Abstract
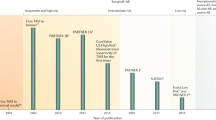
The first human transcatheter aortic valve implantation (TAVI) in 2002, and several subsequent single-center series, showed the feasibility of this new approach for the treatment of patients with severe aortic stenosis who were considered to be at very high or prohibitive surgical risk. More-recent multicenter registries have confirmed the safety and efficacy of this procedure, despite a very-high-risk patient profile. Moreover, the randomized, controlled PARTNER trial has confirmed both the superiority of TAVI over medical treatment in patients not considered to be candidates for standard surgical aortic valve replacement and the noninferiority of TAVI compared with surgical aortic valve replacement in high-risk patients. The hemodynamics of transcatheter valves are usually excellent, although residual paravalvular aortic regurgitation (usually trivial or mild) is frequent. Stroke, major vascular complications, and conduction disturbances leading to permanent pacemaker implantation remain among the most-concerning periprocedural complications of TAVI. Nevertheless, promising preliminary data exist for long-term outcomes following TAVI, 'valve-in-valve' TAVI for surgical prosthesis dysfunction, and for the treatment of lower-risk patients. Improvements in transcatheter valve technology, optimization of procedural and midterm results, and confirmation of long-term durability of transcatheter valve prostheses will determine the expansion of TAVI towards the treatment of a broader spectrum of patients.
Key Points
-
Transcatheter aortic valve implantation (TAVI) represents a less-invasive strategy than surgical aortic valve replacement (SAVR) for the treatment of severe symptomatic aortic stenosis
-
The transfemoral approach is usually the first option for TAVI; transapical, subclavian, axillary, and transaortic routes are alternative approaches
-
TAVI is currently the treatment of choice for patients not considered to be candidates for SAVR, and a proven alternative for those considered to be at high surgical risk
-
Transcatheter valves are associated with excellent hemodynamic results, usually with concomitant improvements in the patient's functional status and quality of life; however, minor residual aortic regurgitation occurs in many patients
-
Periprocedural stroke, vascular and conduction disturbance complications, occurrence of moderate or severe paravalvular aortic regurgitation, relatively high midterm mortality, and valve durability beyond 3-year follow-up are unresolved issues in TAVI
-
The 'valve-in-valve' treatment of surgical prosthesis dysfunction and the treatment of intermediate-risk patients are two of the most-important fields for the development of TAVI in the near future
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Andersen, H. R. et al. Transluminal implantation of artificial heart valves. Description of a new expandable aortic valve and initial results with implantation by catheter technique in closed chest pigs. Eur. Heart J. 13, 704–708 (1992).
Lutter, G., Ardehali, R., Cremer, J. & Bonhoeffer, P. Percutaneous valve replacement: current state and future prospects. Ann. Thorac. Surg. 78, 2199–2206 (2004).
Cribier, A. et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis. First human case description. Circulation 106, 3006–3008 (2002).
Cribier, A. et al. Early experience with percutaneous transcatheter implantation of heart valve prosthesis for the treatment of end-stage inoperable patients with calcific aortic stenosis. J. Am. Coll. Cardiol. 43, 698–703 (2004).
Webb, J. G. et al. Percutaneous aortic valve implantation retrograde from the femoral artery. Circulation 113, 842–850 (2006).
Webb, J. G. et al. Percutaneous transarterial aortic valve replacement in selected high-risk patients with aortic stenosis. Circulation 116, 755–763 (2007).
Lichtenstein, S. V. et al. Transapical transcatheter aortic valve implantation in humans. Initial clinical experience. Circulation 114, 591–596 (2006).
Walther, T. et al. Minimally invasive transapical beating heart aortic valve implantation—proof of concept. Eur. J. Cardiothorac. Surg. 31, 9–15 (2007).
Walther, T. et al. Transapical minimally invasive aortic valve implantation. Multicenter experience. Circulation 116 (11 Suppl.), I240–I245 (2007).
Svensson, L. G. et al. United States feasibility study of transcatheter insertion of a stented aortic valve by the left ventricular apex. Ann. Thorac. Surg. 86, 46–55 (2008).
Walther, T. et al. One-year interim follow-up results of the TRAVERCE trial: the initial feasibility study for trans-apical aortic valve implantation. Eur. J. Cardiothorac. Surg. 39, 532–527 (2011).
