Abstract
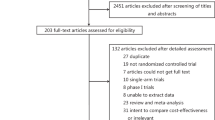
Dose-dense adjuvant breast cancer chemotherapy is a new treatment strategy that aims to improve tumour control by using more frequent cytotoxic dosing together with continuous granulocyte colony-stimulating factor (G-CSF) to minimize neutropaenia. In addition to stimulating neutrophil proliferation, G-CSF mobilizes neutrophils from the bone marrow through proteolytic disruption of the chemokine receptor CXCR4 and its chemotactic ligand CXCL12. As breast cancers also express CXCR4 and oestrogen induces CXCL12, the success of dose-dense treatment could partly reflect inhibition of CXCR4-dependent micrometastatic homing and/or paracrine survival, and suggests a benefit of adjuvant oestrogen suppression for patients with oestrogen-receptor-negative, CXCR4-positive disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Bonadonna, G., Rossi, A., Valagussa, P., Banfi, A. & Veronesi, U. The CMF program for operable breast cancer with positive axillary nodes. Cancer 39, 2904–2915 (1977).
McGuire, W. L., Osborne, C. K., Clark, G. M. & Knight, W. A. Steroid hormone receptors and carcinoma of the breast. Am. J. Physiol. 243, E99–E102 (1982).
Rose, C. et al. Beneficial effect of adjuvant tamoxifen therapy in primary breast cancer patients with high oestrogen receptor values. Lancet 1, 16–19 (1985).
Powles, T. J. et al. Failure of chemotherapy to prolong survival in a group of patients with metastatic breast cancer. Lancet 1, 580–582 (1980).
Early Breast Cancer Trialists Collaborative Group. Effects of adjuvant tamoxifen and of cytotoxic therapy on mortality in early breast cancer. N. Engl. J. Med. 319, 1681–1692 (1988).
Kubota, M. Generation of DNA damage by antineoplastic agents. Anticancer Drugs 2, 531–541 (1991).
Howell, S. & Shalet, S. Gonadal damage from chemotherapy and radiotherapy. Endoc. Metab. Clin. North Am. 27, 927–943 (1998).
Mehta, R. R., Beattie, C. W. & Das Gupta, T. K. Endocrine profile in breast cancer patients receiving chemotherapy. Breast Cancer Res. Treat. 20, 125–132 (1992).
Padmanabhan, N., Howell, A. & Rubens, R. D. Mechanism of action of adjuvant chemotherapy in early breast cancer. Lancet 2, 411–414 (1986).
Poikonen, P., Saarto, T., Elomaa, I., Joensuu, H. & Blomqvist, C. Prognostic effect of amenorrhoea and elevated serum gonadotropin levels induced by adjuvant chemotherapy in premenopausal node-positive breast cancer patients. Eur. J. Cancer 36, 43–48 (2000).
Goldhirsch, A., Gelber, R. D. & Castiglione, M. The magnitude of endocrine effects of adjuvant chemotherapy for premenopausal breast cancer patients. Ann. Oncol. 1, 183–188 (1990).
Early Breast Cancer Trialists Collaborative Group. Polychemotherapy for early breast cancer: an overview of the randomized trials. Lancet 352, 930–942 (1998).
Farquhar, C., Basser, R., Marjoribanks, J. & Lethaby, A. High dose chemotherapy and autologous bone marrow or stem cell transplantation versus conventional chemotherapy for women with early poor prognosis breast cancer. Cochrane Database Syst. Rev. 1, CD003139 (2003).
Budman, D. R. et al. Dose and dose intensity as determinants of outcome in the adjuvant treatment of breast cancer. J. Natl Cancer Inst. 90, 1205–1211 (1998).
Mikhak, B. et al. Long term follow-up of women treated with 16-week dose-intensive adjuvant chemotherapy for high risk breast cancer. Cancer 85, 899–904 (1999).
Kasimir-Bauer, S. et al. Survival of tumor cells in stem cell preparations and bone marrow of patients with high-risk or metastatic breast cancer after receiving dose-intensive or high-dose chemotherapy. Clin. Cancer Res. 7, 1582–1589 (2001).
