Key Points
-
The true incidence of obstructive coronary artery disease (CAD) among patients undergoing transcatheter aortic valve implantation (TAVI) is not known
-
Assessment of CAD using angiography only can overestimate the presence of myocardial ischaemia in patients before TAVI
-
Anatomical scoring criteria for CAD can improve the selection of high-risk patients undergoing TAVI
-
Coronary pressure-wire measurements using conventional algorithms before TAVI might underestimate myocardial ischaemia
-
Noninvasive stress testing can be used safely in patients before TAVI, but might overestimate myocardial ischaemia
-
Percutaneous coronary intervention after TAVI is still not widely practised, and only case reports are available
Abstract
Coronary artery disease (CAD) is common in patients with severe aortic stenosis undergoing transcatheter aortic valve implantation (TAVI), but its clinical relevance is controversial. At present, the optimal means of defining CAD in patients undergoing TAVI with respect to its prognostic implications and the assessment of myocardial ischaemia is not known. For this reason, the best treatment options are a matter for debate, and current guidelines do not recommend revascularization. As the indications for TAVI expand, the lack of any rigorous means of guiding coronary revascularization might negatively affect the clinical outcomes of future patients. In this Review, we summarize the methods of assessing CAD in TAVI populations, and the data on the safety and efficacy of percutaneous coronary intervention in patients undergoing TAVI. We discuss the putative effects of aortic stenosis on the functional assessment of CAD using pressure or flow wires or by noninvasive stress testing. We propose that a new, well-validated method of assessing CAD as a cause of myocardial ischaemia — which distinguishes it from myocardial infarction, previous revascularization, or non-flow-limiting disease — in patients with severe aortic stenosis is needed to guide revascularization in the current era of TAVI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Stefanini, G. G., Stortecky, S., Wenaweser, P. & Windecker, S. Coronary artery disease in patients undergoing TAVI: why, what, when and how to treat. EuroIntervention 10, U69–U75 (2014).
Khawaja, M. Z., Redwood, S. R. & Thomas, M. Coronary artery disease in patients undergoing TAVI — why not to treat. EuroIntervention 10, U76–U83 (2014).
Julius, B. K. et al. Angina pectoris in patients with aortic stenosis and normal coronary arteries: mechanisms and pathophysiological concepts. Circulation 95, 892–898 (1997).
Masson, J. B. et al. Impact of coronary artery disease on outcomes after transcatheter aortic valve implantation. Catheter. Cardiovasc. Interv. 76, 165–173 (2010).
Stefanini, G. G. et al. Coronary artery disease severity and aortic stenosis: clinical outcomes according to SYNTAX score in patients undergoing transcatheter aortic valve implantation Eur. Heart J. 35, 2530–2540 (2014).
Khawaja, M. Z. et al. The effect of coronary artery disease defined by quantitative coronary angiography and SYNTAX score upon outcome after transcatheter aortic valve implantation (TAVI) using the Edwards bioprosthesis. EuroIntervention 11, 450–455 (2015).
Van Mieghem, N. M. et al. Complete revascularization is not a prerequisite for success in current transcatheter aortic valve implantation practice. JACC Cardiovasc. Interv. 6, 867–875 (2013).
Leon, M. B. et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N. Engl. J. Med. 363, 1597–1607 (2010).
Smith, C. R. et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N. Engl. J. Med. 364, 2187–2198 (2011).
Chieffo, A. et al. Transcatheter aortic valve implantation with the Edwards SAPIEN versus the Medtronic CoreValve Revalving system devices: a multicenter collaborative study: the PRAGMATIC Plus Initiative (Pooled-RotterdAm-Milano-Toulouse In Collaboration). J. Am. Coll. Cardiol. 61, 830–836 (2013).
Abdel-Wahab, M. et al. Balloon-expandable versus self-expandable valves in patients undergoing transcatheter aortic valve replacement: the CHOICE randomized clinical trial. JAMA 311, 1503–1514 (2014).
Duncan, A. et al. Long-term outcomes after transcatheter aortic valve replacement in high-risk patients with severe aortic stenosis: the UK Transcatheter Aortic Valve Implantation Registry. JACC Cardiovasc. Interv. 8, 645–653 (2015).
Thielmann, M. et al. Prognostic value of preoperative cardiac troponin I in patients with non-ST-segment elevation acute coronary syndromes undergoing coronary artery bypass surgery. Chest 128, 3526–3536 (2005).