Rodés-Cabau, J. et al. Feasibility and initial results of percutaneous aortic valve implantation including selection of the transfemoral or transapical approach in patients with severe aortic stenosis. Am. J. Cardiol. 102, 1240–1246 (2008).
Lefèvre, T. et al. One year follow-up of the multi-centre European PARTNER transcatheter heart valve study. Eur. Heart J. 32, 148–157 (2011).
Kodali, S. K. et al. Early and late (one year) outcomes following transcatheter aortic valve implantation in patients with severe aortic stenosis (from the United States REVIVAL trial). Am. J. Cardiol. 107, 1058–1064 (2011).
Grube, E. et al. First report on a human percutaneous transluminal implantation of a self-expanding valve prosthesis for interventional treatment of aortic valve stenosis. Catheter. Cardiovasc. Interv. 66, 465–469 (2005).
Grube, E. et al. Percutaneous implantation of the CoreValve self-expanding valve prosthesis in high-risk patients with aortic valve disease. The Siegburg first-in-human study. Circulation 114, 1616–1624 (2006).
Marcheix, B. et al. Surgical aspects of endovascular retrograde implantation of the aortic CoreValve bioprothesis in high-risk older patients with severe symptomatic aortic stenosis. J. Thorac. Cardiovasc. Surg. 134, 1150–1156 (2007).
Grube, E. et al. Percutaneous aortic valve replacement for severe aortic stenosis in high-risk patients using the second- and current third-generation self-expanding corevalve prosthesis. J. Am. Coll. Cardiol. 50, 69–76 (2007).
Rodés-Cabau, J. et al. Transcatheter aortic valve implantation for the treatment of severe symptomatic aortic stenosis in patients at very high or prohibitive surgical risk. Acute and late outcomes of the multicenter Canadian experience. J. Am. Coll. Cardiol. 55, 1080–1090 (2010).
Thomas, M. et al. Thirty-day results of the SAPIEN aortic bioprosthesis European outcome (SOURCE) registry: a European registry of transcatheter aortic valve implantation using the Edwards SAPIEN valve. Circulation 122, 62–69 (2010).
Piazza, N. et al. Procedural and 30-day outcomes following transcatheter aortic valve implantation using the third generation (18F) CoreValve revalving system: results from the multicentre, expanded evaluation registry 1-year following CE mark approval. EuroIntervention 4, 242–249 (2008).
Tamburino, C. et al. Incidence and predictors of early and late mortality after transcatheter aortic valve implantation in 663 patients with severe aortic stenosis. Circulation 123, 299–308 (2011).
Eltchaninoff, H. et al. Transcatheter aortic valve implantation: early results of the FRANCE (FRench Aortic National CoreValve and Edwards) registry. Eur. Heart J. 32, 191–197 (2011).
Zahn, R. et al. Transcatheter aortic valve implantation: first results from a multi-centre real-world registry. Eur. Heart J. 32, 198–204 (2011).
Bosmans, J. M. et al. Procedural, 30-day and one year outcome following CoreValve or Edwards transcatheter aortic valve implantation: results of the Belgian national registry. Interact. Cardiovasc. Thorac. Surg. 12, 762–767 (2011).
Moat, N. et al. Long-term outcomes after transcatheter aortic valve implantation in high-risk patients with severe aortic stenosis. The UK TAVI (United Kingdom Transcatheter Aortic Valve Implantation) registry. J. Am. Coll. Cardiol. 58, 2130–2138 (2011).
Leon, M. B. et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N. Engl. J. Med. 363, 1597–607 (2010).
Smith, C. R. et al. Transcatheter versus Surgical Aortic-Valve Replacement in High-Risk Patients. N. Engl. J. Med. 364, 2187–2198 (2011).
Ng, A. C. et al. Comparison of aortic root dimensions and geometries before and after transcatheter aortic valve implantation by 2- and 3-dimensional transesophageal echocardiography and multislice computed tomography. Circ. Cardiovasc. Imaging 3, 94–102 (2010).
Messika-Zeitoun, D. et al. Multimodal assessment of the aortic annulus diameter. Implications for transcatheter aortic valve implantation. J. Am. Coll. Cardiol. 55, 186–194 (2010).
Koos, R. et al. Evaluation of aortic root for definition of prosthesis size by magnetic resonance imaging and cardiac computed tomography: Implications for transcatheter aortic valve implantation. Int. J. Cardiol. 13 (Suppl. 1), P243 (2011).
