long as 3 months after vaccination and is dependent on signaling via Nod2 PRRs16. Such non–pathogen-specific immunity has also been observed in infants vaccinated with bacillus Calmette-Guérin, in whom heterologous challenge results in enhanced cytokine responses by cells of the innate immune system50.
A primary exposure to infection can 'instruct' the formation of trained populations of innate cells that provide enhanced protection upon secondary challenge with the same pathogen (homologous protection) or a different type of pathogen (heterologous protection). Epigenetic modifications in macrophages may form the basis of this innate memory response, although it is possible that post-transcriptional mechanisms are also important. Triggering of PRRs on responding macrophages is crucial for the induction of epigenetic changes in the trained cell. PRRs can be activated by diverse MAMPs, as well as by endogenous DAMPs released by damaged cells. Important DAMPs in this process include adenosine (ATP), TFF2 and chitinase-like proteins. It is likely that the training of innate cells is also the result of the integration of immunological signals provided by the interactions with other innate cells. The structure presented here for TFF2 is that of the representative trefoil motif–containing protein PSP ('pancreatic spasmolytic polypeptide'; PDB accession code 2PSP); the representative chitinase-like protein structure presented here is that of Ym1 (PDB accession code 1E9L).
Regulation of innate responses by neutrophils
Although traditionally viewed as short-lived effector cells that mediate the elimination of microbial pathogens, neutrophils have now emerged as important regulators of innate and adaptive immunity51. Neutrophils can serve as an important source of cytokines and chemokines to activate and recruit other cells of the immune system52,53,54. Moreover, similar to other cells of the immune system, such as macrophages, neutrophils can be polarized into 'N1' or 'N2' subsets with differential abilities to produce cytokines. For example, N1 neutrophils express IL-12 in response to lipopolysaccharide, and N2 neutrophils express IL-33 and IL-13 in response to helminth infection15. Neutrophils can also produce IL-17 in response to fungal stimulation54 or IFN-γ in the context of bacterial or T. gondii infection55. Intriguingly, the interactions of neutrophils with other innate cells can have long-term consequences. In one study, depletion of neutrophils during a primary exposure to helminth infection failed to induce a protective, long-lived macrophage response in the lungs15. The mechanisms by which neutrophils influence the activity of other innate cells are diverse and depend on the particular inflammatory milieu. Neutrophils and macrophages have been found to act cooperatively during primary responses to Leishmania infection in which neutrophils enhance macrophage activity via tumor-necrosis factor and superoxide production56. Macrophage function and cytokine production can also be enhanced by their interaction with neutrophils via the recognition of neutrophil-derived extracellular traps53. Neutrophils can also aid in the recruitment of cells of the immune system to infected tissue by a novel mechanism that involves the deposition of chemokines that form guiding trails for other cells to follow52. In addition to activating the functions of other innate cells, neutrophils can also dampen immune responses and promote the resolution of inflammation. Localized oxygen consumption by neutrophils has been shown to stabilize the transcription factor HIF in epithelial cells and thus promote the resolution of intestinal inflammation57. Another mechanism of neutrophil-dependent regulation of inflammation is through the production of IL-10 that dampens the responses of dendritic cells, monocytes and macrophages58. Thus, in addition to their well-known effector mechanisms of pathogen eradication, neutrophils can also perform nonredundant regulatory functions by influencing the activities of other cells of the immune system51,59.
