Abstract
Attentional deficits are a core symptom of schizophrenia. Post-mortem analyses of the brains of schizophrenics reveal consistent abnormalities in γ-aminobutyric acid (GABA) interneurons indicative of reduced cortical GABA transmission, raising the possibility that this pathology contributes to attentional deficits. We examined whether blockade of prefrontal cortex (PFC) GABAA receptors with bicuculline (BMI) impairs attention in rats using the 5-choice serial reaction time task (5CSRTT). For comparison, we also examined whether administration of the GABAA receptor agonist muscimol (MUS) would improve attention. In parallel, we examined the effects of both manipulations on activity in an open field and on motivation using the intracranial self-stimulation (ICSS) test. BMI increased PFC neuronal activity, as reflected by increased Fos immunolabeling, and impaired attention, as reflected by decreased accuracy and increased omissions. Although increased omissions also may reflect reductions in locomotor activity or motivation, the overall pattern of effects does not support either of these interpretations: BMI did not affect locomotor activity, and it enhanced motivation in the ICSS test. MUS did not affect attention, although it increased impulsive behavior at a dose that suppressed PFC neuronal activity, as reflected by decreased Fos immunolabeling. These impulsivity effects are not due to altered locomotor activity (which was decreased) or motivation (which was not affected). Our data support the hypothesis that cortical GABA neurons have an important role in regulating attention and may have direct implications for the treatment of schizophrenia.
Similar content being viewed by others
INTRODUCTION
Cognitive deficits, including attentional deficits, are a core feature of schizophrenia (http://www.nimh.nih.gov/publicat/schizoph.cfm) and are refractory to currently available antipsychotic treatments. In schizophrenia, cognitive impairments predate the illness onset, are stable across phases of illness, and are present in non-schizophrenic first-degree relatives of people with schizophrenia (Cornblatt and Malhotra, 2001; Chen and Faraone, 2000). Furthermore, cognitive deficits predict patient difficulties in maintaining employment, living independently and having meaningful social interactions (Green et al, 2004). Understanding the biological bases of these deficits may lead to the development of more efficacious treatments for this devastating disorder.
Pathology in γ-aminobutyric acid (GABA) neurons is one of the most reliable abnormalities found in post-mortem analyses of the schizophrenic brain (Lewis et al, 2005; Benes, 2010). For example, reduced gene expression of the 67-kDa isoform of the GABA synthesizing enzyme glutamic acid decarboxylase (GAD67) and a corresponding reduction in gene expression of the GABA uptake transporter (GAT1) are observed in the prefrontal cortex (PFC) (Volk et al, 2000, 2001; for review, see Lewis et al (2005)). These findings suggest reductions in the synthesis, release, and reuptake of GABA in the brains of schizophrenics.
Within the PFC, GABA neurons regulate the activity of efferent glutamatergic pyramidal neurons (Markram et al, 2004; White, 1989). This microcircuitry is essential for establishing neural synchrony (ie, gamma oscilliations) within cortical networks, including that evoked during attentional tasks (Bartos et al, 2007; Gruber et al, 1999; Steinmetz et al, 2000). Notably, people with schizophrenia exhibit reduced evoked gamma oscillations during cognitive tasks (Cho et al, 2006; Gonzalez-Burgos and Lewis, 2008). Collectively, these findings raise the possibility that reduced GABA-mediated inhibition leads to reductions in neural synchrony and the cognitive deficits that are characteristic of schizophrenia.
Research in laboratory animals provides support for the putative role of GABA neurons in the regulation of cognitive function. For example, blockade of cortical GABAA receptors impairs working memory in monkeys (Sawaguchi et al, 1989) and attentional set-shifting in rats (Enomoto et al, 2011). The purpose of the current experiment was to extend this research by determining if blockade of cortical GABAA receptors with bicuculline (BMI) impairs visuospatial attention in the 5-choice serial reaction time task (5CSRTT) in rats. The 5CSRTT is analogous to the continuous performance task (CPT), which is used to quantify sustained attention in humans (Robbins, 2002). Importantly, individuals with schizophrenia exhibit attentional deficits on the CPT (Cornblatt and Malhotra, 2001; Chen and Faraone, 2000), providing a strong rationale for using the 5CSRTT to study the neurobiology of this disorder. For comparison, we investigated whether low-dose administration of the GABAA receptor agonist muscimol (MUS) could enhance attentional performance. Because high doses of MUS can inhibit PFC cortical activity, we speculated that high doses of MUS would impair 5CSRTT performance in a manner similar to that observed following PFC lesions (Chudasama et al, 2003; Passetti et al, 2002; Pezze et al, 2009; Muir et al, 1996). We used additional tests (open field, intracranial self-stimulation (ICSS)) to determine if these treatments can cause changes in locomotor activity or motivation, both of which can affect performance in the 5CSRTT.
MATERIALS AND METHODS
Rats
Twenty-nine adult male Sprague-Dawley rats (Charles River Laboratories, Raleigh, NC) were used. Procedures began on approximately post-natal day 60. The rats used in the 5CSRTT and open field tests were housed in pairs whereas those used in the ICSS test were housed singly. All rats were maintained on a 12-h/12-h light–dark cycle (lights on at 0700 h). Rats were given 1 week to acclimate to the housing conditions with free access to food (Purina Rat Chow) and water. Rats tested in the 5CSRTT were food restricted to 85% of their free-feeding weights starting 24-h before the onset of training. All rats had free access to water while in the home cage. Experiments were conducted in accordance with the Guide for the Care and Use of Laboratory Animals (National Academy Press, 1996) and McLean Hospital policies.
Drugs
(−)-Bicuculline methiodide (BMI) and muscimol (MUS) were purchased from Sigma-Aldrich (St Louis, MO). Drugs were dissolved in physiological saline (0.9%). The dose of BMI was based upon its salt form.