Tzikas, A. et al. Assessment of the aortic annulus by multislice computed tomography, contrast aortography, and trans-thoracic echocardiography in patients referred for transcatheter aortic valve implantation. Catheter. Cardiovasc. Interv. 77, 868–875 (2011).
Schultz, C. J. et al. Three dimensional evaluation of the aortic annulus using multislice computer tomography: are manufacturer's guidelines for sizing for percutaneous aortic valve replacement helpful? Eur. Heart J. 31, 849–856 (2010).
Lange, R. et al. First successful transapical aortic valve implantation with the Corevalve Revalving system: a case report. Heart Surg. Forum 10, e478–e479 (2007).
Bagur, R. et al. Usefulness of TEE as the primary imaging technique to guide transcatheter transapical aortic valve implantation. JACC Cardiovasc. Imaging 4, 115–124 (2011).
Rodés-Cabau, J. et al. Incidence, predictive factors, and prognostic value of myocardial injury following uncomplicated transcatheter aortic valve implantation. J. Am. Coll. Cardiol. 57, 1988–1999 (2011).
Bauernschmitt, R. et al. Transcatheter aortic valve implantation through the ascending aorta: an alternative option for no-access patients. Heart Surg. Forum 12, E63–E64 (2009).
Latsios, G., Gerckens, U. & Grube, E. Transaortic transcatheter aortic valve implantation: a novel approach for the truly “no-access option” patients. Catheter. Cardiovasc. Interv. 75, 1129–1136 (2010).
Bapat, V., Thomas, M., Hancock, J. & Wilson, K. First successful trans-catheter aortic valve implantation through ascending aorta using Edwards SAPIEN THV system. Eur. J. Cardiothorac. Surg. 38, 811–813 (2010).
Ruge, H. et al. First successful aortic valve implantation with the CoreValve ReValving system via right subclavian artery access: a case report. Heart Surg. Forum 11, 323–324 (2008).
Petronio, A. S. et al. Safety and efficacy of the subclavian approach for transcatheter aortic valve implantation with the CoreValve revalving system. Circ. Cardiovasc. Interv. 3, 359–366 (2010).
De Robertis, F. et al. The left axillary artery—a new approach for transcatheter aortic valve implantation. Eur. J. Cardiothorac. Surg. 36, 807–812 (2009).
Grube, E. et al. Feasibility of transcatheter aortic valve implantation without pre-dilation: a pilot study. JACC Cardiovasc. Intervent. 4, 751–757 (2011).
Gurvitch, R. et al. Transcatheter aortic valve implantation. Durability of clinical and hemodynamic outcomes beyond 3 years in a large patient cohort. Circulation 122, 1319–1327 (2010).
Buellesfeld, L. et al. 2-year follow-up of patients undergoing transcatheter aortic valve implantation using a self-expandable valve prosthesis. J. Am. Coll. Cardiol. 57, 1650–1657 (2011).
Nuis, R. J. et al. Frequency, determinants, and prognostic effects of acute kidney injury and red blood cell transfusion in patients undergoing transcatheter aortic valve implantation. Catheter. Cardiovasc. Interv. 77, 881–9 (2011).
Sinning, J. M. et al. Renal function as predictor of mortality in patients after percutaneous transcatheter aortic valve implantation. JACC Cardiovasc. Interv. 3, 1141–1149 (2010).
Thomas, M. et al. One-year outcomes of cohort 1 in the Edwards SAPIEN Aortic Bioprosthesis European Outcome (SOURCE) registry: the European registry of transcatheter aortic valve implantation using the Edwards SAPIEN valve. Circulation 124, 425–433 (2011).
Wenaweser, P. et al. Clinical outcome and predictors for adverse events after transcatheter aortic valve implantation with the use of different devices and routes. Am. Heart J. 161, 1114–1124 (2011).
Dewey, T. M. et al. Effect of concomitant coronary artery disease on procedural and late outcomes of transcatheter aortic valve implantation. Ann. Thorac. Surg. 89, 758–767 (2010).
Abdel-Wahab, M. et al. Aortic regurgitation after transcatheter aortic valve implantation: incidence and early outcome. Results from the German transcatheter aortic valve interventions registry. Heart 97, 899–906 (2011).
Webb, J. G. et al. Transcatheter aortic valve implantation. Impact on clinical and valve-related outcomes. Circulation 119, 3009–3016 (2009).
