Abstract
The development of personalized cancer therapy depends on a robust system to monitor the patient's individual response to anticancer treatment. Anticancer drug efficacy has been tested on circulating tumor cells (CTCs) derived from patient blood samples after ex vivo expansion into CTC clusters. Current attempts to culture these primary cancer cells focus on long-term maintenance under growth factor supplements into cell lines, which usually takes >6 months and results in a CTC expansion efficiency of <20%. We recently developed a simple but unique microfluidics-based culture approach that requires minimal preprocessing (∼30 min) and does not require prior enrichment of CTCs or depend on the use of growth factor supplements. The approach capitalizes on co-culture of immune cells from the same patient blood sample within specially designed microwells that promote CTC cluster formation within 2 weeks, with an overall cluster formation success rate of ∼50%. Drug screening is facilitated by the incorporation of a gradient generator for parallel exposure to two or more drugs at various concentrations. Owing to the cost-effectiveness and less-invasive nature of this procedure, routine monitoring of disease progression can be achieved. The described microfluidics system can be operated with a single syringe pump to introduce drug compounds (which takes ∼6 min), followed by incubation of the CTC clusters for 48 h before analysis. In addition to its applications in biomedical research, the rapid readout of our platform will enable clinicians to assess or predict a patient's response to various therapeutic strategies, so as to enable personalized or precision therapy.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Torre, L.A. et al. Global cancer statistics, 2012. CA Cancer J. Clin. 65, 87–108 (2015).
Jemal, A. et al. Global cancer statistics. CA Cancer J. Clin. 61, 69–90 (2011).
Gambhir, S.S. Molecular imaging of cancer with positron emission tomography. Nat. Rev. Cancer 2, 683–693 (2002).
Gambarin-Gelwan, M., Wolf, D.C., Shapiro, R., Schwartz, M.E. & Min, A.D. Sensitivity of commonly available screening tests in detecting hepatocellular carcinoma in cirrhotic patients undergoing liver transplantation. Am. J. Gastroenterol. 95, 1535–1538 (2000).
Jeffries, D.O. et al. Surgical biopsy is still necessary for BI-RADS 4 calcifications found on digital mammography that are technically too faint for stereotactic core biopsy. Breast Cancer Res. Treat. 154, 557–561 (2015).
Mathenge, E.G. et al. Core needle biopsy of breast cancer tumors increases distant metastases in a mouse model. Neoplasia 16, 950–960 (2014).
Gupta, G.P. & Massagué, J. Cancer metastasis: building a framework. Cell 127, 679–695 (2006).
van de Stolpe, A., Pantel, K., Sleijfer, S., Terstappen, L.W. & den Toonder, J.M. Circulating tumor cell isolation and diagnostics: toward routine clinical use. Cancer Res. 71, 5955–5960 (2011).
Adalsteinsson, V.A. & Love, J.C. Toward engineered processes for sequencing-based analysis of single circulating tumor cells. Curr. Opin. Chem. Eng. 4, 97–104 (2014).
Racila, E. et al. Detection and characterization of carcinoma cells in the blood. Proc. Natl. Acad. Sci. USA 95, 4589–4594 (1998).
Fehm, T. et al. Determination of HER2 status using both serum HER2 levels and circulating tumor cells in patients with recurrent breast cancer whose primary tumor was HER2 negative or of unknown HER2 status. Breast Cancer Res. 9, R74 (2007).
Gerlinger, M. et al. Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N. Engl. J. Med. 366, 883–892 (2012).
Khoo, B.L. et al. Single-cell profiling approaches to probing tumor heterogeneity. Int. J. Cancer 139, 243–255 (2016).
Khoo, B.L. et al. Liquid biopsy and therapeutic response: circulating tumor cell cultures for evaluation of anticancer treatment. Sci. Adv. 2, e1600274 (2016).
Yu, M. et al. Cancer therapy. Ex vivo culture of circulating breast tumor cells for individualized testing of drug susceptibility. Science 345, 216–220 (2014).
Zhang, L. et al. The identification and characterization of breast cancer CTCs competent for brain metastasis. Sci. Transl. Med. 5, 180ra148 (2013).
Gao, D. et al. Organoid cultures derived from patients with advanced prostate cancer. Cell 159, 176–187 (2014).
Maheswaran, S. & Haber, D.A. Ex vivo culture of CTCs: an emerging resource to guide cancer therapy. Cancer Res. 75, 2411–2415 (2015).