Surgery
Rats were anesthetized with sodium pentobarbital (65 mg/kg, IP) and treated with atropine sulfate (0.25 mg/kg, SC) to minimize bronchial secretions. Rats were implanted with bilateral guide cannulae (26 G; Plastics One, Roanoke, VA) that were situated at the border of infralimbic (IL) and prelimbic cortex (PrL) cortices (relative to bregma: AP=+3.2, ML=±0.75, DV=−1.8 mm from dura; Paxinos and Watson, 1997). Obturators and injector needles (33 G) extended 1.5 mm below the guide cannulae, into the IL/PrL. Rats in the ICSS experiment were simultaneously implanted with a unilateral monopolar, stainless-steel electrode (0.25-mm diameter; Plastics One, Roanoke, VA) aimed at the right medial forebrain bundle at the level of the lateral hypothalamus (relative to bregma: AP=−2.8, ML=1.6, DV=−7.8 from dura). The electrodes were coated with polyamide insulation except at the flattened tip. Skull screws (one of which served as the ground) and the electrode were secured to the skull with dental acrylic.
The 5-Choice Serial Reaction Time Task
We trained the rats as described previously (Paine et al, 2009). Sessions started with the delivery of 1 food pellet (45 mg, Bio-Serv, Frenchtown, NJ); the first trial commenced upon retrieval. A nose poke into the magazine initiated a 5-s intertrial interval (ITI) and illumination of the house light. At the end of the ITI, a 1.0-s light stimulus was presented at the rear of one of the five stimulus locations (apertures). Rats had up to 5 s (limited hold) to make a response. A response in the illuminated aperture (correct response) triggered delivery of 1 food pellet and illumination of the magazine light, which remained illuminated for 5 s following pellet delivery. Nose pokes in the remaining apertures were considered incorrect responses and triggered a 5-s time-out (TO) during which the house light was extinguished. Similarly, failure to respond during the limited hold (ie, an omission) triggered a 5-s TO. The subsequent trial was initiated at the end of the TO period. Responses occurring during the ITI were considered premature responses and also triggered a 5-s TO; the same trial was re-started at the end of the TO period. Responses occurring during the TO period had no programmed consequences. Sessions ended after 90 trials or 30 min. Performance measures of interest were % accuracy ((correct responses/(correct+incorrect responses)) × 100), % omissions ((omissions/trials completed) × 100), premature responses, magazine entries, correct response latency (the time from the stimulus onset to a correct response), and reward latency (the time from a correct response to the collection of the food). Subjects were considered to have acquired the task when their accuracy was ⩾60% (chance performance in this test is 20%) and omissions were ⩽20% for 5 consecutive days. Upon reaching criterion performance, the rats underwent surgery to implant guide cannulae.
Rats (n=17) were allowed to recover for 7 days and then were re-stabilized for 5 days before drug testing. To habituate rats to the infusion procedure they were first infused with vehicle (VEH, 0.9% physiological saline); data from this session were discarded. On test days, rats were infused with either BMI (0, 6.25, 12.5, or 25.0 ng/0.5 μl/side) or MUS (0, 6.25, 12.5, 25.0, or 50.0 ng/0.5 μl/side) immediately before testing on the 5CSRTT. Drug doses for half of the rats tested with each drug were administered in an ascending order, while the remainder of the rats received drug doses in a descending order. There was a minimum of 2 drug-free days between infusions.
Locomotor Activity in an Open Field
Following completion of dose–response relationships in the 5CSRTT, locomotor activity was quantified in an open field. Locomotor activity was recorded in automated (43.2 × 43.2 cm) activity chambers (MED Associates, St Albans, VT). Each locomotor activity session consisted of a 30-min habituation period, after which the rat was removed from the chamber and administered a drug infusion. Immediately following the infusion, the rat was returned to the activity chamber for a 30-min test period. Activity was assessed twice for each rat, once when VEH was infused and once when either BMI (25.0 ng/0.5 μl/side) or MUS (50.0 ng/0.5 μl/side) was infused. The rats were tested according to their previous history (eg, rats that had received BMI in the 5CSRTT experiment were administered BMI during locomotor activity testing). The order of vehicle vs drug administration was counterbalanced across rats. Activity sessions were separated by at least 3–4 drug-free days.
Intracranial Self-Stimulation
Rats (n=12) used for the ICSS studies had not been used in the other tests. The rats were trained on a continuous reinforcement schedule (FR1) to respond for brain stimulation (Carlezon and Chartoff, 2007; Paine et al, 2009). Lever pressing resulted in the illumination of a 2-W house light and immediate delivery of a 0.5-s train of square-wave cathodal pulses (0.1 ms pulse duration) at a set frequency of 141 Hz. Responses during the 0.5-s stimulation period did not earn additional stimulation. The stimulation current (200–350 μA) was adjusted gradually to the lowest value that would sustain a reliable rate of responding (at least 40 rewards per minute).
Once rats reliably lever pressed for stimulation, they were adapted to lever press for a descending series of stimulation frequencies. Each series consisted of 15 1-min trials at each frequency. Each trial consisted of a 5-s ‘priming’ phase during which non-contingent stimulation was given, followed by a 50-s test phase during which the number of responses was counted and ended with a 5-s TO period during which no stimulation was available. The stimulation frequency was then lowered by ∼10% (0.05 log10 units) and another trial was started. After responding had been evaluated at each of the 15 frequencies, the procedure was repeated such that each rat was given four series per day (60 min of training). To characterize the functions relating response strength to reward magnitude, a least-squares line of best fit was plotted across the frequencies that sustained responding at 20, 30, 40, 50, and 60% of the maximum rate using customized analysis software. The threshold for responding was defined as the frequency at which the line intersected the x-axis (theta-0). Drug testing started when mean thresholds varied by less than ±15% over three consecutive training sessions.