Bagur, R. et al. Acute kidney injury following transcatheter aortic valve implantation: predictive factors, prognostic value, and comparison with surgical aortic valve replacement. Eur. Heart J. 31, 865–874 (2010).
Ranucci, M. et al. Surgical and transcatheter aortic valve procedures. The limits of risk scores. Interact. Cardiovasc. Thorac. Surg. 11, 138–141 (2010).
Dewey, T. M. et al. Reliability of risk algorithms in predicting early and late operative outcomes in high-risk patients undergoing aortic valve replacement. J. Thorac. Cardiovasc. Surg. 135, 180–187 (2008).
Rosenhek, R. et al. ESC working group on valvular heart disease position paper: assessing the risk of interventions in patients with valvular heart disease. Eur. Heart J. http://dx.doi.org/10.1093/eurheartj/ehr061 (2011).
Himbert, D. et al. Results of transfemoral or transapical aortic valve implantation following a uniform assessment in high-risk patients with aortic stenosis. J. Am. Coll. Cardiol. 54, 303–311 (2009).
Grube, E. et al. Progress and current status of percutaneous aortic valve replacement results of three device generations of the CoreValve Revalving system. Circ. Cardiovasc. Intervent. 1, 167–175 (2008).
Gurvitch, R. et al. Transcatheter aortic valve implantation: lessons from the learning curve of the first 270 high-risk patients. Catheter. Cardiovasc. Interv. http://dx.doi.org/10.1002/ccd.22961 (2011).
Leon, M. B. et al. Standardized endpoint definitions for transcatheter aortic valve implantation clinical trials: A consensus report from the Valve Academic Research Consortium. J. Am. Coll. Cardiol. 57, 253–269 (2011).
Hayashida, K. et al. Transfemoral aortic valve implantation new criteria to predict vascular complications. JACC Cardiovasc. Interv. 4, 851–858 (2011).
Saia, F. et al. Incidence, prognostic value and management of vascular complications with transfemoral transcatheter aortic valve implantation. Future Cardiol. 7, 321–331 (2011).
Cockburn, J. et al. Large caliber arterial access device closure for percutaneous aortic valve interventions: use of the Prostar system in 118 cases. Catheter. Cardiovasc. Interv. http://dx.doi.org/10.1002/ccd.23105 (2011).
Van Mieghem, N. M. et al. Vascular complications with transcatheter aortic valve implantation using the 18 Fr Medtronic CoreValve system: the Rotterdam experience. Eurointervention 5, 673–679 (2010).
Sharp, A. S. et al. A new technique for vascular access management in transcatheter aortic valve implantation. Catheter. Cardiovasc. Interv. 75, 784–793 (2010).
Genereux, P. et al. Clinical outcomes using a new crossover balloon occlusion technique for percutaneous closure after transfemoral aortic valve implantation. JACC Cardiovasc. Interv. 4, 861–867 (2011).
Kahlert, P. et al. Silent and apparent cerebral ischemia after percutaneous transfemoral aortic valve implantation: a diffusion-weighted magnetic resonance imaging study. Circulation 121, 870–878 (2010).
Ghanem, A. et al. Risk and fate of cerebral embolism after transfemoral aortic valve implantation. A prospective pilot study with diffusion-weighted magnetic resonance imaging. J. Am. Coll. Cardiol. 55, 1427–1432 (2010).
Rodés-Cabau, J. et al. Cerebral embolism following transcatheter aortic valve implantation: comparison of transfemoral and transapical approaches. J. Am. Coll. Cardiol. 57, 18–28 (2011).
Kahlert, P. et al. Cerebral embolization during transcatheter aortic valve implantation (TAVI): a transcranial Doppler study [abstract]. Circulation 122, A18122 (2010).
Szeto, W. Y. et al. Cerebral embolic exposure during transfemoral and transapical transcatheter aortic valve replacement. J. Card. Surg. 26, 348–354 (2011).
Nietlispach, F. et al. An embolic deflection device for aortic valve interventions. JACC Cardiovasc. Interv. 3, 1133–1138 (2010).
Miller, C. et al. Transcatheter (TAVR) versus surgical (AVR) aortic valve replacement: incidence, hazard, determinants, and consequences of neurological events in the PARTNER Trial. Presented at the 2011 Annual meeting of the American Association of Thoracic Surgeons.
Kapadia, S. R., Svensson, L. & Tuzcu, M. Successful percutaneous management of left main trunk occlusion during percutaneous aortic valve replacement. Catheter. Cardiovasc. Interv. 73, 966–972 (2009).