Braun, S. et al. Lack of effect of adjuvant chemotherapy on the elimination of single dormant tumor cells in bone marrow of high-risk breast cancer patients. J. Clin. Oncol. 18, 80–86 (2000).
Gyllenberg, M. & Webb, G. F. Quiescence as an explanation of Gompertzian tumor growth. Growth Dev. Aging 53, 25–33 (1989).
Pittillo, R. F., Schabel, F. M. & Skipper, H. E. The 'sensitivity' of resting and dividing cells. Cancer Chemother. Rep. 54, 137–142 (1970).
Coldman, A. J. & Goldie, J. H. Impact of dose-intense chemotherapy on the development of permanent drug resistance. Semin. Oncol. 14, 29–33 (1987).
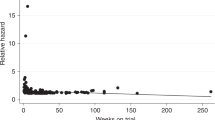
Mayers, C., Panzarella, T. & Tannock I. F. Analysis of the prognostic effects of inclusion in a clinical trial and of myelosuppression on survival after adjuvant chemotherapy for breast carcinoma. Cancer 91, 2246–2257 (2001).
Leonard, R. C., Miles, D., Thomas, R. & Nussey, F. Impact of neutropaenia on delivering planned adjuvant chemotherapy. Br. J. Cancer 89, 2062–2068 (2003).
Cameron, D. A., Massie, C., Kerr, G. & Leonard, R. C. F. Moderate neutropenia with adjuvant CMF confers improved survival in early breast cancer. Br. J. Cancer 89, 1837–1842 (2003).
Ellis, G. K., Livingston, R. B., Gralow, J. R., Green, S. J. & Thompson, T. Dose-dense anthracycline-based chemotherapy for node-positive breast cancer. J. Clin. Oncol. 20, 3637–3643 (2002).
Citron, M. L. et al. Randomized trial of dose-dense versus conventionally scheduled and sequential versus concurrent combination chemotherapy as postoperative adjuvant treatment of node-positive primary breast cancer. J. Clin. Oncol. 21, 1431–1439 (2003).
Chen, Y. M. et al. Serum cytokine level fluctuations in chemotherapy-induced myelosuppression. Jpn J. Clin. Oncol. 26, 18–23 (1996).
Wiik, H., Syrjala, H., Karttunen, R., Bloigu, A. & Haukipuro, K. Neutrophil adhesion molecules in colorectal surgery: effect of filgastrim given postoperatively. Eur. J. Surg. 167, 700–704 (2001).
Bocchietto, E. et al. Proliferative and migratory responses of murine microvascular endothelial cells to G-CSF. J. Cell Physiol. 155, 89–95 (1993).
Liu, F., Poursine-Laurent, J. & Link, D. C. The G-CSF receptor is required for the mobilization of murine haemopoietic progenitors into peripheral blood by cyclophosphamide or interleukin-8. Blood 90, 2522–2528 (1997).
Levesque, J. P. et al. Mobilization by either cyclophosphamide or G-CSF transforms the bone marrow into a highly proteolytic environment. Exp. Hematol. 30, 440–449 (2002).
Hunter, M. G., Druhan, L. J., Massullo, P. R. & Avalos, B. R. Proteolytic cleavage of G-CSF and its receptor by neutrophil elastase induces growth inhibition and decreased cell surface expression of the G-CSF receptor. Am. J. Hematol. 74, 149–155 (2003).
Levesque, J. P., Takamatsu, Y., Nilsson, S. K., Haylock, D. N. & Simmons, P. J. Vascular cell adhesion molecule-1 is cleaved by neutrophil proteases in the bone marrow following haematopoietic progenitor cell mobilization by granulocyte colony-stimulating factor. Blood 98, 1289–1297 (2001).
Gazitt, Y. & Akay, C. Mobilization of myeloma cells involves SDF-1/CXCR4 signalling and downregulation of VLA-4. Stem Cells 22, 65–73 (2004).