Drug effects were quantified using the ‘curve-shift’ method of analysis (Carlezon and Chartoff, 2007; Paine et al, 2009). This method can distinguish changes in motivation (as reflected by alterations in theta-0) from changes in response capabilities (as reflected by alterations in maximum response rates) (see Carlezon and Chartoff (2007)). For each rat, three rate-frequency functions (‘curves’) were determined immediately before drug infusions. The second and third curves were averaged to obtain the baseline (threshold and maximal response rate) parameters. Each rat was then infused with either BMI (0–25.0 ng/0.5 μl/side) or MUS (0–50.0 ng/0.5 μl/side) and tested for an additional 15-min rate-frequency curve. Rats were tested with both BMI and MUS; rats were given at least 7–10 drug-free days before testing on the alternate drug. Doses of each drug were administered in either an ascending or descending manner (counterbalanced across rats); tests with each drug dose were separated by at least 2 drug-free days.
Histology
Following the last test session, rats were anesthetized with sodium pentobarbital (130 mg/kg, IP) and transcardially perfused with 0.9% NaCl followed by 4% paraformaldehyde. A subset of animals was perfused 90 min following infusions of BMI, MUS, or VEH; the brains from these animals were used for Fos immunohistochemistry (see below). Following perfusions, brains were removed, post-fixed for 24 h and then cryoprotected in 30% sucrose before slicing on a microtome. Sections (40 μm) were mounted on slides, stained with cresyl violet, and placements assessed.
Fos Immunohistochemistry
Free-floating sections (40 μm) from animals perfused 90 min following infusions were used to confirm changes in neuronal activity following manipulations of GABAA receptor activation. Briefly, endogenous peroxidase activity was quenched by incubation in 0.3% H2O2 and then non-specific binding was blocked by a 2-h incubation in AB media (0.3% Triton X-100, 2% normal goat serum (Invitrogen, Carlsbad, CA) and 1% bovine serum albumin (Sigma) in 0.01 M Tris-buffered saline). Sections were then incubated overnight with a polyclonal rabbit anti-c-Fos antibody (PC38T, Calbiochem, La Jolla, CA; 1 : 10 000 diluted in AB media). The following day sections were washed, incubated for 1 h at room temperature in biotinylated goat anti-rabbit immunoglobulin G secondary antibody (Vector Laboratories, Burlingame, CA; 1 : 200 diluted in AB media) and then incubated with avidin–biotin–peroxidase complex (Vectastain ABC Elite kit; Vector Laboratories) for 30 min at room temperature. Finally, sections were visualized using 0.05% 3,3′-diaminobenzidine tetrahydrochloride containing 0.01% H2O2 (Vector Laboratories) for 10 min. Rinsing in Tris-buffered saline terminated the reaction.
Statistical Analyses
5CSRTT data and ICSS data were analyzed using separate one-way repeated measures ANOVAs with Dose as the within-subjects factor. Locomotor activity data from habituation and test periods were analyzed separately using two-way repeated measures ANOVAs with Condition (VEH, drug (BMI or MUS)) and Time (10, 20, 30 min) as within-subjects factors. Significant effects were further analyzed using Bonferroni Multiple Comparison post hoc tests.
RESULTS
Histology
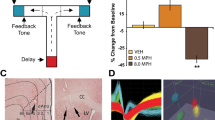
Of the 29 rats tested, four rats were excluded (n=1 for the BMI 5CSRTT/locomotor activity; n=1 for the MUS 5CSRTT/locomotor activity; and n=2 for the ICSS experiment) from statistical analyses because their cannulae placements were outside the IL/PrL (Figures 1, 2a and b).
Schematic drawing showing the location of injector tips in the medial PFC of rats infused with bicuculline (left, n=7) or muscimol (right, n=8) and tested in the 5-choice serial reaction time task. Rats were excluded (not shown) if their tips were not within the boundary of either the prelimbic (PrL) or infralimbic (IL) cortex. Numbers on the left indicate location forward from bregma. Adapted from Paxinos and Watson (1997).
Fos immunohistochemistry was used to confirm that the BMI and MUS infusions had the expected effects on PFC neuronal activity. Microinfusion of BMI (25 ng/0.5 μl/side) increased Fos immunolabeling (Figure 2d), whereas MUS (50 ng/0.5 μl/side) decreased Fos immunolabeling (Figure 2f) relative to that observed when VEH was infused (Figure 2e). These data confirm that BMI and MUS infusions altered neuronal activity at doses that were effective in the behavioral experiments.
Effects of manipulating cortical GABAA receptor activation on c-Fos expression. (a) Schematic of the PFC approximating location of cannulae placements (Paxinos and Watson, 1997). Box indicates field of view in panel (b). (b) Representative cannula placements indicating guide cannulae and obturator; injectors were the same length as the obturator. (c) Schematic of the PFC approximating the field of view in panels (d–f) (Paxinos and Watson, 1997). Intra-PFC infusions of the GABAA receptor antagonist bicuculline (BMI; 25.0 ng/0.5 μl/side) increased c-Fos expression (d), while intra-PFC infusions of the GABAA receptor agonist muscimol (MUS; 50.0 ng/0.5 μl/side) decreased c-Fos expression (f) relative to vehicle (VEH) infusions (e). All infusions were administered 90 min before the rats were killed. PrL, prelimbic cortex; IL, infralimbic cortex.
5-Choice Serial Reaction Time Task
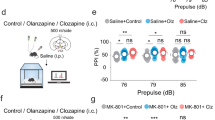
Intra-PFC administration of BMI (n=7) affected accuracy (F[3, 18]=3.20, P<0.05; Figure 3), omissions (F[3, 18]=30.67, P<0.01), and reward retrieval latency (F[3, 18]=4.41, P<0.05). BMI (25.0 ng) decreased accuracy and increased the reward retrieval latency compared with VEH (all Ps<0.05). BMI (12.5–25.0 ng) increased omissions compared with VEH (all Ps<0.05–0.01). All other measures were unaffected by BMI administration (all Fs[3, 18] <2.48, n.s.; Figure 3, Table 1).