Bagur, R. et al. Coronary ostia stenosis following transcatheter aortic valve implantation. JACC Cardiovasc. Interv. 3, 253–255 (2010).
Stabile, E. et al. Acute left main obstructions following TAVI. EuroIntervention 6, 100–105 (2010).
Crimi, G., Passerone, G. & Rubartelli, P. Trans-apical aortic valve implantation complicated by left main occlusion. Catheter. Cardiovasc. Interv. 78, 656–659 (2011).
Saia, F., Marrozzini, C. & Marzocchi, A. Displacement of calcium nodules from the native valve as a possible cause of left main occlusion following transcatheter aortic valve implantation. J. Invasive Cardiol. 23, E106–E109 (2011).
Gogas, B. D., Zacharoulis, A. A. & Antoniadis, A. G. Acute coronary occlusion following TAVI. Catheter. Cardiovasc. Interv. 77, 435–438 (2011).
Aregger, F. et al. Risk of acute kidney injury in patients with severe aortic valve stenosis undergoing transcatheter valve replacement. Nephrol. Dial. Transplant. 24, 2175–2179 (2009).
Elhmidi, Y. et al. Incidence and predictors of acute kidney injury in patients undergoing transcatheter aortic valve implantation. Am. Heart J. 161, 735–739 (2011).
Van Linden, A. et al. Risk of acute kidney injury after minimally invasive transapical aortic valve implantation in 270 patients. Eur. J. Cardiothorac. Surg. 39, 835–843 (2011).
Sinhal, A. et al. Atrioventricular block after transcatheter balloon expandable aortic valve implantation. JACC Cardiovasc. Interv. 1, 305–309 (2008).
Gutiérrez, M. et al. Electrocardiographic changes and clinical outcomes after transapical aortic valve implantation. Am. Heart J. 158, 302–308 (2009).
Godin, M. et al. Frequency of conduction disturbances after transcatheter implantation of an Edwards Sapien aortic valve prosthesis. Am. J. Cardiol. 106, 707–712 (2010).
Piazza, N. et al. Early and persistent intraventricular conduction abnormalities and requirements for pacemaking after percutaneous replacement of the aortic valve. JACC Cardiovasc. Interv. 1, 310–316 (2008).
Jilaihawi, H. et al. Predictors for permanent pacemaker requirement after transcatheter aortic valve implantation with the CoreValve bioprosthesis. Am. Heart J. 157, 860–866 (2009).
Erkapic, D. et al. Electrocardiographic and further predictors for permanent pacemaker requirement after transcatheter aortic valve implantation. Europace 12, 1188–1190 (2010).
Nuis, R. J. et al. Timing and potential mechanisms of new conduction abnormalities during the implantation of the Medtronic CoreValve system in patients with aortic stenosis. Eur. Heart J. 32, 2067–2074 (2011).
Baan, J. et al. Factors associated with cardiac conduction disorders and permanent pacemaker implantation after percutaneous aortic valve implantation with the CoreValve prosthesis. Am. Heart J. 159, 497–503 (2010).
Fraccaro, C. et al. Incidence, predictors, and outcome of conduction disorders after transcatheter self-expandable aortic valve implantation. Am. J. Cardiol. 107, 747–754 (2011).
Khawaja, M. Z. et al. Permanent pacemaker insertion after CoreValve transcatheter aortic valve implantation: incidence and contributing factors (the UK CoreValve collaborative). Circulation 123, 951–960 (2011).
Haworth, P. et al. Predictors for permanent pacing after transcatheter aortic valve implantation. Catheter. Cardiovasc. Interv. 76, 751–756 (2010).
Roten, L. et al. Incidence and predictors of atrioventricular conduction impairment after transcatheter aortic valve implantation. Am. J. Cardiol. 106, 1473–1480 (2010).
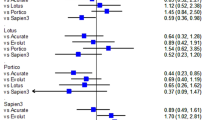
Clavel, M. A. et al. Comparison of the hemodynamic performance of percutaneous and surgical bioprostheses for the treatment of severe aortic stenosis. J. Am. Coll. Cardiol. 53, 1883–1891 (2009).
Zegdi, R. et al. Is it reasonable to treat all calcified stenotic aortic valves with a valved stent? Results from a human anatomic study in adults. J. Am. Coll. Cardiol. 51, 579–584 (2009).