Baccelli, I. et al. Identification of a population of blood circulating tumor cells from breast cancer patients that initiates metastasis in a xenograft assay. Nat. Biotechnol. 31, 539–544 (2013).
Fidler, I.J. Metastasis: quantitative analysis of distribution and fate of tumor emboli labeled with 125 I-5-iodo-2′-deoxyuridine. J. Natl. Cancer Inst. 45, 773–782 (1970).
Mak, I.W., Evaniew, N. & Ghert, M. Lost in translation: animal models and clinical trials in cancer treatment. Am. J. Transl. Res. 6, 114–118 (2014).
Hutchinson, L. & Kirk, R. High drug attrition rates--where are we going wrong? Nat. Rev. Clin. Oncol. 8, 189–190 (2011).
Joyce, J.A. & Fearon, D.T. T cell exclusion, immune privilege, and the tumor microenvironment. Science 348, 74–80 (2015).
Hwang, R.F. et al. Cancer-associated stromal fibroblasts promote pancreatic tumor progression. Cancer Res. 68, 918–926 (2008).
Hughes, C.S., Postovit, L.M. & Lajoie, G.A. Matrigel: a complex protein mixture required for optimal growth of cell culture. Proteomics 10, 1886–1890 (2010).
Berdel, W.E., Danhauser-Riedl, S., Steinhauser, G. & Winton, E.F. Various human hematopoietic growth factors (interleukin-3, GM-CSF, G-CSF) stimulate clonal growth of nonhematopoietic tumor cells. Blood 73, 80–83 (1989).
Yu, M. et al. Ex vivo culture of circulating breast tumor cells for individualized testing of drug susceptibility. Science 345, 216–220 (2014).
Jiao, Y. & Torquato, S. Emergent behaviors from a cellular automaton model for invasive tumor growth in heterogeneous microenvironments. PLoS Comput. Biol. 7, e1002314 (2011).
Pantel, K. & Riethdorf, S. Pathology: are circulating tumor cells predictive of overall survival? Nat. Rev. Clin. Oncol. 6, 190–191 (2009).
Khoo, B.L. et al. Short-term expansion of breast circulating cancer cells predicts response to anti-cancer therapy. Oncotarget 6, 15578–15593 (2015).
Cayrefourcq, L. et al. Establishment and characterization of a cell line from human circulating colon cancer cells. Cancer Res. 75, 892–901 (2015).
Allan, A.L. & Keeney, M. Circulating tumor cell analysis: technical and statistical considerations for application to the clinic. J. Oncol. 2010, 426218 (2010).
Thiery, J.P. & Lim, C.T. Tumor dissemination: an EMT affair. Cancer Cell 23, 272–273 (2013).
Maheswaran, S. et al. Detection of mutations in EGFR in circulating lung-cancer cells. N. Engl. J. Med. 359, 366–377 (2008).
Riethdorf, S. et al. Detection and HER2 expression of circulating tumor cells: prospective monitoring in breast cancer patients treated in the neoadjuvant GeparQuattro trial. Clin. Cancer Res. 16, 2634–2645 (2010).
Lara, O., Tong, X., Zborowski, M. & Chalmers, J.J. Enrichment of rare cancer cells through depletion of normal cells using density and flow-through, immunomagnetic cell separation. Exp. Hematol. 32, 891–904 (2004).
Sollier, E. et al. Size-selective collection of circulating tumor cells using Vortex technology. Lab. Chip. 14, 63–77 (2014).
Khoo, B.L. et al. Clinical validation of an ultra high-throughput spiral microfluidics for the detection and enrichment of viable circulating tumor cells. PloS One 9, e99409 (2014).
Moon, H.S. et al. Continuous separation of breast cancer cells from blood samples using multi-orifice flow fractionation (MOFF) and dielectrophoresis (DEP). Lab. Chip. 11, 1118–1125 (2011).
Huang, R.Y. et al. An EMT spectrum defines an anoikis-resistant and spheroidogenic intermediate mesenchymal state that is sensitive to e-cadherin restoration by a src-kinase inhibitor, saracatinib (AZD0530). Cell Death Dis. 4, e915 (2013).
Ozkumur, E. et al. Inertial focusing for tumor antigen–dependent and–independent sorting of rare circulating tumor cells. Sci. Transl. Med. 5, 179ra147 (2013).
Munz, M. et al. Side-by-side analysis of five clinically tested anti-EpCAM monoclonal antibodies. Cancer Cell Int. 10, 44 (2010).