Effects of intra-PFC infusions of the GABAA receptor antagonist bicuculline on performance in the 5-choice serial reaction time task. Intra-PFC infusions of bicuculline (n=7) decreased accuracy (P<0.05) (a) and increased both omissions (P<0.01) (b) and the reward retrieval latency (P<0.05) (d). Bicuculline infusions did not affect premature responses (c). **P<0.01, *P<0.05 from 0.0 (Bonferroni Multiple Comparison test).
Intra-PFC administration of MUS (n=8) affected premature responses (F[4, 28]=5.89, P<0.05; Figure 4); MUS (50.0 ng) increased premature responses compared with VEH (P<0.05). All other measures were unaffected by MUS administration (all Fs[4, 28] <1.07, n.s.; Figure 4, Table 1).
Effects of intra-PFC infusions of the GABAA receptor agonist muscimol on performance in the 5-choice serial reaction time task. Intra-PFC infusions of muscimol (n=8) increased premature responses (P<0.05) (c), but did not affect accuracy (a), omissions (b), or the reward retrieval latency (d). *P<0.05 from 0.0 (Bonferroni Multiple Comparison test).
Locomotor Activity
Across the habituation period before BMI and VEH infusions, locomotor activity significantly decreased (F[2, 12]=67.40, P<0.01; Figure 5a); activity was higher during the first 10 min compared with the remainder of the habituation period (both Ps<0.01). However, activity did not differ between the habituation period before VEH infusions as compared with that before BMI infusions (F[1, 6] <1.0, n.s.), nor was there a significant Condition × Time interaction (F[2, 12] <1.0, n.s.). Activity significantly decreased across the test period (F[2, 12]=9.67, P<0.01); activity was higher during the first 10 min compared with the remainder of the test period (both Ps<0.01). Activity was not different when VEH was infused as compared with when BMI was infused (F[1, 6] <1.0, n.s.), nor was there a significant Condition × Time interaction (F[2, 12] <1.0, n.s.).
Effects of modulating cortical GABAA receptor activation on locomotor activity. Rats were habituated to the chambers for 30 min, infused with bicuculline (BMI; 25.0 ng/0.5 μl/side; n=7), muscimol (MUS; 50.0 ng/0.5 μl/side; n=8) or their respective vehicles (VEH) and tested for an additional 30 min. Inset shows total activity during the habituation and test sessions. BMI did not affect locomotor activity (a). During the test, MUS decreased the total locomotor activity (P<0.01) (b), but there was not a significant Time × Condition interaction. **P<0.01 from VEH (main effect of Condition).
Across the habituation period before MUS and VEH infusions, locomotor activity significantly decreased (F[2, 14]=123.34, P<0.01; Figure 5b); activity was higher during the first 10 min compared with the remainder of the habituation period (both Ps<0.01). Activity did not differ between the habituation period before VEH infusions as compared with that before MUS infusions (F[1, 7] <1.0, n.s.), nor was there a Condition × Time interaction (F[2, 14] <1.0, n.s.). Activity decreased across the test period (F[2, 14]=29.87, P<0.01); activity was higher during the first 10 min compared with the remainder of the test period (both Ps<0.01). During the test period, activity was significantly higher when VEH infused as compared with when MUS was infused (F[1, 7]=14.75, P<0.01; Figure 5b, inset), but there was not a significant Condition × Time interaction (F[2, 14]=3.19, n.s.).
Intracranial Self-Stimulation
A total of 10 rats were included in this portion of the experiment. Intra-PFC infusions of BMI affected the threshold amount of stimulation required to maintain lever pressing (ie, Theta-0) (F[3, 27]=6.60, P<0.01; Figure 6a–c), without affecting maximum rates of responding (F[3, 27]=1.58, n.s.). Intra-PFC infusions of 25 ng BMI significantly decreased the amount of stimulation required to maintain lever pressing compared with VEH infusions (BMI 0 ng; P<0.01). In contrast, intra-PFC infusions of MUS did not affect either ICSS thresholds or maximum rates of responding (Fs[4, 36] <1.3, n.s.; Figure 6d–f).
Effects of modulating cortical GABAA receptor activation on intracranial self-stimulation thresholds. Representative rate-frequency curves from rats (n=10) that received intra-PFC infusions of either (a) bicuculline (BMI; 25.0 ng/0.5 μl/side) or (d) muscimol (MUS; 50.0 ng/0.5 μl/side) in comparison with when they were treated with vehicle (VEH). BMI (25.0 ng/0.5 μl/side) decreased the threshold for responding (P<0.01) (b) without affecting maximum rates of responding (c). MUS did not affect either the threshold of responding (e) or the maximum rate of responding (f). **P<0.01 from 0.0 (Bonferroni Multiple Comparison test).
DISCUSSION
Cortical GABAergic interneurons provide recurrent inhibition to pyramidal neurons, an effect that is postulated to stabilize cortical networks allowing for optimal cognitive performance (Winterer and Weinberger, 2004). It has been proposed that disruptions in GABA transmission underlie cognitive deficits in schizophrenia (Lewis et al, 2005). Here, we show that blockade of cortical GABAA receptors with BMI caused a non-selective increase in cortical activity (as indicated by increased Fos immunolabeling) and impaired attention as measured by reduced accuracy of responding and increased omissions.