Christopherson, K. W., Cooper, S., Hangoc, G. & Broxmeyer, H. E. CD26 is essential for normal G-CSF-induced progenitor cell mobilization as determined by CD26−/− mice. Exp. Hematol. 31, 1126–1134 (2003).
Pethiyagoda, C. L., Welch, D. R. & Fleming, T. P. Dipeptidyl peptidase IV inhibits cellular invasion of melanoma cells. Clin. Exp. Metastasis 18, 391–400 (2000).
Kajiyama, H. et al. Dipeptidyl peptidase IV overexpression induces upregulation of E-cadherin and TIMPs, resulting in decreased invasion in ovarian carcinoma cells. Cancer Res. 63, 2278–2283 (2003).
Eddlestone, J., Christiansen, S. C. & Zuraw, B. L. Functional expression of the CXC chemokine receptor CXCR4 by human bronchial epithelial cells: regulation by proinflammatory mediators. J. Immunol. 169, 6445–6451 (2002).
Helbig, G. et al. NF-κB promotes breast cancer cell migration and metastasis by inducing the expression of the chemokine receptor CXCR4. J. Biol. Chem. 278, 21631–21638 (2003).
Castellone, M. D. et al. Functional expression of the CXCR4 chemokine receptor is induced by RET/PTC oncogenes and is a common event in human papillary thyroid carcinomas. Oncogene 23, 5958–5967 (2004).
Moser, B., Wolf, M., Walz, A. & Loetscher, P. Chemokines: multiple levels of leukocyte migration control. Trends Immunol. 25, 75–84 (2004).
Sadir, R., Imberty, A., Baleux, F. & Lortat-Jacob, H. Heparan sulfate/heparin oligosaccharides protect stromal cell-derived factor-1 (SDF–1/CXCL12) against proteolysis induced by CD26/DPPIV. J. Biol. Chem. (in the press).
Netelenbos, T. et al. Proteoglycans on bone marrow endothelial cells bind and present SDF-1 towards hematopoietic progenitor cells. Leukemia 17, 175–184 (2003).
Gouwy, M., Struyf, S., Catusse, J., Proost, P. & Van Damme, J. Synergy between proinflammatory ligands of G protein-coupled receptors in neutrophil activation and migration. J. Leuk. Biol. 76, 185–194 (2004).
Suratt, B. T. et al. Role of the CXCR4/SDF-1 chemokine axis in circulating neutrophil homeostasis. Blood 104, 565–571 (2004).
Cherla, R. P. & Ganju, R. K. Stromal cell-derived factor 1α-induced chemotaxis in T cells is mediated by nitric oxide signaling pathways. J. Immunol. 66, 3067–3074 (2001).
Shen, W., Bendall, L. J., Gottlieb, D. J. & Bradstock, K. F. The chemokine receptor CXCR4 enhances integrin-mediated in vitro adhesion and facilitates engraftment of leukemic precursor B cells in the bone marrow. Exp. Hematol. 29, 1439–1447 (2001).
Dominguez, F. et al. Hormonal and embryonic regulation of chemokine receptors CXCR1, CXCR4, CCR5 and CCR2B in the human endometrium and the human blastocyst. Mol. Hum. Reprod. 9, 189–198 (2003).
Bartolome, R. A. et al. Stromal cell-derived factor 1α promotes melanoma cell invasion across basement membranes involving stimulation of membrane-type 1 matrix metalloproteinase and Rho GTPase activities. Cancer Res. 64, 2534–2543 (2004).
Mori, T. et al. CXCR4 antagonist inhibits stromal cell-derived factor 1-induced migration and invasion of human pancreatic cancer. Mol. Cancer Ther. 3, 29–37 (2004).
Herrera, C. et al. Comodulation of CXCR4 and CD26 in human lymphocytes. J. Biol. Chem. 276, 19532–19539 (2001).
Wesley, U. V., Tiwari, S. & Houghton, A. N. Role for dipeptidyl peptidase IV in tumor suppression of human non small cell lung carcinoma cells. Int. J. Cancer 109, 855–866 (2004).
Chen, Y., Stamatoyannopoulos, G. & Song, C. Z. Downregulation of CXCR4 by inducible small interfering RNA inhibits breast cancer cell invasion in vitro. Cancer Res. 63 4801–4804 (2003).