Basophils, mast cells and eosinophils
The proliferation of basophils is associated with various helminth infections60,61,62,63,64,65,66. Interestingly, basophils are a major source of IL-4 and can promote type 2 cytokine–mediated inflammation in a pathogen-specific manner following both primary exposure and secondary exposure to helminths65,66,67,68,69,70. For example, studies suggest that although basophils contribute to responses by the TH2 subset of helper T cells following primary infection with Trichuris muris or Trichinella spiralis, they are not contributors following primary infection with N. brasiliensis or Heligmosomoides polygyrus bakeri60,63,69,71,72,73,74. In contrast, basophils have been shown to be critically important in the context of secondary infection with N. brasiliensis or H. polygyrus bakeri71,73,74,75. Furthermore, although the mechanisms through which basophils promote primary immunity to T. muris and T. spiralis remain unknown, studies suggest that basophils promote secondary immunity to N. brasiliensis via their coordinated interactions with tissue-resident macrophage populations75. Specifically, basophils primed with immunoglobulin E infiltrate the skin following secondary exposure to larvae. These basophils then produce IL-4 and interact with skin-resident macrophage populations, which promotes an M2 phenotype, including expression of the classic M2 signature genes Arg1, Chi313 and Pdcd1Ig2 (ref. 75). These basophil-induced M2 macrophage populations then effectively trap parasitic larvae in the skin in a manner dependent on the arginase Arg-1 and thereby inhibit migration of the larvae to the lungs. Depletion of basophils blocks the M2 development of macrophages and the associated inhibition of migration of larvae to the lungs75. Collectively, these data demonstrate that basophils promote secondary immunity to N. brasiliensis via their interactions with skin-resident macrophage populations. Similar to its effect during N. brasiliensis, antibody-mediated depletion of basophils in the context of H. polygyrus bakeri infection results in a reduced capacity to clear worms74. Although the mechanism by which basophils promote immunity to H. polygyrus bakeri remains uncertain, given the importance of M2 macrophages in protective immunity in this system42, we are tempted to speculate that basophils 'instruct' macrophages, as seen during infection with N. brasiliensis. However, further studies are needed to determine if basophils act cooperatively with other cell populations of the innate immune system to promote protective immunity to other helminth parasites. Further findings suggest that basophil-macrophage interactions also contribute to inflammation in a model of allergic disease44,76, which suggests that cross-talk among cells of the innate immune system represents a conserved feature of type 2 inflammation.
In addition to their role in promoting type 2 immunity, basophils also contribute to anti-bacterial-immunity. For example, basophils can recognize and be activated by staphylococcal enterotoxins via antibody-mediated mechanisms77. Further studies have also demonstrated that basophils form basophil-derived extracellular traps that are able to trap and kill bacteria78. However, where anti-microbial basophil responses act together with and/or 'instruct' other cells of the innate immune system remains to be defined.
Similar to basophils, IL-4-expressing mast cells and eosinophils increase in number following many parasitic infections65,66,79,80,81. Mast cells have a critical role in promoting macrophage activation and protective immunity to T. spiralis82. Additional studies have also demonstrated a role for mast cells in optimal innate immune responses and protective immunity to H. polygyrus bakeri and T. muris83. Furthermore, helminth-elicited eosinophil responses are sufficient for the promotion of fat-resident M2 macrophages and glucose tolerance following infection80,81. Collectively, such studies suggest that macrophage-granulocyte cross-talk represents a conserved feature of helminth-induced inflammation.
As do basophils, mast cells and eosinophils can express TLRs and become activated in response to bacterial stimuli84,85,86. For example, stimulation of bone marrow–derived mast cells with Francisella tularenis results in the production of mast cell–derived IL-4. IL-4 produced from stimulated mast cells is sufficient to promote the M2 activation of macrophages and control of the intracellular growth of F. tularenis87. Moreover, patients suffering bacterial infections present with decreased peripheral eosinophil counts85, and it has been demonstrated that eosinophils release extracellular traps that kill Staphylococcus aureus and Escherichia coli85,86. Thus, similar to other granulocyte populations, mast cells and eosinophils possess anti-bacterial qualities that promote protective immunity.
Interactions of macrophages with ILCs
Studies of IL-13 reporter mice have facilitated the identification of a lineage marker–negative, c-Kit+, IL-33 receptor–positive, IL-13+ innate ILC2 population following primary infection of the mice with N. brasiliensis88,89,90. Since their original identification, ILC2 cells have been recognized for their ability to promote type 2 cytokine–mediated immunity and inflammation in the context of various models of allergic inflammation and parasitic infection11,91. Although the mechanisms by which ILC2 cells promote type 2 cytokine–mediated immunity remain to be fully defined, it is well established that these cells directly promote helminth-induced eosinophil responses and contribute to macrophage activation11,91. For example, the activation of ILC2 cells after hookworm infection is sufficient to promote eosinophilia and M2 activation of macrophages that contributes to infection-induced increases in visceral adipose tissue81. Furthermore, it has been demonstrated that ILC2 responses act cooperatively with CD4+ T cells to support the M2 activation of macrophages in the lungs following a secondary challenge with N. brasiliensis92. Finally, studies have also shown that ILC2 cells promote the M2 activation of macrophages and the subsequent induction of protective regulatory T cells93. Collectively, these studies suggest that ILC2 cells promote host-protective responses in part through their crosstalk with eosinophil and macrophage populations.