Etchells, E., Meade, M., Tomlinson, G. & Cook, D. Semi-quantitative dipyridamole myocardial stress perfusion imaging for cardiac risk assessment before noncardiac vascular surgery: a metaanalysis. J. Vasc. Surg. 36, 534–540 (2002).
Beach, J. M. et al. Coronary artery disease and outcomes of aortic valve replacement for severe aortic stenosis. J. Am. Coll. Cardiol. 61, 837–848 (2013).
Mullany, C. J. et al. Coronary artery disease and its management: influence on survival in patients undergoing aortic valve replacement. J. Am. Coll. Cardiol. 10, 66–72 (1987).
Lund, O., Nielsen, T. T., Pilegaard, H. K., Magnussen, K. & Knudsen, M. A. The influence of coronary artery disease and bypass grafting on early and late survival after valve replacement for aortic stenosis. J. Thorac. Cardiovasc. Surg. 100, 327–337 (1990).
Tjang, Y. S., van Hees, Y., Korfer, R., Grobbee, D. E. & van der Heijden, G. J. Predictors of mortality after aortic valve replacement. Eur. J. Cardiothorac. Surg. 32, 469–474 (2007).
Likosky, D. S. et al. Long-term survival of the very elderly undergoing aortic valve surgery. Circulation 120, S127–S133 (2009).
Iung, B. et al. Prognosis of valve replacement for aortic stenosis with or without coexisting coronary heart disease: a comparative study. J. Heart Valve Dis. 2, 430–439 (1993).
Svensson, L. G., Blackstone, E. H. & Cosgrove, D. M. 3rd Surgical options in young adults with aortic valve disease. Curr. Probl. Cardiol. 28, 417–480 (2003).
Dewey, T. M. et al. Effect of concomitant coronary artery disease on procedural and late outcomes of transcatheter aortic valve implantation. Ann. Thorac. Surg. 89, 758–767 (2010).
Greason, K. L. et al. Transcatheter versus surgical aortic valve replacement in patients with prior coronary artery bypass graft operation: a PARTNER trial subgroup analysis. Ann. Thorac. Surg. 98, 1–7 (2014).
Gilard, M. et al. Registry of transcatheter aortic-valve implantation in high-risk patients. N. Engl. J. Med. 366, 1705–1715 (2012).
Gautier, M. et al. Impact of coronary artery disease on indications for transcatheter aortic valve implantation and on procedural outcomes. EuroIntervention 7, 549–555 (2011).
Ludman, P. F. et al. Transcatheter aortic valve implantation in the United Kingdom: temporal trends, predictors of outcome, and 6-year follow-up: a report from the UK Transcatheter Aortic Valve Implantation (TAVI) Registry, 2007 to 2012. Circulation 131, 1181–1190 (2015).
Schymik, G. et al. European experience with the second-deneration Edwards SAPIEN XT transcatheter heart valve in patients with severe aortic stenosis: 1-year outcomes from the SOURCE XT Registry. JACC Cardiovasc. Interv. 8, 657–669 (2015).
Thomas, M. et al. Thirty-day results of the SAPIEN aortic Bioprosthesis European Outcome (SOURCE) Registry: a European registry of transcatheter aortic valve implantation using the Edwards SAPIEN valve. Circulation 122, 62–69 (2010).
Linke, A. et al. Treatment of aortic stenosis with a selfexpanding transcatheter valve: the International Multi-centre ADVANCE Study. Eur. Heart J. 35, 2672–2684 (2014).
Abdel-Wahab, M. et al. Comparison of outcomes in patients having isolated transcatheter aortic valve implantation versus combined with preprocedural percutaneous coronary intervention. Am. J. Cardiol. 109, 581–586 (2012).
Pasic, M. et al. Combined elective percutaneous coronary intervention and transapical transcatheter aortic valve implantation. Interact. Cardiovasc. Thorac. Surg. 14, 463–468 (2012).
Gasparetto, V. et al. Safety and effectiveness of a selective strategy for coronary artery revascularization before transcatheter aortic valve implantation. Catheter. Cardiovasc. Interv. 81, 376–383 (2013).
Abramowitz, Y. et al. Comparison of early and late outcomes of TAVI alone compared to TAVI plus PCI in aortic stenosis patients with and without coronary artery disease. Catheter. Cardiovasc. Interv. 83, 649–654 (2014).
Griese, D. P. et al. Concomitant coronary intervention is associated with poorer early and late clinical outcomes in selected elderly patients receiving transcatheter aortic valve implantation. Eur. J. Cardiothorac. Surg. 46, e1–e7 (2014).