Tanabe, S. et al. Expression of mRNA of chemokine receptor CXCR4 in feline mammary adenocarcinoma. Vet. Rec. 151, 729–733 (2002).
Schmid, B. C., Rudas, M., Rezniczek, G. A., Leodolter, S. & Zeillinger, S. CXCR4 is expressed in ductal carcinoma in situ of the breast and in atypical ductal hyperplasia. Breast Cancer Res. Treat. 84, 247–250 (2004).
Christopherson, K. W., Cooper, S. & Broxmeyer, H. E. Cell surface peptidase CD26/DPPIV mediates G-CSF mobilization of mouse progenitor cells. Blood 101, 4680–4686 (2003).
Gazitt, Y. & Liu, Q. Plasma levels of SDF-1 and expression of SDF-1 receptor on CD34+ cells in mobilized peripheral blood of non-Hodgkin's lymphoma patients. Stem Cells 19, 37–45 (2001).
Nagase, H. et al. Cytokine-mediated regulation of CXCR4 expression in human neutrophils. J. Leuk. Biol. 71, 711–717 (2002).
Rutella, S. et al. Homogeneous expression of CXCR4 on G-CSF-mobilized peripheral blood CD34+ cells. Blood 95, 4015–4016 (2000).
Levesque, J. P., Hendy, J., Takamatsu, Y., Simmons, P. J. & Bendall, L. J. Disruption of the CXCR4/CXCL12 chemotactic interaction during hematopoietic stem cell mobilization induced by G-CSF or cyclophosphamide. J. Clin. Invest. 111, 187–196 (2003).
Psenak, O., Sefc, L., Sykora, V., Chang, K. T. & Necas, E. Cytokine gene expression in regenerating haematopoietic tissues of mice after cyclophosphamide treatment. Acta Haematologica 109, 68–75 (2003).
Laver, J. H., Xu, F., Barredo, J. C. & Abboud, M. R. Effects of radiation and 4-hydroperoxycyclophosphamide on production of G- and GM-CSF by stromal cells. Bone Marrow Transplant. 10, 529–533 (1992).
To, L. B. et al. A comparative study of the phenotype and proliferative capacity of peripheral blood CD34+ cells mobilized by four different protocols. Blood 84, 2930–2939 (1994).
Scotton, C. J. et al. Multiple actions of the chemokine CXCL12 on epithelial tumour cells in human ovarian cancer. Cancer Res. 62, 5930–5938 (2002).
Zeelenberg, I. S., Ruuls-Van Stalle, L. & Roos, E. The chemokine receptor CXCR4 is required for outgrowth of colon carcinoma micrometastases. Cancer Res. 63, 3833–3839 (2003).
Fernandis, A. Z., Prasad, A., Band, H., Klosel, R. & Ganju, R. K. Regulation of CXCR4-mediated chemotaxis and chemoinvasion of breast cancer cells. Oncogene 23, 157–167 (2004).
Barbero, S. et al. SDF-1 stimulates human glioblastoma cell growth through the activation of both Erk-1/2 and Akt. Cancer Res. 63, 1969–1974 (2003).
Lee, B. C., Lee, T. H., Avraham, S. & Avraham, H. K. Involvement of the chemokine receptor CXCR4 and its ligand SDF-1 in breast cancer cell migration through human brain microvascular endothelial cells. Mol. Cancer Res. 2, 327–338 (2004).
Kijowski, J. et al. The SDF-1–CXCR4 axis stimulates VEGF secretion and activates integrins but does not affect proliferation and survival in lymphohematopoietic cells. Stem Cells 19, 453–466 (2001).
Scheurer, S. B., Rybak, J. N., Rosli, C., Neri, D. & Elia, G. Modulation of gene expression by hypoxia in human umbilical cord vein endothelial cells: a transcriptomic and proteomic study. Proteomics 4, 1737–1760 (2004).