NK cells have long been known to be the principal innate cells that induce the classical activation of macrophages, monocytes and dendritic cells. Unlike viral infection, in which NK cells sense infected cells through the direct recognition of virus-encoded antigens by activating receptors on their surface94, the activation of NK cells by eukaryotic parasites requires accessory cells such as monocytes, dendritic cells and macrophages95. The microbial activation of mononuclear cells allows the transmission of both soluble signals and membrane-associated signals for the activation of NK cells. In turn, activated NK cells exert cytotoxic activity and produce proinflammatory cytokines that further induce the maturation of monocytic cells into M1 macrophages and dendritic cells. Crosstalk between NK cells and monocytes is mediated principally by the production of IL-12 by the latter cells, which then trigger IFN-γ production by NK cells. The provision of IFN-γ and other accessory signals by NK cells can trigger the further maturation of monocytes into either M1 macrophages or inflammatory dendritic cells. In vitro studies suggest that TLR-stimulated neutrophils release soluble mediators that attract and activate NK cells96. Mature neutrophils are also required for the proper maintenance of NK cells in the bone marrow and periphery97. Neutrophils condition NK cells for enhanced responsiveness to IL-12, cytotoxicity and cytokine production through the caspase-dependent release of IL-1 and IL-18. In turn, NK cells can serve as a crucial source of the cell-signaling molecule GM-CSF during infection to enhance neutrophil effector function98. In addition to the release of these cytokines by neutrophils, inflammasome-mediated activation and release of IL-1 and IL-18 by tissue-resident macrophages and parenchymal cells themselves could provide the initiating signals for the recruitment of NK cells and inflammatory monocytes and foster NK cell–mononuclear cell crosstalk (Fig. 2). Critically, the activation and cytokine production of NK cells is terminated following their lysis or disengagement from their monocytic target cells99. Additionally, IL-10 production provides another layer of negative regulation for the prevention of immunopathology of an otherwise protective type 1 response100. Not much is known about how ILC1 cells differ from NK cells in the way they engage in crosstalk with mononuclear cells, but given the extensive overlap between ILC1 cells and NK cells in their gene-expression and cytokine-secretion patterns101, it is reasonable to assume that ILC1 cells probably interact with myeloid cells very similarly to NK cells.
Analogous to the way NK cells and ILC2 cells act as inducers of the M1 activation of macrophages and M2 activation of macrophages, respectively, crosstalk between ILC3 cells expressing the transcription factor RORγt and inflammatory CCR2+ monocytes also occurs during microbial infection of the intestine102. Newly recruited monocytes differentiate into phenotypically proinflammatory CD11c+ intestinal macrophages within the lamina propria and produce large amounts of IL-1β under the influence of ILC3 cells. IL-1β produced by inflammatory monocytes reciprocally enhances IL-22 production by ILC3 cells to promote resistance to infection. IL-23 produced by microbe-activated dendritic cells can also drive the ILC3 production of IL-22, IL-17, IFN-γ and GM-CSF103. The activation of ILC3 cells by IL-1 and IL-23 and the production of these cytokines probably provide protection against a variety of bacterial, fungal and protozoal pathogens. During homeostasis, microbiota-derived production of IL-1β seems to drive GM-CSF production by ILCs to promote regulatory T cells and oral tolerance104. However, during microbial infection, this balance is tilted toward enhanced production of IL-1 and IL-23, which leads to more production of IL-22 and IL-17. How enteric protozoal, fungal and helminth pathogens perturb this balance by producing shifts in the microbiome, the cytokine milieu and the tissue-regulatory milieu remains a fertile area of investigation.
Conclusions
In this Review, we have emphasized the importance of communication between cells of the innate immune system in determining both the quality and the magnitude of an immune response. In particular, a growing number of studies have indicated that crosstalk between myeloid cell populations provides an essential contribution to the initiation of the immune response. We propose a model in which various granulocytes interact with macrophages to promote macrophage activation (Fig. 4). Macrophages in turn provide signals to granulocytes, which influences their activation as well. Together with ILCs, myeloid cells have a central role in tailoring the immune response and associated effector-cell functions to distinct groups of pathogens. Intrinsic to this model is the ability of individual myeloid cells and ILCs to exhibit different effector functions in response to specific groups of pathogens. Increasing evidence suggests that just as helper T cell subsets differentiate from a common helper T cell progenitor, each of these cells of the innate immune system is also programmed by the immunological milieu to activate specific signaling-pathway modules that mediate the expression of distinct cell-surface and secreted molecules. Future studies should also investigate the interactions between cells of the adaptive and innate immune systems that coordinate tissue-specific immune responses through the positive amplification of common effector programs and also, notably, antagonistic regulatory interactions105,106. How are these lineage- and signaling-induced determinants of the activation of cells of the innate immune system controlled at the molecular level? Is epigenetic chromatin modification of primary importance, or are more downstream mechanisms, such as those mediated by non-coding regulatory RNAs, also involved? Answers to such questions involving communication between cells of the innate immune system might provide fundamental insights into how to perturb the innate immune response therapeutically by targeting specific signaling pathways that can enhance resistance and/or prevent harmful inflammatory responses.