Reductions in accuracy are the most reliable indicator of attentional deficits in the 5CSRTT (Robbins, 2002). Although the accuracy impairment observed following intra-PFC BMI infusions was relatively small (∼10%), it is of a similar magnitude as that observed in some PFC lesion experiments (Passetti et al, 2002, 2003b) and following other manipulations (Passetti et al, 2003a; Paine et al, 2007, 2009; Paine and Carlezon, 2009). Moreover, the accuracy impairment was observed in combination with increased omissions, another potential indicator of attentional deficits. Increased omissions in the 5CSRTT can be attributed to various factors including (i) attentional deficits (rats fail to detect the stimulus presentation), (ii) motivational deficits (rats are unwilling to ‘work’ for the food pellet), or (iii) motor deficits (rats are unable to respond) (Robbins, 2002). The pattern of results in the current experiment suggests that the increased omissions following intra-PFC BMI infusions reflect attentional deficits. Although BMI infusions increased the latency to retrieve the sugar pellet reward, the effect was small (∼300 ms) and rats exhibited normal food-seeking behavior (ie, magazine entries). Moreover, BMI decreased brain reward thresholds in the ICSS test, an effect that reflects enhanced motivation (Carlezon and Chartoff, 2007). Thus, it is unlikely that the increase in omissions results from decreased motivation to respond for a food reward. Increased omissions may also indicate reductions in activity or motor capabilities. Intra-PFC BMI infusions did not, however, affect the latency to make a correct response, impulsive behavior (ie, premature responding) or food-seeking behavior in the 5CSRTT. Moreover, rats did not exhibit reductions in locomotor activity in the open field or in the capability to respond in the ICSS test. These data suggest that intra-PFC BMI infusions did not cause gross motor deficits that interfered with the ability to nose poke in the presence of the stimulus. Combined with the small but significant deficit in accuracy, the increase in omissions observed following intra-PFC BMI infusions most likely reflects an attentional deficit.
Contrary to our hypothesis, stimulation of GABAA receptors with microinjections of MUS did not affect attention at any dose tested. At the highest dose tested—which reduced PFC activity as indicated by decreased Fos immunolabeling—PFC MUS infusions increased impulsive behavior as indicated by an increase in premature responding. Increased impulsive-like behavior cannot be easily explained by either increased locomotor activity (locomotor activity was decreased following MUS infusions) or increased reward sensitivity (which was unaffected by MUS infusions). Failure to find attentional improvements following low-dose MUS infusions may not be surprising given that MUS is a full agonist at GABAA receptors, this likely results in non-selective suppression of cortical activity, rather than the selective suppression which is likely necessary in order to synchronize specific cortical networks. Future research investigating the role of positive allosteric modulators at GABAA receptors, which may be better suited to selectively potentiate GABAA receptor activation, is warranted. Moreover, the cognitive enhancing effects of positive allosteric modulators at GABAA receptors may be more robust in models exhibiting cognitive impairments. Indeed, GABAA-positive allosteric modulators enhance novel object recognition in rats that exhibited performance deficits following chronic phencyclidine treatment, a rodent model of schizophrenia (Damgaard et al, 2011).
One limitation of our within-subject design is that the rats received several infusions of the GABA drugs. To mitigate any effects of repeated treatment on sensitivity to these drugs, we varied the order of treatment across subjects and ensured that there were drug-free days between tests. The locomotor activity and ICSS experiments were intended to identify major effects on motor capabilities or motivation that could complicate interpretation of the attention tests. It remains possible that more subtle changes in GABA receptor sensitivity could influence our results. Our data provide a rationale for more detailed studies that are designed specifically to evaluate if intra-PFC treatment with BMI or MUS cause long-term changes in sensitivity to the behavioral effects of these drugs, and identify dose ranges of these drugs that are relevant for local microinfusions. Studies designed to evaluate experience-dependent alterations in drug sensitivity often involve repeated treatment and testing with a single dose (eg, Todtenkopf and Carlezon, 2006) and thus are beyond the scope of the present work.
Role of the PFC in Attention
The 5CSRTT quantifies sustained visuospatial attention and impulse control in rats and is analogous to the CPT used to quantify sustained attention in humans (Robbins, 2002). We observed that over-activation and inactivation of a region encompassing both dorsal and ventral portions of the medial PFC resulted in dissociable deficits in the 5CSRTT. We used alterations in the expression of Fos as an index of changes in the activity of these regions. Although Fos is widely accepted as an indicator of neuronal activation, there are limitations of this approach: as one example, Fos induction can occur by activation of intracellular signaling pathways that do not necessarily lead to neuronal activation (Hoffman and Lyo, 2002). This concern is mitigated in the present studies because the effects of MUS and BMI on cell activity are well characterized (Majchrzak and Di Scala, 2000; Sawaguchi et al, 1989) and the direction of our effects corresponds with existing literature on the effects of these drugs. Over-activation of the medial PFC impaired accuracy and increased omissions suggesting an attentional deficit, while inactivation of the medial PFC increased premature responding suggesting increased impulsive behavior. This contrasts with previous observations following excitotoxic lesions: large lesions encompassing both dorsal and ventral subregions of the medial PFC lead to deficits in both cognitive domains, while those restricted to dorsal subregions (eg, anterior cingulated cortex and/or PrL) induce attentional deficits and those restricted to ventral subregions (IL and/or orbitofrontal cortex) induce impulsive behavior (Chudasama et al, 2003; Passetti et al, 2002; Pezze et al, 2009; Muir et al, 1996). It is not entirely clear why temporary inactivation and excitotoxic lesions would result in disparate performance deficits in the 5CSRTT, but the discrepancy might be explained by compensatory changes that occur in projection areas following medial PFC lesions. The PFC has top-down control over a number of subcortical structures with a putative role in cognitive behavior (eg, nucleus accumbens (NAc) and hippocampus); long-term removal of this control may alter firing patterns in these structures. For example, Pezze et al (2009) suggested that both the attentional and impulse control deficits resulting from large medial PFC lesions are the result of increased D2 receptor activation in the NAc. In contrast, temporary inactivation of the PFC decreases DA release, and hence receptor activation, in the NAc (Murase et al, 1993). Regardless, our Fos studies provide the basis for future studies in which electrophysiological techniques are used to link changes in cellular activity with behavior.