Hitchon, C. et al. Hypoxia-induced production of SDF-1 (CXCL12) and VEGF by synovial fibroblasts. Arthr. Rheum. 46, 2587–2597 (2002).
Graeber, T. G. et al. Hypoxia-mediated selection of cells with diminished apoptotic potential in solid tumours. Nature 379, 88–91 (1996).
Kanda, S., Mochizuki, Y. & Kanetake, H. SDF-1 induces tube-like structural formation of endothelial cells through phosphatidylinositol 3′-kinase. J. Biol. Chem. 278, 257–262 (2003).
Feil, C. & Augustin, H. G. Endothelial cells differentially express functional CXCR4 under the control of autocrine activity and exogenous cytokines. Biochem. Biophys. Res. Comm. 247, 38–45 (1998).
Bachelder, R. E., Wendt, M. A. & Mercurio, A. M. VEGF promotes breast carcinoma invasion in an autocrine manner by regulating the chemokine receptor CXCR4. Cancer Res. 62, 7203–7206 (2002).
Staller, P. et al. Chemokine receptor CXCR4 downregulated by von Hippel–Lindau tumour suppressor pVHL. Nature 425, 307–311 (2003).
Taichman, R. S. et al. Use of the stromal cell-derived factor-1/CXCR4 pathway in prostate cancer metastasis to bone. Cancer Res. 62, 1832–1837 (2002).
Phillips, R. J. et al. The stromal derived factor-1/SXCR4 biological axis in non-small cell lung cancer metastases. Am. J. Respir. Crit. Care Med. 167, 1676–1686 (2003).
Burger, M. et al. Functional expression of CXCR4 on small-cell lung cancer cells mediates migration, integrin activation, and adhesion to stromal cells. Oncogene 22, 8093–8101 (2003).
Koshiba, T. et al. Expression of stromal cell-derived factor 1 and CXCR4 ligand receptor system in pancreatic cancer: a possible role for tumor progression. Clin. Cancer Res. 6, 3530–3535 (2000).
Libura, J. et al. CXCR4–SDF1 signaling is active in rhabdomyosarcoma cells and regulates locomotion, chemotaxis and adhesion. Blood 100, 2597–2606 (2002).
Muller, A. et al. Involvement of chemokine receptors in breast cancer metastasis. Nature 410, 50–56 (2001).
Kato, M., Kitayama, J., Kazama, S. & Nagawa, H. Expression pattern of CXC chemokine receptor-4 is correlated with lymph node metastasis in human invasive ductal carcinoma. Breast Cancer Res. Treat. 5, R144–R150 (2003).
Oonuma, T. et al. Role of CXCR4 and SDF-1 in mammary tumor metastasis in the cat. J. Vet. Med. Sci. 65, 1069–1073 (2003).
Schmitz, L. L. et al. Morphologic and quantitative changes in blood and marrow following growth factor therapy. Am. J. Clin. Pathol. 101, 67–75 (1994).
Sakamoto, C. et al. Antiapoptotic effect of G-CSF, GM-CSF and cAMP on human neutrophils. Int. J. Hematol. 77, 60–70 (2003).
Ogawa, Y. et al. Sudden termination of G-CSF injection leads to apoptosis of a large proportion of increased granulocytes. Oncol. Rep. 8, 1027–1029 (2001).
Petit, I. et al. G-CSF induces stem cell mobilization by decreasing bone marrow SDF-88 and upregulating CXCR4. Nature Immunol. 3, 687–694 (2002).
Malanski, N. A., Mul, F. P., van Buul, J. D., Roos, D. & Kuijpers, T. W. G-CSF inhibits the mitochondria-dependent activation of caspase-3 in neutrophils. Blood 99, 672–679 (2002).
Boxio, R., Bossenmeyer-Pourie, C., Steinckwich, N., Dournon, C. & Nusse, O. Mouse bone marrow contains large numbers of functionally competent neutrophils. J. Leuk. Biol. 75, 604–611 (2004).
Gaugler, M., Squiban, C., Mouthon, M., Gourmelon, P. & van der Meeren, A. Irradiation enhances the support of haemopoietic cell transmigration, proliferation and differentiation by endothelial cells. Br. J. Haematol. 113, 940–950 (2001).