Various cell populations of the innate immune system engage in crosstalk with macrophages. Macrophages are crucial effectors for the defense against many pathogens. These cells can be activated differentially upon infection with diverse infectious agents. The acquisition of effector responses is tailored to each pathogen and is critically shaped by the interactions of macrophages with other innate cells and epithelial cells. Myeloid and lymphoid innate cells can differentially produce cytokines that 'instruct' the activation of macrophages. Effector macrophages can be derived from monocyte precursors as well as from embryonic, tissue-derived macrophages. Tissue-derived cues provided by epithelial cells are also critical for the 'instruction' of effective macrophage effector cells. Macrophages are also an important source of secreted factors that act on the surrounding cell populations of the immune system and help orchestrate a productive response for pathogen eradication and tissue repair. BETs, basophil-derived extracellular traps; TSLP, thymic stromal lymphopoietin.
Cells of the innate immune system can also provide a more rapid directed response upon re-exposure to pathogens and thereby contribute to acquired resistance. This is now best documented for NK cells and macrophages, but it raises the possibility that other cells of the innate immune system with memory-like properties will also be identified. A central tenet of innate acquired resistance is that the specificity of the memory response depends on the activation of specific PRRs, analogous to activation of T cells and B cells through antigen receptors. More studies are needed to elucidate the mechanisms of trained innate immunity. In particular, is specificity again largely dependent on epigenetic modifications that prime cells for increased responsiveness to specific PRR signaling pathways? How plastic are the changes in innate memory cells? Do they require an inflammatory tissue milieu to sustain a persistent phenotype? Investigating these questions should provide essential insights into innate memory responses and should deliver new targets for vaccine development and also, potentially, for the induction of long-term hypo-responsiveness to prevent tissue damage during inflammatory disease.
References
Wills-Karp, M. et al. Trefoil factor 2 rapidly induces interleukin 33 to promote type 2 immunity during allergic asthma and hookworm infection. J. Exp. Med. 209, 607–622 (2012).
Patel, N. et al. A2B adenosine receptor induces protective antihelminth type 2 immune responses. Cell Host Microbe 15, 339–350 (2014).
Gause, W.C., Wynn, T.A. & Allen, J.E. Type 2 immunity and wound healing: evolutionary refinement of adaptive immunity by helminths. Nat. Rev. Immunol. 13, 607–614 (2013).
Sutherland, T.E. et al. Chitinase-like proteins promote IL-17-mediated neutrophilia in a tradeoff between nematode killing and host damage. Nat. Immunol. 15, 1116–1125 (2014).
Chiu, C. & Openshaw, P.J. Antiviral B cell and T cell immunity in the lungs. Nat. Immunol. 16, 18–26 (2015).
Yan, N. & Chen, Z.J. Intrinsic antiviral immunity. Nat. Immunol. 13, 214–222 (2012).
Cervantes-Barragan, L. et al. Control of coronavirus infection through plasmacytoid dendritic-cell-derived type I interferon. Blood 109, 1131–1137 (2007).
Ciancanelli, M.J. et al. Infectious disease. Life-threatening influenza and impaired interferon amplification in human IRF7 deficiency. Science 348, 448–453 (2015).
Lang, P.A. et al. Hematopoietic cell-derived interferon controls viral replication and virus-induced disease. Blood 113, 1045–1052 (2009).
Macal, M. et al. Plasmacytoid dendritic cells are productively infected and activated through TLR-7 early after arenavirus infection. Cell Host Microbe 11, 617–630 (2012).
Sonnenberg, G.F. & Artis, D. Innate lymphoid cells in the initiation, regulation and resolution of inflammation. Nat. Med. 21, 698–708 (2015).
Murray, P.J. et al. Macrophage activation and polarization: nomenclature and experimental guidelines. Immunity 41, 14–20 (2014).
Carpenter, S., Ricci, E.P., Mercier, B.C., Moore, M.J. & Fitzgerald, K.A. Post-transcriptional regulation of gene expression in innate immunity. Nat. Rev. Immunol. 14, 361–376 (2014).
Murray, P.J., Rathmell, J. & Pearce, E. SnapShot: Immunometabolism. Cell Metab. 22, 190–190.e1 (2015).