Although our data indicate that the medial PFC mediates attention, they also suggest that it is not necessary for optimal attention in well-trained animals. When the medial PFC was temporarily taken ‘off-line’ by high doses of MUS, attention was not impaired. In well-trained rats, subcortical structures may be sufficient to maintain attention via habit-like responding (Yin and Knowlton, 2006; (Killcross and Coutureau, 2003). In contrast, attention was impaired when the PFC was non-specifically over-activated by BMI infusions. Not only would this over-activation disrupt neural synchrony within the PFC microcircuitry, but it would also disrupt synchrony within PFC target areas such as the NAc and hippocampus. It has been proposed that optimal attentional performance results from specific activation of ‘task-relevant’ pyramidal neurons and suppression of ‘task-irrelevant’ pyramidal neurons by GABA-mediated recurrent inhibition (Winterer and Weinberger, 2004); effectively this would result in activation of specific neurons in medial PFC target areas. Thus over-activation and asynchrony in the PFC would effectively lead to disruptions in neural synchrony within target structures. Currently, it is unclear if one specific projection area underlies the attentional deficits observed following PFC over-activation or whether these deficits result from disruptions across the entire neural network.
The current experiments provide new insight on how manipulations that affect intracellular signaling processes may cause attentional deficits. For example, disrupting the function of cyclic-AMP-dependent protein kinase (PKA) or its downstream target CREB (cyclic-AMP response element-binding protein) within the PFC decreases accuracy and increases omissions in the 5CSRTT (Paine et al, 2009). Decreasing either PKA or CREB function decreases neuronal excitability (Dong et al, 2006; Lopez de Armentia et al, 2007; Trantham-Davidson et al, 2007), but the manipulations used are not cell-type specific and may therefore decrease firing of either pyramidal neurons or GABA interneurons. Given the similarity between the attentional deficits observed following disruption of the PKA signaling pathway and those following GABAA receptor antagonism, we speculate that disruption of either PKA or CREB function cause attentional deficits as a result of reduced GABA-mediated inhibition.
Although the goal of the current experiment was to investigate the putative role in GABAA receptors in the attentional deficits observed in schizophrenia, attentional deficits are also involved in other psychiatric disorders (eg, bipolar disorder, ADHD). Dysregulation of neuronal firing could result from dysfunction in a variety of neurotransmitter systems (eg, dopamine and acetylcholine). Thus, although other psychiatric disorders may have different pathologies, the net effect of these pathologies may result in cortical asynchrony and hence attentional deficits.
Role of the PFC in Impulsive Behavior and Reward
The medial PFC, through its interactions with the NAc and ventral tegmental area (VTA), is postulated to regulate both impulsive behavior (Pattij et al, 2007; Pezze et al, 2007, 2009) and sensitivity to reward (Tzschentke, 2000). Moreover, impulsive action is hypothesized to be regulated, at least in part, by an increased motivation to obtain rewards (Fineberg et al, 2010). In the current experiment, we observed a dissociation between cortical manipulations that affected impulsive behavior and those that affected reward sensitivity. Temporary inactivation of the medial PFC increased impulsive behavior without affecting sensitivity to reward, while over-action of the medial PFC increased sensitivity to reward without affecting impulsive behavior. Thus, at least in the context of the 5CSRTT and ICSS, it appears that impulsivity and reward sensitivity can vary independently of one another.
Increased premature responding following temporary inactivation of the medial PFC is consistent with the hypothesized role of this brain area in the regulation of impulsive behavior or the tendency toward rapid, unplanned actions (for review, see Fineberg et al (2010)). Moreover, our findings are consistent with the observed increase in premature responding in the 5CSRTT following excitotoxic lesions of ventral portions of the medial PFC (Chudasama et al, 2003; Passetti et al, 2002; Pezze et al, 2009) and with the observed increase in premature responding during a ‘waiting task’ following temporary inactivation of the PFC (Narayanan et al, 2006). The effects of excitotoxic lesions on premature responding have been attributed to increased activation of D2 receptors in the NAc. Indeed, D2 receptor antagonist infusions into the NAc normalize impulsive behavior (Pezze et al, 2009). Temporary inactivation of the PFC, however, would be expected to decrease, rather than increase, NAc DA (Musare et al, 1993, see below). Thus, the same mechanism cannot account for increased premature responding following temporary inactivation of the medial PFC. Nonetheless, temporary inactivation and increased NAc DA following cortical excitotoxic lesions may ultimately have the same effect on NAc medium spiny neurons (MSNs)—namely a reduction in firing rate. A reduction in excitatory drive to the NAc reduces MSN firing rate, as does increased D2 receptor activation (Carlezon and Thomas, 2009; Surmeier et al, 2007). Thus, reductions in MSN firing rate may underlie impulsive behavior that is observed following removal of the medial PFC.
Over-activation of the medial PFC increased sensitivity to reward. The regulation of reward by the medial PFC is thought to occur through a multisynaptic pathway involving the VTA. Indeed, intra-PFC BMI infusions enhance burst firing of putative VTA DA neurons (Enomoto et al, 2011). Furthermore, electrical stimulation of the PFC increases DA release in the NAc, an effect that can be attenuated via blockade of glutamate receptors in the VTA (Taber et al, 1995). Similarly, application of glutamate to the PFC increases burst firing of VTA neurons and increases DA release in the NAc, while application of a local anesthetic to the PFC inhibits VTA neuron firing and reduces DA release in the NAc (Murase et al, 1993).
Conclusions
Acute blockade of cortical GABAA receptors increased PFC activity and caused attentional deficits in the 5CSRTT. These findings add to a growing body of evidence supporting a role for GABA neuron dysfunction in the cognitive deficits observed in schizophrenia (see Lewis et al (2005)). Attentional deficits are often observed in adolescents that are at-risk for developing schizophrenia before the onset of other signs of the disorder; following their onset, these deficits are stable across the course of illness (Cornblatt and Malhotra, 2001; Chen and Faraone, 2000). Our studies in adult rats provide the basis for future research that examines the neurodevelopmental role of GABA dysfunction in the etiology of attentional deficits observed in schizophrenia. In addition, we show that the utility of full GABAA receptor agonists to treat such deficits is hampered the emergence unique cognitive deficits, raising the possibility that positive allosteric modulators at GABAA receptors might represent an alternative method by which alterations in GABA receptor function could be utilized to reverse cognitive deficits in this schizophrenia.