Ponomaryov, T. et al. Induction of the chemokine SDF-1 following DNA damage improves human stem cell function. J. Clin. Invest. 106, 1331–1339 (2000).
Nagler, A. et al. Low-intensity conditioning is sufficient to ensure engraftment in matched unrelated bone marrow transplantation. Exp. Hematol. 29, 362–370 (2001).
Bornhauser, M. et al. Dose-reduced conditioning for allogeneic blood stem cell transplantation: durable engraftment without antithymocyte globulin. Bone Marrow Transplant. 26, 119–125 (2000).
Miralbell, R. et al. Conditioning the leukemic patient before allogeneic BMT: value of intensifying immunosuppression in the context of different levels of T lymphocyte depletion of the graft. Bone Marrow Transplant. 11, 447–451 (1993).
Tomita, Y., Sachs, D. H. & Sykes M. Myelosuppressive conditioning is required to achieve engraftment of pluripotent stem cells contained in moderate doses of syngeneic bone marrow. Blood 83, 939–948 (1994).
Xu, H. et al. A delay in bone marrow transplantation after partial conditioning improves engraftment. Transplantation 77, 819–826 (2004).
Norton, L. & Simon, R. Tumor size, sensitivity to therapy, and design of treatment schedules. Cancer Treat. Rep. 61, 1307–1317 (1977).
Baumann, I. et al. Mobilisation kinetics of primitive haemopoietic cells following G-CSF with or without chemotherapy in advanced breast cancer. Ann. Oncol. 7, 1051–1057 (1996).
Gazitt, Y. Homing and mobilization of hematopoietic stem cells and hematopoietic cancer cells are mirror image processes, utilizing similar signaling pathways and occurring concurrently. Leukemia 18, 1–10 (2004).
Glimm, H., Tang, P., Clark-Lewis, I., von Kalle, C. & Eaves, C. Ex vivo treatment of proliferating human cord blood stem cells with SDF-1 enhances their ability to engraft NOD/SCID mice. Blood 99, 3454–3457 (2002).
Plett, P. A., Frankovitz, S. M., Wolber, F. M., Abonour, R. & Orschell-Traycoff, C. M. Treatment of circulating CD34+ cells with SDF-1 or anti-CXCR4 antibody enhances migration and NOD/SCID repopulating potential. Exp. Hematol. 30, 1061–1069 (2002).
Broxmeyer, H. E. et al. SDF-1/CXCL12 directly enhances survival/antiapoptosis of myeloid progenitor cells through CXCR4 and G-proteins and enhances engraftment of competitive, repopulating stem cells. J. Leuk. Biol. 73, 630–638 (2003).
Kahn, J. et al. Overexpression of CXCR4 on human CD34+ progenitors increases their proliferation, migration and NOD/SCID repopulation. Blood 103, 2942–2949 (2004).
Christopherson, K. W., Hangoc, G., Mantel, C. R. & Broxmeyer, H. E. Modulation of hematopoietic stem cell homing and engraftment by CD26. Science 305, 1000–1003 (2004).
Pituch-Norowolska, A. et al. Circulating CXCR4-positive stem/progenitor cells compete for SDF-1-positive niches in bone marrow, muscle and neural tissues: an alternative hypothesis to stem cell plasticity. Folia Histochem. Cytobiol. 41, 13–21 (2003).
Cristofanilli, M. et al. Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N. Engl. J. Med. 351, 781–791 (2004).
Cooper, B. W., Moss, T. J., Ross, A. A., Ybanez, J. & Lazarus, H. M. Occult tumor contamination of hematopoietic stem-cell products does not affect clinical outcome of autologous transplantation in patients with metastatic breast cancer. J. Clin. Oncol. 16, 3509–3517 (1998).
Valkovic, T. et al. Correlation between vascular endothelial growth factor, angiogenesis, and tumor-associated macrophages in invasive ductal breast carcinomas. Virchows Arch. 440, 583–588 (2002).