Wong, A.D. & Searson, P.C. Live-cell imaging of invasion and intravasation in an artificial microvessel platform. Cancer Res. 74, 4937–4945 (2014).
Liu, P.-f. et al. A bladder cancer microenvironment simulation system based on a microfluidic co-culture model. Oncotarget 6, 37695–37705 (2015).
Trietsch, S.J., Israëls, G.D., Joore, J., Hankemeier, T. & Vulto, P. Microfluidic titer plate for stratified 3D cell culture. Lab. Chip. 13, 3548–3554 (2013).
Napolitano, A. et al. Scaffold-free three-dimensional cell culture utilizing micromolded nonadhesive hydrogels. BioTechniques 43, 494–500 (2007).
Xu, Z. et al. Application of a microfluidic chip-based 3D co-culture to test drug sensitivity for individualized treatment of lung cancer. Biomaterials 34, 4109–4117 (2013).
Zhang, Z. et al. Expansion of CTCs from early stage lung cancer patients using a microfluidic co-culture model. Oncotarget 5, 12383 (2014).
Choi, Y. et al. A microengineered pathophysiological model of early-stage breast cancer. Lab. Chip. 15, 3350–3357 (2015).
Kalluri, R. & Zeisberg, M. Fibroblasts in cancer. Nat. Rev. Cancer 6, 392–401 (2006).
Carmeliet, P. & Jain, R.K. Angiogenesis in cancer and other diseases. Nature 407, 249–257 (2000).
Infanger, D.W., Lynch, M.E. & Fischbach, C. Engineered culture models for studies of tumor-microenvironment interactions. Annu. Rev. Biomed. Eng. 15, 29–53 (2013).
Nagrath, S. et al. Isolation of rare circulating tumour cells in cancer patients by microchip technology. Nature 450, 1235–1239 (2007).
Stott, S.L. et al. Isolation of circulating tumor cells using a microvortex-generating herringbone-chip. Proc. Natl. Acad. Sci. USA 107, 18392–18397 (2010).
Riethdorf, S. et al. Detection of circulating tumor cells in peripheral blood of patients with metastatic breast cancer: a validation study of the cellsearch system. Clin. Cancer Res. 13, 920 (2007).
Warkiani, M.E. et al. An ultra-high-throughput spiral microfluidic biochip for the enrichment of circulating tumor cells. Analyst 139, 3245–3255 (2014).
Butler, T.P. & Gullino, P.M. Quantitation of cell shedding into efferent blood of mammary adenocarcinoma. Cancer Res. 35, 512–516 (1975).
Deng, G. et al. Enrichment with anti-cytokeratin alone or combined with anti-EpCAM antibodies significantly increases the sensitivity for circulating tumor cell detection in metastatic breast cancer patients. Breast Cancer Res. 10, R69 (2008).
Hur, S.C., Henderson-MacLennan, N.K., McCabe, E.R. & Di Carlo, D. Deformability-based cell classification and enrichment using inertial microfluidics. Lab. Chip. 11, 912–920 (2011).
Zheng, S. et al. 3D microfilter device for viable circulating tumor cell (CTC) enrichment from blood. Biomed. Microdev. 13, 203–213 (2011).
Lu, X. & Kang, Y. Hypoxia and hypoxia-inducible factors: master regulators of metastasis. Clin. Cancer Res. 16, 5928–5935 (2010).
Fidler, I.J. The pathogenesis of cancer metastasis: the 'seed and soil' hypothesis revisited. Nat. Rev. Cancer 3, 453–458 (2003).
Vaupel, P., Thews, O., Kelleher, D.K. & Hoeckel, M. Current status of knowledge and critical issues in tumor oxygenation. Results from 25 years research in tumor pathophysiology. Adv. Exp. Med. Biol. 454, 591–602 (1998).
Soeda, A. et al. Hypoxia promotes expansion of the CD133-positive glioma stem cells through activation of HIF-1alpha. Oncogene 28, 3949–3959 (2009).
Noy, R. & Pollard, J.W. Tumor-associated macrophages: from mechanisms to therapy. Immunity 41, 49–61 (2014).
Spellman, P.T. & Gray, J.W. Detecting cancer by monitoring circulating tumor DNA. Nat. Med. 20, 474–475 (2014).
Yu, M. et al. Circulating breast tumor cells exhibit dynamic changes in epithelial and mesenchymal composition. Science 339, 580–584 (2013).