Van Gameren, M. et al. Do we need separate risk stratification models for hospital mortality after heart valve surgery? Ann. Thorac. Surg. 85, 921–930 (2008).
Pijls, N. H. et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER study. J. Am. Coll. Cardiol. 49, 2105–2111 (2007).
Tonino, P. A. et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N. Engl. J. Med. 360, 213–224 (2009).
Prati, F. et al. Angiography alone versus angiography plus optical coherence tomography to guide decision-making during percutaneous coronary intervention: the Centro per la Lotta contro l'Infarto-Optimisation of Percutaneous Coronary Intervention (CLI-OPCI) study. EuroIntervention 8, 823–829 (2012).
Tu, S. et al. In vivo comparison of arterial lumen dimensions assessed by co-registered three-dimensional (3D) quantitative coronary angiography, intravascular ultrasound and optical coherence tomography. Int. J. Cardiovasc. Imaging 28, 1315–1327 (2012).
Villari, B. et al. Regression of coronary artery dimensions after successful aortic valve replacement. Circulation 85, 972–978 (1992).
O'Sullivan, C. J. et al. Clinical outcomes and revascularization strategies in patients with low-flow, low-gradient severe aortic valve stenosis according to the assigned treatment modality. JACC Cardiovasc. Interv. 8, 704–717 (2015).
Khawaja, M. Z., Wang, D., Pocock, S., Redwood, S. R. & Thomas, M. R. The percutaneous coronary intervention prior to transcatheter aortic valve implantation (ACTIVATION) trial: study protocol for a randomized controlled trial. Trials 15, 300 (2014).
Takashima, H. et al. Severity of morphological lesion complexity affects fractional flow reserve in intermediate coronary stenosis. J. Cardiol. 66, 239–245 (2015).
De Bruyne, B. et al. Fractional flow reserve-guided PCI for stable coronary artery disease. N. Engl. J. Med. 371, 1208–1217 (2014).
Rajappan, K. et al. Mechanisms of coronary microcirculatory dysfunction in patients with aortic stenosis and angiographically normal coronary arteries. Circulation 105, 470–476 (2002).
Dixon, J. A. & Spinale, F. G. Myocardial remodelling: cellular and extracellular events and targets. Annu. Rev. Physiol. 73, 47–68 (2011).
Choudhury, L. et al. Coronary vasodilator reserve in primary and secondary left ventricular hypertrophy: a study with positron emission tomography. Eur. Heart J. 18, 108–116 (1997).
Heusch, G. Alpha-adrenergic coronary vasoconstriction in humans. J. Am. Coll. Cardiol. 55, 1278 (2010).
Broyd, C. J. et al. Myocardial ischemia in aortic stenosis: insights from arterial pulse-wave dynamics after percutaneous aortic valve replacement. Trends Cardiovasc. Med. 23, 185–191 (2013).
Galiuto, L. et al. Impaired coronary and myocardial flow in severe aortic stenosis is associated with increased apoptosis: a transthoracic Doppler and myocardial contrast echocardiography study. Heart 92, 208–212 (2006).
Davies, J. E. et al. Arterial pulse wave dynamics after percutaneous aortic valve replacement: fall in coronary diastolic suction with increasing heart rate as a basis for angina symptoms in aortic stenosis. Circulation 124, 1565–1572 (2011).
Stähli, B. E., Maier, W., Corti, R., Lüscher, T. F. & Altwegg, L. A. Fractional flow reserve evaluation in patients considered for transfemoral transcatheter aortic valve implantation: a case series. Cardiology 123, 234–239 (2012).
Nijjer, S. S. et al. Improvement in coronary haemodynamics after percutaneous coronary intervention: assessment using instantaneous wave-free ratio. Heart 99, 1740–1748 (2013).
Sen, S. et al. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave-intensity analysis: results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) study. J. Am. Coll. Cardiol. 59, 1392–1402 (2012).
Wiegerinck, E. M. et al. Impact of aortic valve stenosis on coronary hemodynamics and the instantaneous effect of transcatheter aortic valve implantation. Circ. Cardiovasc. Interv. 8, e002443 (2015).
Davies, J. E. et al. Evidence of a dominant backward-propagating 'suction' wave responsible for diastolic coronary filling in humans, attenuated in left ventricular hypertrophy. Circulation 113, 1768–1778 (2006).
Bountioukos, M. et al. Safety of dobutamine stress echocardiography in patients with aortic stenosis. J. Heart Valve Dis. 12, 441–446 (2003).
Baroni, M. et al. Mechanisms of regional ischaemic changes during dipyridamole echocardiography in patients with severe aortic valve stenosis and normal coronary arteries. Heart 75, 492–497 (1996).