Liu, C. Y. et al. Apoptotic neutrophils undergoing secondary necrosis induce human lung epithelial cell detachment. J. Biomed. Sci. 10, 746–756 (2003).
Hall, J. M. & Korach, K. S. Stromal cell derived factor 1, a novel target of estrogen receptor action, mediates the mitogenic effects of estradiol in ovarian and breast cancer cells. J. Mol. Endocrinol. 17, 792–803 (2003).
Coser, K. R., Chesnes, J., Hur, J., Isselbacher, K. J. & Shioda, T. Global analysis of ligand sensitivity of estrogen-inducible and -suppressible genes in MCF7/BUS breast cancer cells by DNA microarray. Proc. Natl Acad. Sci. USA 100, 13994–13999 (2003).
Hess, K. R., Pusztai, L., Buzdar, A. U. & Hortobagyi, G. N. Estrogen receptors and distinct patterns of breast cancer relapse. Breast Cancer Res. Treat. 78, 105–118 (2003).
Colleoni, M. et al. Identifying breast cancer patients at high risk for bone metastases. J. Clin. Oncol. 18, 3925–3935 (2000).
Morgan, L. R. et al. Therapeutic use of tamoxifen in advanced breast cancer: correlation with biochemical parameters. Cancer Treat. Rep. 60, 1437–1443 (1976).
Buzzoni, R. et al. Combination goserelin and tamoxifen therapy in premenopausal advanced breast cancer. Br. J. Cancer 71, 1111–1114 (1995).
Valagussa, P. et al. Adjuvant CMF effect on site of first recurrence in operable breast cancer with positive axillary nodes. Breast Cancer Res. Treat. 1, 349–356 (1981).
Kaufmann, M. et al. Goserelin, a depot GnRH agonist in the treatment of premenopausal patients with metastatic breast cancer. J. Clin. Oncol. 7, 1113–1119 (1989).
Moseson, D. L. et al. The use of antiestrogens tamoxifen and nafoxidine in the treatment of human breast cancer in correlation with estrogen receptor values. Cancer 41, 797–802 (1978).
Klijn, J. G., de Jong, F. H., Lamberts, S. W. & Blankenstein, M. A. LHRH-agonist treatment in clinical and experimental human breast cancer. J. Steroid Biochem. 23, 867–873 (1985).
Coradini, D. et al. Relationship between steroid receptors as continuous variables and response to adjuvant treatments in postmenopausal women with node-positive breast cancer. Int. J. Biol. Markers 14, 60–67 (1999).
Sainsbury, R. Aromatase inhibition in the treatment of advanced breast cancer: is there a relationship between potency and clinical efficacy? Br. J. Cancer 90, 1733–1739 (2004).
Ellis, M. J., Rosen, E., Dressman, H. & Marks, J. Neoadjuvant comparisons of aromatase inhibitors and tamoxifen: pretreatment determinants of response and on-treatment effect. J. Steroid Biochem. Mol. Biol. 86, 301–307 (2003).
Dowsett, M. et al. HER-2 amplification impedes the antiproliferative effects of hormone therapy in estrogen receptor-positive primary breast cancer. Cancer Res. 61, 8452–8458 (2001).
Shou, J. et al. Mechanisms of tamoxifen resistance: increased estrogen receptor-HER2/neu crosstalk in ER/HER2-positive breast cancer. J. Natl Cancer Inst. 96, 926–935 (2004).
Love, R. R. et al. Her-2/neu overexpression and response to oophorectomy plus tamoxifen adjuvant therapy in estrogen receptor-positive premenopausal women with operable breast cancer. J. Clin. Oncol. 21, 453–457 (2003).
Santen, R. J. et al. Estrogen production via the aromatase enzyme in breast carcinoma: which cell type is responsible? J. Steroid Biochem. Mol. Biol. 61, 267–271 (1997).
Smithers, D. W. An attack on cytologism. Lancet 1, 493–499 (1962).
Watson, J. V. What does “response” in cancer chemotherapy really mean? Br. Med. J. 283, 34–37 (1981).