Payne, R. et al. Viable circulating tumour cell detection using multiplex RNA in situ hybridisation predicts progression-free survival in metastatic breast cancer patients. Br. J. Cancer 106, 1790–1797 (2012).
Cristofanilli, M. et al. Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N. Engl. J. Med. 351, 781–791 (2004).
Hayes, D.F. et al. Circulating tumor cells at each follow-up time point during therapy of metastatic breast cancer patients predict progression-free and overall survival. Clin. Cancer Res. 12, 4218–4224 (2006).
Soothill, J.S., Ward, R. & Girling, A.J. The IC50: an exactly defined measure of antibiotic sensitivity. J. Antimicrob. Chemother. 29, 137–139 (1992).
Pettinato, G., Wen, X. & Zhang, N. Formation of well-defined embryoid bodies from dissociated human induced pluripotent stem cells using microfabricated cell-repellent microwell arrays. Sci. Rep. 4, 7402 (2014).
Fukuda, J. et al. Micromolding of photocrosslinkable chitosan hydrogel for spheroid microarray and co-cultures. Biomaterials 27, 5259–5267 (2006).
Tu, T.Y. et al. Rapid prototyping of concave microwells for the formation of 3D multicellular cancer aggregates for drug screening. Adv. Healthcare Mater. 3, 609–616 (2014).
Kumar, N. et al. Intraoperative cell salvage in metastatic spine tumour surgery reduces potential for reinfusion of viable cancer cells. Eur. Spine J. 25, 4008–4015 (2016).
Wong, A.L. et al. Phase II study of neoadjuvant weekly paclitaxel and carboplatin with lapatinib in HER2+ breast cancer. J. Clin. Oncol. 32, 619–619 (2014).
Friedl, P. & Gilmour, D. Collective cell migration in morphogenesis, regeneration and cancer. Nat. Rev. Mol. Cell Biol. 10, 445–457 (2009).
Al-Hajj, M., Wicha, M.S., Benito-Hernandez, A., Morrison, S.J. & Clarke, M.F. Prospective identification of tumorigenic breast cancer cells. Proc. Natl. Acad. Sci. USA 100, 3983–3988 (2003).
Eyler, C.E. & Rich, J.N. Survival of the fittest: cancer stem cells in therapeutic resistance and angiogenesis. J. Clin. Oncol. 26, 2839–2845 (2008).
Kang, M.K. & Kang, S.K. Tumorigenesis of chemotherapeutic drug-resistant cancer stem-like cells in brain glioma. Stem Cells Dev. 16, 837–847 (2007).
Sharma, S.V. et al. A chromatin-mediated reversible drug-tolerant state in cancer cell subpopulations. Cell 141, 69–80 (2010).
Singh, A. & Settleman, J. EMT, cancer stem cells and drug resistance: an emerging axis of evil in the war on cancer. Oncogene 29, 4741–4751 (2010).
Li, X. et al. Intrinsic resistance of tumorigenic breast cancer cells to chemotherapy. J. Natl. Cancer Inst. 100, 672–679 (2008).
Lee, J.-H., Choi, W.-S., Lee, K.-H. & Yoon, J.-B. A simple and effective fabrication method for various 3D microstructures: backside 3D diffuser lithography. J. Micromech. Microeng. 18, 125015–125017 (2008).
Whitesides, G.M. & Tang, S.K.Y. Basic Microfluidic and Soft Lithographic Techniques Vol. 2 (New Technical, 2009).
Raval, P.J., Carter, D.P. & Fairbanks, G. Relationship of hemolysis buffer structure, pH and ionic strength to spontaneous contour smoothing of isolated erythrocyte membranes. Biochim. Biophys. Acta 983, 230–240 (1989).
Al-Lazikani, B., Banerji, U. & Workman, P. Combinatorial drug therapy for cancer in the post-genomic era. Nat. Biotechnol. 30, 679–692 (2012).
Borgen, E. et al. Standardization of the immunocytochemical detection of cancer cells in BM and blood: I. establishment of objective criteria for the evaluation of immunostained cells. Cytotherapy 1, 377–388 (1999).
Acknowledgements
We express our sincere gratitude to all volunteers who participated in this trial and donated blood samples for characterization of our device. The clinical samples and data collection were supported by a Singapore National Medical Research Council (NMRC) grant. This work was also supported by the Mechanobiology Institute and the Singapore–MIT Alliance for Research and Technology (SMART) BioSystems and Micromechanics (BioSyM) Interdisciplinary Research Groups (IRGs), which are funded by the National Research Foundation, Prime Minister's Office, Singapore, under CREATE.