Chen, F. et al. Neutrophils prime a long-lived effector macrophage phenotype that mediates accelerated helminth expulsion. Nat. Immunol. 15, 938–946 (2014).
Kleinnijenhuis, J. et al. Bacille Calmette-Guerin induces NOD2-dependent nonspecific protection from reinfection via epigenetic reprogramming of monocytes. Proc. Natl. Acad. Sci. USA 109, 17537–17542 (2012).
Saeed, S. et al. Epigenetic programming of monocyte-to-macrophage differentiation and trained innate immunity. Science 345, 1251086 (2014).
Randolph, G.J. A macrophage revolution-and beyond. Immunol. Rev. 262, 5–8 (2014).
Gautier, E.L. et al. Immunological Genome Consortium. Gene-expression profiles and transcriptional regulatory pathways that underlie the identity and diversity of mouse tissue macrophages. Nat. Immunol. 13, 1118–1128 (2012).
Gomez Perdiguero, E. et al. Tissue-resident macrophages originate from yolk-sac-derived erythro-myeloid progenitors. Nature 518, 547–551 (2015).
Hashimoto, D. et al. Tissue-resident macrophages self-maintain locally throughout adult life with minimal contribution from circulating monocytes. Immunity 38, 792–804 (2013).
Lavin, Y. et al. Tissue-resident macrophage enhancer landscapes are shaped by the local microenvironment. Cell 159, 1312–1326 (2014).
Hoeffel, G. et al. C-Myb(+) erythro-myeloid progenitor-derived fetal monocytes give rise to adult tissue-resident macrophages. Immunity 42, 665–678 (2015).
Epelman, S., Lavine, K.J. & Randolph, G.J. Origin and functions of tissue macrophages. Immunity 41, 21–35 (2014).
Schiwon, M. et al. Crosstalk between sentinel and helper macrophages permits neutrophil migration into infected uroepithelium. Cell 156, 456–468 (2014).
Silva, M.T. When two is better than one: macrophages and neutrophils work in concert in innate immunity as complementary and cooperative partners of a myeloid phagocyte system. J. Leukoc. Biol. 87, 93–106 (2010).
Bourdonnay, E. et al. Transcellular delivery of vesicular SOCS proteins from macrophages to epithelial cells blunts inflammatory signaling. J. Exp. Med. 212, 729–742 (2015).
Westphalen, K. et al. Sessile alveolar macrophages communicate with alveolar epithelium to modulate immunity. Nature 506, 503–506 (2014).
Ginhoux, F. & Jung, S. Monocytes and macrophages: developmental pathways and tissue homeostasis. Nat. Rev. Immunol. 14, 392–404 (2014).
Serbina, N.V. & Pamer, E.G. Monocyte emigration from bone marrow during bacterial infection requires signals mediated by chemokine receptor CCR2. Nat. Immunol. 7, 311–317 (2006).
Shi, C. et al. Bone marrow mesenchymal stem and progenitor cells induce monocyte emigration in response to circulating toll-like receptor ligands. Immunity 34, 590–601 (2011).
Serbina, N.V., Jia, T., Hohl, T.M. & Pamer, E.G. Monocyte-mediated defense against microbial pathogens. Annu. Rev. Immunol. 26, 421–452 (2008).
Espinosa, V. et al. Inflammatory monocytes orchestrate innate antifungal immunity in the lung. PLoS Pathog. 10, e1003940 (2014).
Okabe, Y. & Medzhitov, R. Tissue-specific signals control reversible program of localization and functional polarization of macrophages. Cell 157, 832–844 (2014).
Askenase, M.H. et al. Bone-marrow-resident NK cells prime monocytes for regulatory function during infection. Immunity 42, 1130–1142 (2015).
Goldszmid, R.S. et al. NK cell-derived interferon-γ orchestrates cellular dynamics and the differentiation of monocytes into dendritic cells at the site of infection. Immunity 36, 1047–1059 (2012).
Yap, G.S. & Rivera, A. IFN-γ signals a changing of the guards. Immunity 36, 904–906 (2012).
Kreider, T., Anthony, R.M., Urban, J.F. Jr. & Gause, W.C. Alternatively activated macrophages in helminth infections. Curr. Opin. Immunol. 19, 448–453 (2007).
Loke, P. et al. Alternative activation is an innate response to injury that requires CD4+ T cells to be sustained during chronic infection. J. Immunol. 179, 3926–3936 (2007).
Chen, F. et al. An essential role for TH2-type responses in limiting acute tissue damage during experimental helminth infection. Nat. Med. 18, 260–266 (2012).