Onuffer, J. J. & Horuk, R. Chemokines, chemokine receptors and small-molecule antagonists: recent developments. Trends Pharmacol. Sci. 23, 459–467 (2002).
Hatse, S., Princen, K., Bridger, G., De Clercq, E. & Schols, D. Chemokine receptor inhibition by AMD3100 is strictly confined to CXCR4. FEBS Lett. 527, 255–262 (2002).
Zhang, L., Kharbanda, S., Hanfelt, J. & Kern, F. G. Both autocrine and paracrine effects of transfected acidic fibroblast growth factor are involved in the estrogen-independent and antiestrogen-resistant growth of MCF-7 breast cancer cells. Cancer Res. 58, 352–361 (1998).
Bogdanos, J. et al. Endocrine/paracrine/autocrine survival factor activity of bone microenvironment participates in the development of androgen ablation and chemotherapy refractoriness of prostate cancer metastasis in skeleton. Endocr. Rel. Cancer 10, 279–289 (2003).
Kouniavsky, G. et al. Stromal extracellular matrix reduces chemotherapy-induced apoptosis in colon cancer cell lines. Clin. Exp. Metastasis 19, 55–60 (2002).
Fortney, J. E., Zhao, W., Wenger, S. L. & Gibson L. F. Bone marrow stromal cells regulate caspase 3 activity in leukemic cells during chemotherapy. Leuk. Res. 25, 901–907 (2001).
Pietras, K. et al. Inhibition of PDGF receptor signaling in tumor stroma enhances antitumor effect of chemotherapy. Cancer Res. 62, 5476–5484 (2002).
Zondor, S. D. & Medina, P. J. Bevacizumab: an angiogenesis inhibitor with efficacy in colorectal and other malignancies. Ann. Pharmacother. 38, 1258–1264 (2004).
Liang, Z. et al. Inhibition of breast cancer metastasis by selective synthetic peptides against CXCR4. Cancer Res. 64, 4302–4308 (2004).
Tamamura, H. et al. T140 analogs as CXCR4 antagonists identified as antimetastatic agents in the treatment of breast cancer. FEBS Lett. 550, 79–83 (2003).
Mihara, M. et al. p53 has a direct apoptogenic role at the mitochondria. Mol. Cell 11, 577–590 (2003).
Erster, S., Mihara, M., Kim, R. H., Petrenko, O. & Mol, U. M. In vivo mitochondrial p53 translocation triggers a rapid first wave of cell death in response to DNA damage that can precede p53 target gene activation. Mol. Cell. Biol. 24, 6728–6741 (2004).
Acknowledgements
Thanks are due to B.S. Mann of the Center for Drug Evaluation and Research, FDA, Rockville, Maryland, USA, and to J.C. Chim from the Division of Haematology/Oncology, Queen Mary Hospital, Hong Kong, for constructive comments on the manuscript.
Author information
Authors and Affiliations
Ethics declarations
Competing interests
The author declares no competing financial interests.
Related links
Related links
DATABASES
Entrez Gene
National Cancer Institute
Rights and permissions
About this article
Cite this article
Epstein, R. The CXCL12–CXCR4 chemotactic pathway as a target of adjuvant breast cancer therapies. Nat Rev Cancer 4, 901–909 (2004). https://doi.org/10.1038/nrc1473
Issue Date:
DOI: https://doi.org/10.1038/nrc1473
This article is cited by
-
Platelet-derived microparticles stimulate the invasiveness of colorectal cancer cells via the p38MAPK-MMP-2/MMP-9 axis
Cell Communication and Signaling (2023)
-
EIF3D promotes gallbladder cancer development by stabilizing GRK2 kinase and activating PI3K-AKT signaling pathway
Cell Death & Disease (2017)
-
Enriching Traditional Protein-protein Interaction Networks with Alternative Conformations of Proteins
Scientific Reports (2017)
-
Biological/pathological functions of the CXCL12/CXCR4/CXCR7 axes in the pathogenesis of bladder cancer
International Journal of Clinical Oncology (2017)
-
Balancing efficacy of and host immune responses to cancer therapy: the yin and yang effects
Nature Reviews Clinical Oncology (2016)