Author information
Authors and Affiliations
Contributions
B.L.K. and G.G. conceived and designed the experiments. B.L.K., G.G. and Y.B.L. performed the experiments. C.T.L., S.C.L. and J.H. contributed by providing reagents, materials and analysis tools. B.L.K., G.G., Y.B.L., S.C.L., J.H. and C.T.L. wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Integrated supplementary information
Supplementary Figure 1 Optimization of microwell fabrication.
(A) Schematics illustrating the formation of a microwell. The distance of the laser from the substrate, the speed of laser ablation as well as laser power affects the depth and width of microwell formed. The higher the laser power, the deeper and wider the resultant microwell becomes. The layer of the recast is an artifact generated by the laser process, which becomes prominent with stronger laser power. (B) Phase contrast images of the smallest (left; average inner diameter 50 μm; Scale bar is 50 μm) and largest possible microwell that can be fabricated (middle; average inner diameter 341.5 μm; Scale bar is 100 μm.) with laser-ablation. (Right) Magnified view of the array of microwells with optimal parameters. (C) Simulation results of flow velocity at the entrance of the channel. (left) Cross-sectional slices of the velocity magnitude in the XZ-plane. Coloured scale bar represents the velocity magnitude in mm/s. Red arrows depict the direction of the flow and have lengths that are proportional to the velocity magnitude. (right) Zoomed in view of the panel a where the microwells are. The uniform dark blue colour within the microwells indicate that there is no flow in that region i.e. cells in culture do not experience shear stresses from the flow of fluid entering the channel from the gradient generator.
Supplementary Figure 2 Optimization of microwell parameters.
Phase contrast images of cancer cells seeded into microwells of different average diameters (∼107 μm, 187.5 μm and 341.5 μm from left to right). Images were obtained with a 20X objective lens. Scale bar is 50 μm.
Supplementary Figure 3 Custom tapered microwells for CTC cluster formation.
Clinical samples do not form clusters in conventional round bottom wells (left) but are able to develop clusters consistently in our tapered microwell assay. These clusters can be formed in microwells generated by either laser-ablation (middle) or microfabrication (right).
Supplementary Figure 4 Step 79: Enumeration of cell counts in a fixed area reveal cell packing density.
(a) Cell counts in a fixed area (e.g. 50 μm by 50 μm) are obtained from images of cultures with WBCs from healthy volunteer only and spiked cultures with WBC and cancer cell lines. (b) Spiked cultures start to form aggregates of higher cell density (> 8 cells per 2500 μm2) after only 3 days in culture.
Supplementary Figure 5 Substrate adherence requirement.
(a) Surfactant treatment of polystyrene surfaces is temporary, and spheroids of cell lines cultured in laser-ablated microwells dispersed after three days in culture. N=3. Scale bar is 50 μm. (b) Clinical samples can form loose clusters with microwells of 187.5 μm average diameter in the absence of surfactant treatment. N=3. Scale bar is 50 μm.
Supplementary Figure 6 Step 79: Cluster identification.
(a) Morphological phenotyping of a cluster in laser-ablated microwells using a phase-contrast microscope. Scale bar is 100 μm. (b) Cluster stained in situ with live dye for visualization and quantification of cell density. Scale bar is 100 μm. (c) Clusters demonstrate a region of lower gray scale values, while regions without cells reflect most of the light, leading to high gray scale values. (d) Microfabricated microwells with sparse blood cell monolayer (top) or cluster (bottom) respectively at 10X magnification. Corresponding scatter plots of grey values reflect cell density within the microwell. Microwells with sparse cell density have high grey values within the microwell region, while those with high cell density reflect lower grey values < 50% of peak. Scale bar is 100 μm.
Supplementary Figure 7 Panel of healthy sample cultures.
Cultures of healthy blood samples demonstrate either cell debris (25%) or monolayer of residual blood cells (75%) (n=16). Scale bar is 50 μm.
Supplementary Figure 8 Step 6: Fabrication of the primary mold with elliptical pillars.