Pesce, J.T. et al. Arginase-1-expressing macrophages suppress Th2 cytokine-driven inflammation and fibrosis. PLoS Pathog. 5, e1000371 (2009).
Anthony, R.M. et al. Memory T(H)2 cells induce alternatively activated macrophages to mediate protection against nematode parasites. Nat. Med. 12, 955–960 (2006).
Esser-von Bieren, J. et al. Antibodies trap tissue migrating helminth larvae and prevent tissue damage by driving IL-4Rα-independent alternative differentiation of macrophages. PLoS Pathog. 9, e1003771 (2013).
Egawa, M. et al. Inflammatory monocytes recruited to allergic skin acquire an anti-inflammatory M2 phenotype via basophil-derived interleukin-4. Immunity 38, 570–580 (2013).
Netea, M.G. Immunological memory in innate immunity. J. Innate Immun. 6, 117–118 (2014).
Netea, M.G., Latz, E., Mills, K.H. & O'Neill, L.A. Innate immune memory: a paradigm shift in understanding host defense. Nat. Immunol. 16, 675–679 (2015).
Yoshida, K. et al. The transcription factor ATF7 mediates lipopolysaccharide-induced epigenetic changes in macrophages involved in innate immunological memory. Nat. Immunol. 16, 1034–1043 (2015).
Didierlaurent, A. et al. Sustained desensitization to bacterial Toll-like receptor ligands after resolution of respiratory influenza infection. J. Exp. Med. 205, 323–329 (2008).
Lee, J. et al. Epigenetic modification and antibody-dependent expansion of memory-like NK cells in human cytomegalovirus-infected individuals. Immunity 42, 431–442 (2015).
Jensen, K.J. et al. Heterologous immunological effects of early BCG vaccination in low-birth-weight infants in Guinea-Bissau: a randomized-controlled trial. J. Infect. Dis. 211, 956–967 (2015).
Mantovani, A., Cassatella, M.A., Costantini, C. & Jaillon, S. Neutrophils in the activation and regulation of innate and adaptive immunity. Nat. Rev. Immunol. 11, 519–531 (2011).
Lim, K. et al. Neutrophil trails guide influenza-specific CD8+ T cells in the airways. Science 349, aaa4352 (2015).
Warnatsch, A., Ioannou, M., Wang, Q. & Papayannopoulos, V. Inflammation. Neutrophil extracellular traps license macrophages for cytokine production in atherosclerosis. Science 349, 316–320 (2015).
Taylor, P.R. et al. Activation of neutrophils by autocrine IL-17A-IL-17RC interactions during fungal infection is regulated by IL-6, IL-23, RORγt and dectin-2. Nat. Immunol. 15, 143–151 (2014).
Sturge, C.R. et al. TLR-independent neutrophil-derived IFN-γ is important for host resistance to intracellular pathogens. Proc. Natl. Acad. Sci. USA 110, 10711–10716 (2013).
Novais, F.O. et al. Neutrophils and macrophages cooperate in host resistance against Leishmania braziliensis infection. J. Immunol. 183, 8088–8098 (2009).
Campbell, E.L. et al. Transmigrating neutrophils shape the mucosal microenvironment through localized oxygen depletion to influence resolution of inflammation. Immunity 40, 66–77 (2014).
Zhang, X., Majlessi, L., Deriaud, E., Leclerc, C. & Lo-Man, R. Coactivation of Syk kinase and MyD88 adaptor protein pathways by bacteria promotes regulatory properties of neutrophils. Immunity 31, 761–771 (2009).
Mócsai, A. Diverse novel functions of neutrophils in immunity, inflammation, and beyond. J. Exp. Med. 210, 1283–1299 (2013).
Giacomin, P.R. et al. Thymic stromal lymphopoietin-dependent basophils promote Th2 cytokine responses following intestinal helminth infection. J. Immunol. 189, 4371–4378 (2012).
Lantz, C.S. et al. Role for interleukin-3 in mast-cell and basophil development and in immunity to parasites. Nature 392, 90–93 (1998).
Lantz, C.S. et al. IL-3 is required for increases in blood basophils in nematode infection in mice and can enhance IgE-dependent IL-4 production by basophils in vitro. Lab. Invest. 88, 1134–1142 (2008).
Siracusa, M.C. et al. TSLP promotes interleukin-3-independent basophil haematopoiesis and type 2 inflammation. Nature 477, 229–233 (2011).