Schultz, C. J. et al. Geometry and degree of apposition of the CoreValve Revalving system with multislice computed tomography after implantation in patients with aortic stenosis. J. Am. Coll. Cardiol. 54, 911–918 (2009).
Clavel, M. A. et al. Validation and characterization of transcatheter aortic valve effective orifice area measured by Doppler-echocardiography. JACC Cardiovasc. Imaging 4, 1053–1062 (2011).
Kalavrouziotis, D. et al. Transcatheter aortic valve implantation in patients with severe aortic stenosis and small aortic annulus. J. Am. Coll. Cardiol. 58, 1016–1024 (2011).
Bauer, F. et al. Acute improvement in global and regional left ventricular systolic function after percutaneous heart valve implantation in patients with symptomatic aortic stenosis. Circulation 110, 1473–1476 (2004).
Clavel, M. A. et al. Comparison between transcatheter and surgical prosthetic valve implantation in patients with severe aortic stenosis and reduced left ventricular ejection fraction. Circulation 122, 1928–1936 (2010).
Rodés-Cabau, J., Dumont, E. & Doyle, D. “Valve-in-valve” for the treatment of paravalvular leaks following transcatheter aortic valve implantation. Catheter. Cardiovasc. Interv. 74, 1116–1119 (2009).
Ussia, G. P. et al. The valve-in-valve technique for treatment of aortic bioprosthesis malposition: an analysis of incidence and 1-year clinical outcomes from the Italian CoreValve registry. J. Am. Coll. Cardiol 57, 1062–1068 (2011).
Latib, A. et al. Post-implantation repositioning of the CoreValve percutaneous valve. JACC Cardiovasc. Interv. 3, 119–121 (2010).
John, D. et al. Correlation of device landing zone calcification and acute procedural success in patients undergoing transcatheter aortic valve implantations with the self-expanding CoreValve prosthesis. JACC Cardiovasc. Interv. 3, 233–243 (2010).
Détaint, D. et al. Determinants of significant paravalvular regurgitation after transcatheter aortic valve implantation : impact of device and annulus discongruence. JACC Cardiovasc. Interv. 2, 821–827 (2009).
Sherif, M. A. et al. Anatomic and procedural predictors of paravalvular aortic regurgitation after implantation of the Medtronic CoreValve bioprosthesis. J. Am. Coll. Cardiol. 56, 1623–1629 (2010).
Gotzmann, M. et al. Short-term effects of transcatheter aortic valve implantation on neurohormonal activation, quality of life and 6-minute walk test in severe and symptomatic aortic stenosis. Heart 96, 1102–1106 (2010).
Bagur, R. et al. Exercise capacity in patients with severe symptomatic aortic stenosis before and six months after transcatheter aortic valve implantation. Am. J. Cardiol. 108, 258–264 (2011).
Ussia, G. P. et al. Quality of life assessment after percutaneous aortic valve implantation. Eur. Heart J. 30, 1790–1796 (2009).
Krane, M. et al. Quality of life among patients undergoing transcatheter aortic valve implantation. Am. Heart J. 160, 451–457 (2010).
Bagur, R. et al. Performance-based functional assessment of patients undergoing transcatheter aortic valve implantation. Am. Heart J. 161, 726–734 (2011).
Bekeredijian, R. et al. Usefulness of percutaneous aortic valve implantation to improve quality of life in patients >80 years of age. Am. J. Cardiol. 106, 1777–1781 (2010).
Gonçalves, A. et al. Quality of life improvement at midterm follow-up after transcatheter aortic valve implantation. Int. J. Cardiol. http://dx.doi.org/10.1016/j.ijcard.2011.05.050 (2011).
Gotzmann, M. et al. One-year results of transcatheter aortic valve implantation in severe symptomatic aortic valve stenosis. Am. J. Cardiol. 107, 1687–1692 (2011).
Reynolds, M. R. et al. Health related quality of life after transcatheter aortic valve replacement in inoperable patients with severe aortic stenosis. Circulation 124, 1964–1972 (2011).
Gotzmann, M. et al. Transcatheter aortic valve implantation in patients with severe symptomatic aortic valve stenosis-predictors of mortality and poor treatment response. Am. Heart J. 162, 238–245 (2011).
Tamburino, C. et al. Early and mid term outcomes of transcatheter aortic valve implantation in patients with logistic euroscore less than 20%: a comparative analysis between different risk strata. Catheter. Cardiovasc. Interv. http://dx.doi.org/10.1002/ccd.23100 (2011).