References
Bartos M, Vida I, Jonas P (2007). Synaptic mechanisms of synchronized gamma oscillations in inhibitory interneuron networks. Nat Rev Neurosci 8: 45–56.
Benes FM (2010). Amygdalocortical circuitry in schizophrenia: from circuits to molecules. Neuropsychopharmacology 35: 239–257.
Carlezon Jr WA, Chartoff EH (2007). Intracranial self-stimulation (ICSS) in rodents to study the neurobiology of motivation. Nat Protocols 2: 2987–2995.
Carlezon Jr WA, Thomas MJ (2009). Biological substrates of reward and aversion: a nucleus accumbens activity hypothesis. Neuropharmacology 56 (Suppl 1): 122–132.
Chen WJ, Faraone SV (2000). Sustained attention deficits as markers of genetic susceptibility to schizophrenia. Am J Med Genet C Semin Med Genet 97: 52–57.
Cho RY, Konecky RO, Carter CS (2006). Impairments in frontal cortical gamma synchrony and cognitive control in schizophrenia. Proc Natl Acad Sci USA 103: 19878–19883.
Chudasama Y, Passetti F, Rhodes SE, Lopian D, Desai A, Robbins TW (2003). Dissociable aspects of performance on the 5-choice serial reaction time task following lesions of the dorsal anterior cingulate, infralimbic and orbitofrontal cortex in the rat: differential effects on selectivity, impulsivity and compulsivity. Behav Brain Res 146: 105–119.
Cornblatt BA, Malhotra AK (2001). Impaired attention as an endophenotype for molecular genetic studies of schizophrenia. Am J Med Genet B Neuropsychiatr Genet 105: 11–15.
Damgaard T, Plath N, Neill JC, Hansen SL (2011). Extrasynaptic GABA(A) receptor activation reverses recognition memory deficits in an animal model of schizophrenia. Psychopharmacology (Berl) 214: 403–413.
Dong Y, Green T, Saal D, Marie H, Neve R, Nestler EJ et al (2006). CREB modulates excitability of nucleus accumbens neurons. Nat Neurosci 9: 475–477.
Enomoto T, Tse MT, Floresco SB (2011). Reducing gamma-aminobutyric acid induces cognitive, behavioral, and dopaminergic neuron abnormalities that resemble schizophrenia. Biol Psychiatry 69: 432–441.
Fineberg NA, Potenza MN, Chamberlain SR, Berlin HA, Menzies L, Bechara A et al (2010). Probing compulsive and impulsive behaviors, from animal models to endophenotypes: a narrative review. Neuropsychopharmacology 35: 591–604.
Gonzalez-Burgos G, Lewis DA (2008). GABA neurons and the mechanisms of network oscillations: implications for understanding cortical dysfunction in schizophrenia. Schizophr Bull 34: 944–961.
Green MF, Kern RS, Heaton RK (2004). Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophr Res 72: 41–51.
Gruber T, Müller MM, Keil A, Elbert T (1999). Selective visual-spatial attention alters induced gamma band responses in the human EEG. Clin Neurophysiol 110: 2074–2085.
Hoffman GE, Lyo D (2002). Anatomical markers of activity in neuroendocrine systems: are we all ‘fos-ed out’? J Neuroendocrinol 14: 259–268.
Killcross S, Coutureau E (2003). Coordination of actions and habits in the medial prefrontal cortex of rats. Cereb Cortex 13: 400–408.
Lewis DA, Hashimoto T, Volk DW (2005). Cortical inhibitory neurons and schizophrenia. Nat Rev Neurosci 6: 312–324.
Lopez de Armentia M, Jancic D, Olivares R, Alarcon JM, Kandel ER, Barco A (2007). cAMP response element-binding protein-mediated gene expression increases the intrinsic excitability of CA1 pyramidal neurons. J Neurosci 27: 13909–13918.
Majchrzak M, Di Scala G (2000). GABA and muscimol as reversible inactivation tools in learning and memory. Neural Plast 7: 19–29.
Markram H, Toledo-Rodriguez M, Wang Y, Gupta A, Silderberg G, Wu C (2004). Interneurons of the cortical inhibitory system. Nat Rev Neurosci 5: 793–807.
Muir JL, Everitt BJ, Robbins TW (1996). The cerebral cortex of the rat and visual attentional function: dissociable effects of mediofrontal, cingulated, anterior dorsolateral, and parietal cortex lesion on a five-choice serial reaction time task. Cereb Cortex 6: 470–481.
Murase S, Grenhoff J, Chouvet G, Gonon FG, Svensson TH (1993). Prefrontal cortex regulates burst firing and transmitter release in rat mesolimbic dopamine neurons studied in vivo. Neurosci Lett 157: 53–56.
Narayanan NS, Horst NK, Lauback M (2006). Reversible inactivations of the rat medial prefrontal cortex impair the ability to wait for a stimulus. Neuroscience 139: 865–876.
National Academy Press (1996). Guide for the Care and Use of Laboratory Animals. National Academy Press: Washington, DC.
Paine TA, Carlezon Jr WA (2009). Effects of antipsychotic drugs on MK-801-induced attentional and motivational deficits in rats. Neuropharmacology 56: 788–797.
Paine TA, Neve RL, Carlezon Jr WA (2009). Attention deficits and hyperactivity following inhibition of cAMP-dependent protein kinase (PKA) within the medial prefrontal cortex of rats. Neuropsychopharmacology 34: 2143–2155.