(a) The 4” soda lime mask with the elliptical opening patterned in the Cr layer, already coated with the 500-nm thick PMGI sacrificial layer (step 28). (b) SU-8 spin coating of the mask plate. SU-8 3050 is poured carefully on the plate while this is placed on the vacuum chuck of the spin coater (steps 29 and 31). (c) Soft baking of the SU-8 (steps 30 and 32). (d) Loading of the mask (face down) in the UV exposure system. A blank mask plate is placed face up to prevent reflection of the UV light from the bottom, after passing through the SU-8 layer. (e) The opal diffuser is placed on top of the mask (step 33). (f) Development of the mask. When all the unexposed SU-8 has been removed, the plate is cleaned with spraying SU-8 developer first and IPA later, and then dried with gentle nitrogen flow (step 35).
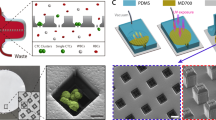
Supplementary Figure 9 Step 34: Soft-lithographic replica of the primary mold.
(a) The mask plate with the SU-8 dome-shaped pillars is placed in a petri dish face up (Step 39). (b) PDMS is poured on the mask (step 40). (c) De-gassing of the PDMS to remove all trapped air. (d) After curing, the PDMS is cut along the mask border with a razor blade (step 43). (e) Using a pair of tweezer, the cured PDMS is gently peeled off from the mask. (f) PDMS replica and original mold after the peeling-off step is completed.
Supplementary Figure 10 Step 37: The soft-lithographic replica of the secondary mold.
(a) Surface activation of the PDMS Secondary mold using oxygen plasma (step 45). (b) The activated PDMS secondary mold is placed in a vacuum jar along with a small quantity of silane for its silanization process (step 45). (c) After the silanization is completed, the Secondary Mold is placed in a petri dish and fresh uncured PDMS is poured (same as in previous image and step 39-40 and 48). Then, after curing the PDMS is cut along the Secondary Mold border with a razor blade (as in step 48) and the replica is gently peeled off. (d) Secondary Mold (right) and its PDMS replica (left)
Supplementary Figure 11 Step 48: Release of PDMS from the mold after curing.
(a) Carefully cut out the PDMS without cutting the SU-8 pattern of the gradient generator. (b) Slide the blade along the inner wall of the aluminum mold for the barrier layer. (c) Cut along the outline of the PDMS replica mold of the microwell layer drawn in Step 50. (d-f) Use the blade to lift the corners of the PDMS from each of the three molds. (g-i) Peel out the gradient generator, barrier and microwell layers from their respective molds.
Supplementary Figure 12 Steps 49 and 50: Preparation of each PDMS layer prior to assembly.
(a) Trim the sides of the gradient generator and punch two vertical holes at the inlets. (b) Cover the top surface of the barrier layer with tape. (c) Flip the barrier layer upside down and cut through the thin layer of PDMS along the length on both sides of each channel. (d) Peel off the tape and use a pair of tweezers to tear out the thin strips of PDMS. (e, f) Place the microwell layer under the barrier layer and align it with the channels in the barrier layer. Trim off the sides of the microwell layer using the edges of the barrier layer as a guide.
Supplementary information
Supplementary Figures and Tables
Supplementary Figures 1–12 and The Supplementary Tutorial. (PDF 5929 kb)
Supplementary Table
Supplementary Table 1 (XLSX 13 kb)
Supplementary Data 1
Design of photolithography mask for gradient generator layer. (ZIP 7230 kb)
Supplementary Data 2
Design of photolithography mask for microwell layer. (ZIP 18 kb)
Supplementary Data 3
CAD file for aluminum mold for barrier layer. (ZIP 96 kb)
Rights and permissions
About this article
Cite this article
Khoo, B., Grenci, G., Lim, Y. et al. Expansion of patient-derived circulating tumor cells from liquid biopsies using a CTC microfluidic culture device. Nat Protoc 13, 34–58 (2018). https://doi.org/10.1038/nprot.2017.125
Published:
Issue Date:
DOI: https://doi.org/10.1038/nprot.2017.125
This article is cited by
-
Ex vivo expansion of circulating tumour cells (CTCs)
Scientific Reports (2023)
-
Analytical device miniaturization for the detection of circulating biomarkers
Nature Reviews Bioengineering (2023)
-
Biology, vulnerabilities and clinical applications of circulating tumour cells
Nature Reviews Cancer (2023)
-
Single-cell metabolic fingerprints discover a cluster of circulating tumor cells with distinct metastatic potential
Nature Communications (2023)
-
Circulating tumor cell-derived preclinical models: current status and future perspectives
Cell Death & Disease (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.