Leon M. TAVR in lower risk patients: PARTNER II update. Presented at the 2011 Transcatheter Valve Therapeutics meeting.
Taylor, J. The time has come for a SYNTAX-like trial for transcatheter aortic valve implantation. Eur. Heart J. 32, 128–129 (2011).
US National Library of Medicine. ClinicalTrials.gov Transcatheter Compared to Surgical Valve Implantation in Patients With Severe Aortic Valve Stenosis (TAVIvsSAVR) [online], (2011).
Webb, J. G. et al. Transcatheter valve-in-valve implantation for failed bioprosthetic heart valves. Circulation 27, 1848–1857 (2010).
Pasic, M. et al. Transapical aortic valve implantation after previous aortic valve replacement. Clinical proof of the “valve-in-valve” concept. J. Thorac. Cardiovasc. Surg. 142, 270–277 (2011).
Gotzmann, M., Mügge, A. & Bojara, W. Transcatheter aortic valve implantation for treatment of patients with degenerated aortic bioprosstheses-valve-in-valve technique. Catheter. Cardiovasc. Interv. 76, 1000–1006 (2010).
Kempfert, J. et al. Transapical off-pump valve-in-valve implantation in patients with degenerated aortic xenografts. Ann. Thorac. Surg. 89, 1934–1941 (2010).
Schofer, J. et al. Aortic stenosis: a first-in-man retrograde transarterial implantation of a non-metallic aortic valve prosthesis. Circ. Cardiovasc. Interv. 1, 126–133 (2008).
Treede, H. et al. Six-months results of a repositionable and retrievable epicardial valve for transcatheter aortic valve replacement: the Direct Flow Medical aortic valve. J. Thorac. Cardiovasc. Surg. 140, 897–903 (2010).
Gaia, D. F. et al. Off-pump transapical balloon-expandable aortic valve endoprosthesis implantation. Rev. Bras. Cir. Cardiovasc. 24, 233–238 (2009).
Gaia, D. F. et al. Transapical aortic valve implantation: results of a Brazilian prosthesis. Rev. Bras. Cir. Cardiovasc. 25, 293–302 (2010).
Kempfert, J., Rastan, A. J., Mohr, F. W., and Walther, T. A new self-expanding transcatheter aortic valve for transapical implantation—first in man implantation of the JenaValve. Eur. J. Cardiothorac. Surg. 40, 761–763 (2011).
Buellesfeld, L., Gerckens, U. and Grube, E. Percutaneous implantation of the first repositionable aortic valve prosthesis in a patient with severe aortic stenosis. Catheter. Cardiovasc. Interv. 71, 579–584 (2008).
Kempfert, J. et al. Transapical aortic valve implantation using a new self-expandable bioprosthesis: initial outcomes. Eur. J. Cardiothorac. Surg. 40, 1114–1119 (2011).
Falk, V. et al. New anatomically oriented transapical aortic valve implantation. Ann. Thorac. Surg. 87, 925–926 (2009).
Falk, V. et al. Transapical aortic valve implantation with a self-expanding anatomically oriented valve. Eur. Heart J. 32, 878–887 (2011).
Acknowledgements
The author wishes to thank Mélanie Côté, MSc, (Quebec Heart and Lung Institute, Quebec City, QC, Canada) for her outstanding work in the preparation of tables and figures.
Author information
Authors and Affiliations
Ethics declarations
Competing interests
J. Rodés-Cabau declares that he is a consultant for Edwards Lifesciences and St. Jude Medical.
Rights and permissions
About this article
Cite this article
Rodés-Cabau, J. Transcatheter aortic valve implantation: current and future approaches. Nat Rev Cardiol 9, 15–29 (2012). https://doi.org/10.1038/nrcardio.2011.164
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2011.164
This article is cited by
-
Modifications in ocular microperfusion after transcatheter aortic valve implantation
Scientific Reports (2023)
-
A validated computational framework to predict outcomes in TAVI
Scientific Reports (2020)
-
Delirium is associated with higher mortality in transcatheter aortic valve replacement: systemic review and meta-analysis
Cardiovascular Intervention and Therapeutics (2020)
-
Prognostic impact of cancer history in patients undergoing transcatheter aortic valve implantation
Clinical Research in Cardiology (2020)
-
Predictive factors and long-term prognosis of transcatheter aortic valve implantation-associated endocarditis
Clinical Research in Cardiology (2020)