Zajarias, A., Eltchaninoff, H. & Cribier, A. Successful coronary intervention after percutaneous aortic valve replacement. Catheter. Cardiovasc. Interv. 69, 522–524 (2007).
Greenberg, G. & Kornowski, R. Coronary angioplasty after self-expandable transcatheter aortic valve implantation. J. Invasive Cardiol. 25, 361–363 (2013).
Ribeiro, H. B. et al. Predictive factors, management, and clinical outcomes of coronary obstruction following transcatheter aortic valve implantation: insights from a large multicenter registry. J. Am. Coll. Cardiol. 62, 1552–1562 (2013).
Mohr, F. W. et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet 381, 629–638 (2013).
Adams, D. H. et al. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N. Engl. J. Med. 370, 1790–1798 (2014).
Babaliaros, V. et al. 30 day outcomes from the PARTNER II trial for transapical and transfemoral 29mm TAVR in inoperable patients with the Edwards Sapien XT [abstract]. J. Am. Coll. Cardiol. 63, A1687 (2014).
Mack, M. J. et al. 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet 385, 2477–2484 (2015).
Kapadia, S. R. et al. 5-year outcomes of transcatheter aortic valve replacement compared with standard treatment for patients with inoperable aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet 385, 2485–2491 (2015).
Reardon, M. J. et al. 2-year outcomes in patients undergoing surgical or self-expanding transcatheter aortic valve replacement. J. Am. Coll. Cardiol. 66, 113–121 (2015).
Penkalla, A. et al. Transcatheter aortic valve implantation combined with elective coronary artery stenting: a simultaneous approach Eur. J. Cardiothorac. Surg. 47, 1083–1089 (2015).
Cremer, P. C. et al. Stress positron emission tomography is safe and can guide coronary revascularization in high-risk patients being considered for transcatheter aortic valve replacement. J. Nucl. Cardiol. 21, 1001–1010 (2014).
Burgstahler, C. et al. Adenosine stress first pass perfusion for the detection of coronary artery disease in patients with aortic stenosis: a feasibility study. Int. J. Cardiovasc. Imaging 24, 195–200 (2008).
Patsilinakos, S. P. et al. Adenosine stress myocardial perfusion tomographic imaging in patients with significant aortic stenosis. J. Nucl. Cardiol. 11, 20–25 (2004).
Demirkol, M. O., Yaymaci, B., Debeş, H., Başaran, Y. & Turan, F. Dipyridamole myocardial perfusion tomography in patients with severe aortic stenosis. Cardiology 97, 37–42 (2002).
Patsilinakos, S. P. et al. Detection of coronary artery disease in patients with severe aortic stenosis with noninvasive methods. Angiology 50, 309–317 (1999).
Author information
Authors and Affiliations
Contributions
E.D., P.H., and R.B. researched data for the article and wrote the manuscript. All the authors contributed substantially to discussion of content, and reviewing and editing the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
I.M. receives consulting fees from Boston Scientific. The other authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Danson, E., Hansen, P., Sen, S. et al. Assessment, treatment, and prognostic implications of CAD in patients undergoing TAVI. Nat Rev Cardiol 13, 276–285 (2016). https://doi.org/10.1038/nrcardio.2016.9
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2016.9
This article is cited by
-
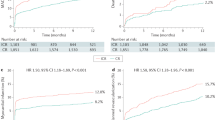
Impact of extent of coronary artery disease and percutaneous revascularization assessed by the SYNTAX score on outcomes following transcatheter aortic valve replacement
BMC Cardiovascular Disorders (2021)
-
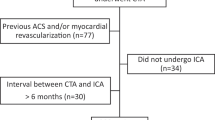
Computed Tomography Angiography for the Diagnosis of Coronary Artery Disease Among Patients Undergoing Transcatheter Aortic Valve Implantation
Journal of Cardiovascular Translational Research (2021)
-
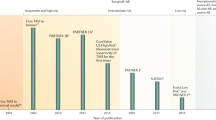
The Influence of Aortic Valve Obstruction on the Hyperemic Intracoronary Physiology: Difference Between Resting Pd/Pa and FFR in Aortic Stenosis
Journal of Cardiovascular Translational Research (2019)
-
A numerical study of the hemodynamic effect of the aortic valve on coronary flow
Biomechanics and Modeling in Mechanobiology (2018)
-
Timing and Outcomes of PCI in the TAVR Era
Current Treatment Options in Cardiovascular Medicine (2018)