Ogilvie, B.M., Hesketh, P.M. & Rose, M.E. Nippostrongylus brasiliensis: peripheral blood leucocyte response of rats, with special reference to basophils. Exp. Parasitol. 46, 20–30 (1978).
Min, B. et al. Basophils produce IL-4 and accumulate in tissues after infection with a Th2-inducing parasite. J. Exp. Med. 200, 507–517 (2004).
Voehringer, D., Shinkai, K. & Locksley, R.M. Type 2 immunity reflects orchestrated recruitment of cells committed to IL-4 production. Immunity 20, 267–277 (2004).
Voehringer, D. Protective and pathological roles of mast cells and basophils. Nat. Rev. Immunol. 13, 362–375 (2013).
Siracusa, M.C., Comeau, M.R. & Artis, D. New insights into basophil biology: initiators, regulators, and effectors of type 2 inflammation. Ann. NY Acad. Sci. 1217, 166–177 (2011).
Sullivan, B.M. et al. Genetic analysis of basophil function in vivo. Nat. Immunol. 12, 527–535 (2011).
van Panhuys, N. et al. Basophils are the major producers of IL-4 during primary helminth infection. J. Immunol. 186, 2719–2728 (2011).
Ohnmacht, C. & Voehringer, D. Basophils protect against reinfection with hookworms independently of mast cells and memory Th2 cells. J. Immunol. 184, 344–350 (2010).
Ohnmacht, C. & Voehringer, D. Basophil effector function and homeostasis during helminth infection. Blood 113, 2816–2825 (2009).
Ohnmacht, C. et al. Basophils orchestrate chronic allergic dermatitis and protective immunity against helminths. Immunity 33, 364–374 (2010).
Herbst, T. et al. Antibodies and IL-3 support helminth-induced basophil expansion. Proc. Natl. Acad. Sci. USA 109, 14954–14959 (2012).
Obata-Ninomiya, K. et al. The skin is an important bulwark of acquired immunity against intestinal helminths. J. Exp. Med. 210, 2583–2595 (2013).
Kang, Y.H. & Biswas, S.K. Basophil-macrophage dialog in allergic inflammation. Immunity 38, 408–410 (2013).
Leung, D.Y. et al. Presence of IgE antibodies to staphylococcal exotoxins on the skin of patients with atopic dermatitis. Evidence for a new group of allergens. J. Clin. Invest. 92, 1374–1380 (1993).
Yousefi, S. et al. Basophils exhibit antibacterial activity through extracellular trap formation. Allergy 70, 1184–1188 (2015).
Gessner, A., Mohrs, K. & Mohrs, M. Mast cells, basophils, and eosinophils acquire constitutive IL-4 and IL-13 transcripts during lineage differentiation that are sufficient for rapid cytokine production. J. Immunol. 174, 1063–1072 (2005).
Qiu, Y. et al. Eosinophils and type 2 cytokine signaling in macrophages orchestrate development of functional beige fat. Cell 157, 1292–1308 (2014).
Wu, D. et al. Eosinophils sustain adipose alternatively activated macrophages associated with glucose homeostasis. Science 332, 243–247 (2011).
Urban, J.F. Jr. et al. Stat6 signaling promotes protective immunity against Trichinella spiralis through a mast cell- and T cell-dependent mechanism. J. Immunol. 164, 2046–2052 (2000).
Hepworth, M.R. et al. Mast cells orchestrate type 2 immunity to helminths through regulation of tissue-derived cytokines. Proc. Natl. Acad. Sci. USA 109, 6644–6649 (2012).
Sandig, H. & Bulfone-Paus, S. TLR signaling in mast cells: common and unique features. Front. Immunol. 3, 185 (2012).
Hogan, S.P., Waddell, A. & Fulkerson, P.C. Eosinophils in infection and intestinal immunity. Curr. Opin. Gastroenterol. 29, 7–14 (2013).
Svensson, L. & Wennerås, C. Human eosinophils selectively recognize and become activated by bacteria belonging to different taxonomic groups. Microbes Infect. 7, 720–728 (2005).
Ketavarapu, J.M. et al. Mast cells inhibit intramacrophage Francisella tularensis replication via contact and secreted products including IL-4. Proc. Natl. Acad. Sci. USA 105, 9313–9318 (2008).
Moro, K. et al. Innate production of TH2 cytokines by adipose tissue-associated c-Kit+Sca-1+ lymphoid cells. Nature 463, 540–544 (2010).
Price, A.E. et al. Systemically dispersed innate IL-13-expressing cells in type 2 immunity. Proc. Natl. Acad. Sci. USA 107, 11489–11494 (2010).