Paine TA, Tomasiewicz HC, Zhang K, Carlezon Jr WA (2007). Sensitivity of the five-choice serial reaction time task to the effects of various psychotropic drugs in Sprague-Dawley rats. Biol Psychiatry 62: 687–693.
Passetti F, Chudasama Y, Robbins TW (2002). The frontal cortex of the rat and visual attentional performance: dissociable functions of distinct medial prefrontal subregions. Cereb Cortex 12: 1254–1268.
Passetti F, Dalley JW, Robbins TW (2003a). Double dissociation of serotonergic and dopaminergic mechanisms on attentional performance using a rodent five-choice reaction time task. Psychopharmacology (Berl) 165: 136–145.
Passetti F, Levita L, Robbins TW (2003b). Sulpiride alleviates the attentional impairments of rats with medial prefrontal cortex lesions. Behav Brain Res 138: 59–69.
Pattij T, Janssen MCW, Vanderschuren LJMJ, Schoffelmeer ANM, van Gaalen MM (2007). Involvement of dopamine D1 and D2 receptors in the nucleus accumbens core and shell in inhibitory response control. Psychopharmacology (Berl) 191: 587–598.
Paxinos G, Watson C (1997). The Rat Brain in Stereotaxic Coordinates, 3rd edn. Academic Press: Orlando, FL.
Pezze MA, Dalley JW, Robbins TW (2007). Differential roles of dopamine D1 and D2 receptors in the nucleus accumbens in attentional performance on the five-choice serial reaction time task. Neuropsychopharmacology 32: 273–283.
Pezze MA, Dalley JW, Robbins TW (2009). Remediation of attentional dysfunction in rats with lesions of the medial prefrontal cortex by intra-accumbens administration of the dopamine D2/3 receptor antagonist sulpiride. Psychopharmacology (Berl) 202: 307–313.
Robbins TW (2002). The 5-choice serial reaction time task: behavioural pharmacology and functional neurochemistry. Psychopharmacology (Berl) 163: 362–380.
Sawaguchi T, Matsumura M, Kubota K (1989). Delayed response deficits produced by local injection of bicuculline into the dorsolateral prefrontal cortex in Japanese macaque monkeys. Exp Brain Res 75: 457–469.
Steinmetz PN, Roy A, Fitzgerald PJ, Hsiao SS, Johnson KO, Niebur E (2000). Attention modulates synchronized neuronal firing in primate somatosensory cortex. Nature 404: 187–190.
Surmeier DJ, Ding J, Day M, Wang Z, Shen W (2007). D1 and D2 dopamine-receptor modulation of striatal glutamatergic signaling in striatal medium spiny neurons. Trends Neurosci 30: 228–235.
Taber MT, Das S, Fibiger HC (1995). Cortical regulation of subcortical dopamine release: mediation via the ventral tegmental area. J Neurochem 65: 1407–1410.
Todtenkopf MS, Carlezon Jr WA (2006). Contribution of drug doses and conditioning periods to psychomotor stimulant sensitization. Psychopharmacology (Berl) 185: 451–458.
Trantham-Davidson H, Kröner S, Seamans JK (2007). Dopamine modulation of prefrontal cortex interneurons occurs independently of DARPP-32. Cereb Cortex 18: 951–958.
Tzschentke TM (2000). The medial prefrontal cortex as a part of the brain reward system. Amino Acids 19: 211–219.
Volk D, Austin M, Pierri J, Sampson A, Lewis D (2001). GABA transporter-1 mRNA in the prefrontal cortex in schizophrenia: decreased expression in a subset of neurons. Am J Psychiatry 158: 256–265.
Volk DW, Austin MC, Pierri JN, Sampson AR, Lewis DA (2000). Decreased glutamic acid decarboxylase67 messenger RNA expression in a subset of prefrontal cortical gamma-aminobutyric acid neurons in subjects with schizophrenia. Arch Gen Psychiatry 57: 237–245.
White EL (1989). Cortical Circuits: Synaptic Organization of the Cerebral Cortex, Structure, Function and Theory. Birkhauser: Boston, MA.
Winterer G, Weinberger DR (2004). Genes, dopamine and cortical signal-to-noise ratio in schizophrenia. Trends Neurosci 27: 683–690.
Yin HH, Knowlton BJ (2006). The role of the basal ganglia in habit formation. Nat Rev 7: 464–476.
Acknowledgements
Funded by a NARSAD Young Investigator Award (to TAP) and a grant from the National Institute of Mental Health (MH063266 to WAC). We would like to thank Anna Frackman and Lindsay Boven for their technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Carlezon holds US patents for novel treatments for depressive disorders. He has received compensation from Huya Bioscience, Infinity Pharmaceuticals, Lantheus, Myneurolab.com, Psychogenics, and Transcept within the last 3 years.
Rights and permissions
About this article
Cite this article
Paine, T., Slipp, L. & Carlezon, W. Schizophrenia-Like Attentional Deficits Following Blockade of Prefrontal Cortex GABAA Receptors. Neuropsychopharmacol 36, 1703–1713 (2011). https://doi.org/10.1038/npp.2011.51
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2011.51
Keywords
This article is cited by
-
Control of sustained attention and impulsivity by Gq-protein signalling in parvalbumin interneurons of the anterior cingulate cortex
Translational Psychiatry (2023)
-
Disinhibition of the prefrontal cortex leads to brain-wide increases in neuronal activation that are modified by spatial learning
Brain Structure and Function (2019)
-
Adolescent THC Exposure Causes Enduring Prefrontal Cortical Disruption of GABAergic Inhibition and Dysregulation of Sub-Cortical Dopamine Function
Scientific Reports (2017)
-
Genetic Polymorphism of GABRR2 Modulates Individuals’ General Cognitive Ability in Healthy Chinese Han People
Cellular and Molecular Neurobiology (2017)
-
Regulation of sustained attention, false alarm responding and implementation of conditional rules by prefrontal GABAA transmission: comparison with NMDA transmission
Psychopharmacology (2017)