Neill, D.R. et al. Nuocytes represent a new innate effector leukocyte that mediates type-2 immunity. Nature 464, 1367–1370 (2010).
Eberl, G., Colonna, M., Di Santo, J.P. & McKenzie, A.N. Innate lymphoid cells. Innate lymphoid cells: a new paradigm in immunology. Science 348, aaa6566 (2015).
Bouchery, T. et al. ILC2s and T cells cooperate to ensure maintenance of M2 macrophages for lung immunity against hookworms. Nat. Commun. 6, 6970 (2015).
Besnard, A.G. et al. IL-33-mediated protection against experimental cerebral malaria is linked to induction of type 2 innate lymphoid cells, M2 macrophages and regulatory T cells. PLoS Pathog. 11, e1004607 (2015).
Arase, H., Mocarski, E.S., Campbell, A.E., Hill, A.B. & Lanier, L.L. Direct recognition of cytomegalovirus by activating and inhibitory NK cell receptors. Science 296, 1323–1326 (2002).
Newman, K.C. & Riley, E.M. Whatever turns you on: accessory-cell-dependent activation of NK cells by pathogens. Nat. Rev. Immunol. 7, 279–291 (2007).
Riise, R.E. et al. TLR-stimulated neutrophils instruct NK cells to trigger dendritic cell maturation and promote adaptive T cell responses. J. Immunol. 195, 1121–1128 (2015).
Jaeger, B.N. et al. Neutrophil depletion impairs natural killer cell maturation, function, and homeostasis. J. Exp. Med. 209, 565–580 (2012).
Bär, E., Whitney, P.G., Moor, K., Reis e Sousa, C. & LeibundGut-Landmann, S. IL-17 regulates systemic fungal immunity by controlling the functional competence of NK cells. Immunity 40, 117–127 (2014).
Jenkins, M.R. et al. Failed CTL/NK cell killing and cytokine hypersecretion are directly linked through prolonged synapse time. J. Exp. Med. 212, 307–317 (2015).
Perona-Wright, G. et al. Systemic but not local infections elicit immunosuppressive IL-10 production by natural killer cells. Cell Host Microbe 6, 503–512 (2009).
Robinette, M.L. et al. Immunological Genome Consortium. Transcriptional programs define molecular characteristics of innate lymphoid cell classes and subsets. Nat. Immunol. 16, 306–317 (2015).
Seo, S.U. et al. Intestinal macrophages arising from CCR2+ monocytes control pathogen infection by activating innate lymphoid cells. Nat. Commun. 6, 8010 (2015).
Chen, L. et al. IL-23 activates innate lymphoid cells to promote neonatal intestinal pathology. Mucosal Immunol. 8, 390–402 (2015).
Mortha, A. et al. Microbiota-dependent crosstalk between macrophages and ILC3 promotes intestinal homeostasis. Science 343, 1249288 (2014).
Gasteiger, G. & Rudensky, A.Y. Interactions between innate and adaptive lymphocytes. Nat. Rev. Immunol. 14, 631–639 (2014).
Guarda, G. et al. T cells dampen innate immune responses through inhibition of NLRP1 and NLRP3 inflammasomes. Nature 460, 269–273 (2009).
Acknowledgements
Supported by the US National Institutes of Health (R01AI114647-01A1 and R21CA167238-01A1 to A.R.; K22 AI110573-01 and 1R01AI123224 to M.C.S.; R01AI083405 to G.S.Y.; and 1R01AI107588 to W.C.G.) and the Amelior Foundation (Gause laboratory).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Rivera, A., Siracusa, M., Yap, G. et al. Innate cell communication kick-starts pathogen-specific immunity. Nat Immunol 17, 356–363 (2016). https://doi.org/10.1038/ni.3375
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ni.3375
This article is cited by
-
Peroxiredoxin 3 has a crucial role in the macrophage polarization by regulating mitochondrial homeostasis
Respiratory Research (2024)
-
Age-related immune alterations and cerebrovascular inflammation
Molecular Psychiatry (2022)
-
Nuclear ADP-ribosylation drives IFNγ-dependent STAT1α enhancer formation in macrophages
Nature Communications (2021)
-
A Catalogus Immune Muris of the mouse immune responses to diverse pathogens
Cell Death & Disease (2021)
-
Pretreatment of Indobufen and Aspirin and their Combinations with Clopidogrel or Ticagrelor Alleviates Inflammasome Mediated Pyroptosis Via Inhibiting NF-κB/NLRP3 Pathway in Ischemic Stroke
Journal of Neuroimmune Pharmacology (2021)